SEPSIS Patway
RECOGNISING SEPSIS
The clinical diagnosis of sepsis may be obvious, such as when someone presents to the emergency department with community acquired pneumonia or a perforated viscus; however, in other circumstances and when onset is more insidious the diagnosis of sepsis is often missed.
Early diagnosis and prompt treatment is essential as each hours delay in administering antibiotics increases risk of death by close to 8% (6). Compliance with international guidelines for the management of sepsis remains low even in countries where the guidelines have been embraced (7;8).
Sepsis occurs as a result of infection, signs suggestive of infection include:
- Fever and/or rigors
- Hypothermia
- Cough, increased sputum production or dyspnoea
- Abdominal pain or distension
- Dysuria, urinary frequency, odour
- New onset confusion or decreased level of consciousness
- Recent surgery or invasive procedure with cellulitis or wound infection
- Line associated redness/swelling/pain
- Painful swollen joint
- Meningism
Infection confirmed or suspected plus:
- Temperature > 38.3C or < 36C (normal temperature does not exclude sepsis)
- Respiratory rate > 20 / minute
- Heart rate > 90/minute
- Acute confusion or decreased level of consciousness
- Hyperglycemia (blood glucose > 7.7 mmol/L in patient without diabetes)
- Oliguria (urine output less than 0.5 mL/kg/hour)
The clinical diagnosis of sepsis may be obvious, such as when someone presents to the emergency department with community acquired pneumonia or a perforated viscus; however, in other circumstances and when onset is more insidious the diagnosis of sepsis is often missed.
Early diagnosis and prompt treatment is essential as each hours delay in administering antibiotics increases risk of death by close to 8% (6). Compliance with international guidelines for the management of sepsis remains low even in countries where the guidelines have been embraced (7;8).
Sepsis occurs as a result of infection, signs suggestive of infection include:
- Fever and/or rigors
- Hypothermia
- Cough, increased sputum production or dyspnoea
- Abdominal pain or distension
- Dysuria, urinary frequency, odour
- New onset confusion or decreased level of consciousness
- Recent surgery or invasive procedure with cellulitis or wound infection
- Line associated redness/swelling/pain
- Painful swollen joint
- Meningism
Infection confirmed or suspected plus:
- Temperature > 38.3C or < 36C (normal temperature does not exclude sepsis)
- Respiratory rate > 20 / minute
- Heart rate > 90/minute
- Acute confusion or decreased level of consciousness
- Hyperglycemia (blood glucose > 7.7 mmol/L in patient without diabetes)
- Oliguria (urine output less than 0.5 mL/kg/hour)
SIGNS SUGGESTIVE OF SEPTIC SHOCK
Infection confirmed or suspected plus:
- Mottled or cold peripheries
- Capillary refill time > 3seconds
- Systolic BP < 90 mmHg or MAP < 60 mmHg
- Purpuric rash
- Arterial or venous lactate > 2 mmol/L
- Oliguria (urine output less than 0.5 mL/kg/hour
Infection confirmed or suspected plus:
- Mottled or cold peripheries
- Capillary refill time > 3seconds
- Systolic BP < 90 mmHg or MAP < 60 mmHg
- Purpuric rash
- Arterial or venous lactate > 2 mmol/L
- Oliguria (urine output less than 0.5 mL/kg/hour
IMMEDIATE MANAGEMENT
- Assess for airway patency and administer oxygen
- Obtain IV access, blood cultures and baseline blood tests (including lactate)
- Other diagnostic samples if they will not delay antibiotic treatment (e.g. sputum, urine, pus)
- Prescribe and administer antibiotics (should be administered in first hour)
- IV fluid bolus if patient showing signs of shock/hypoperfusion – 250-500 mL crystalloid (e.g. N/Saline, Hartmanns or Plasmalyte) repeated as required.
- Seek senior help and transfer to ICU if transient or no response to treatment
- Examination for source of sepsis if not already clear
- Monitor fluid balance and urine output
Follow a patway
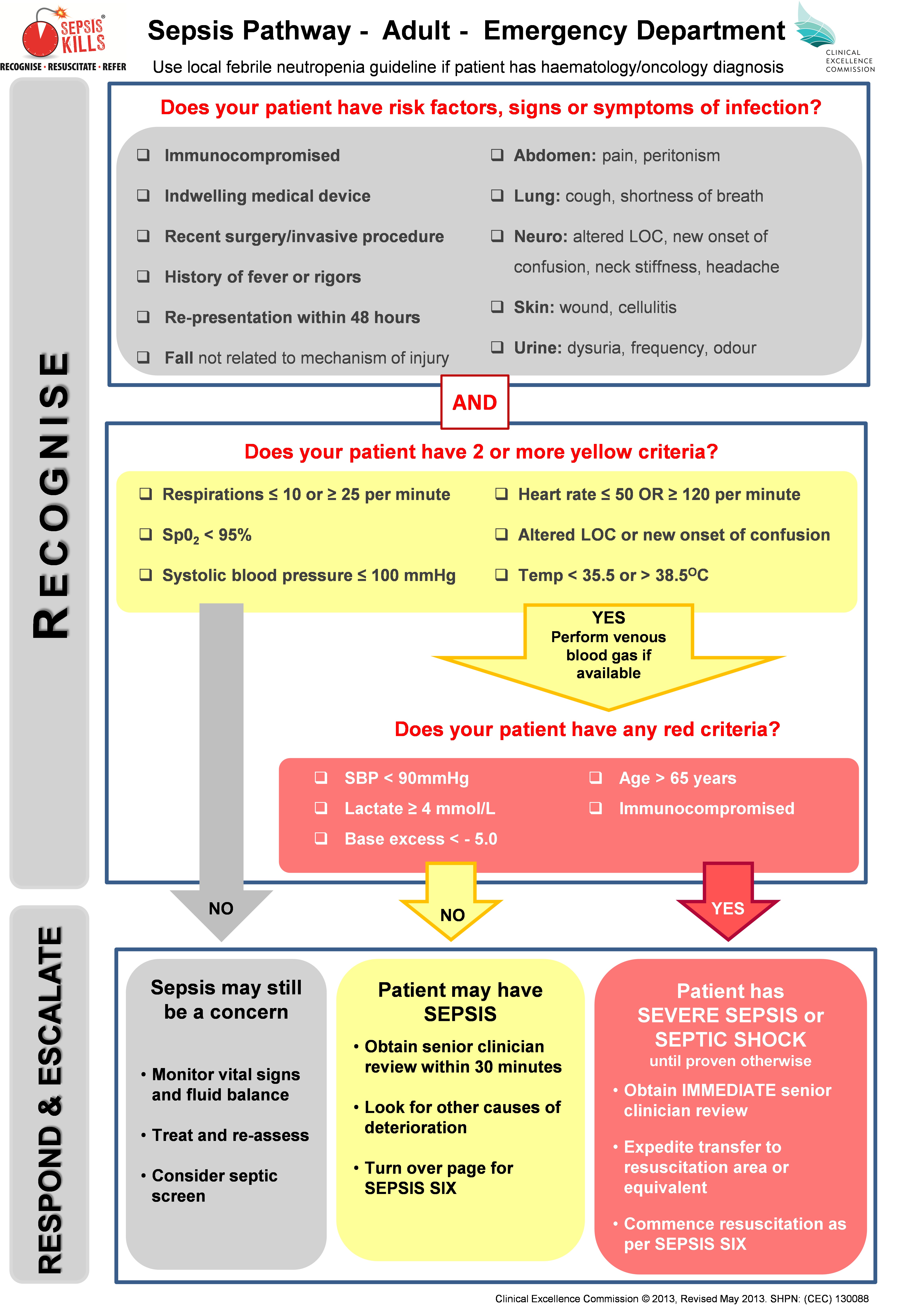
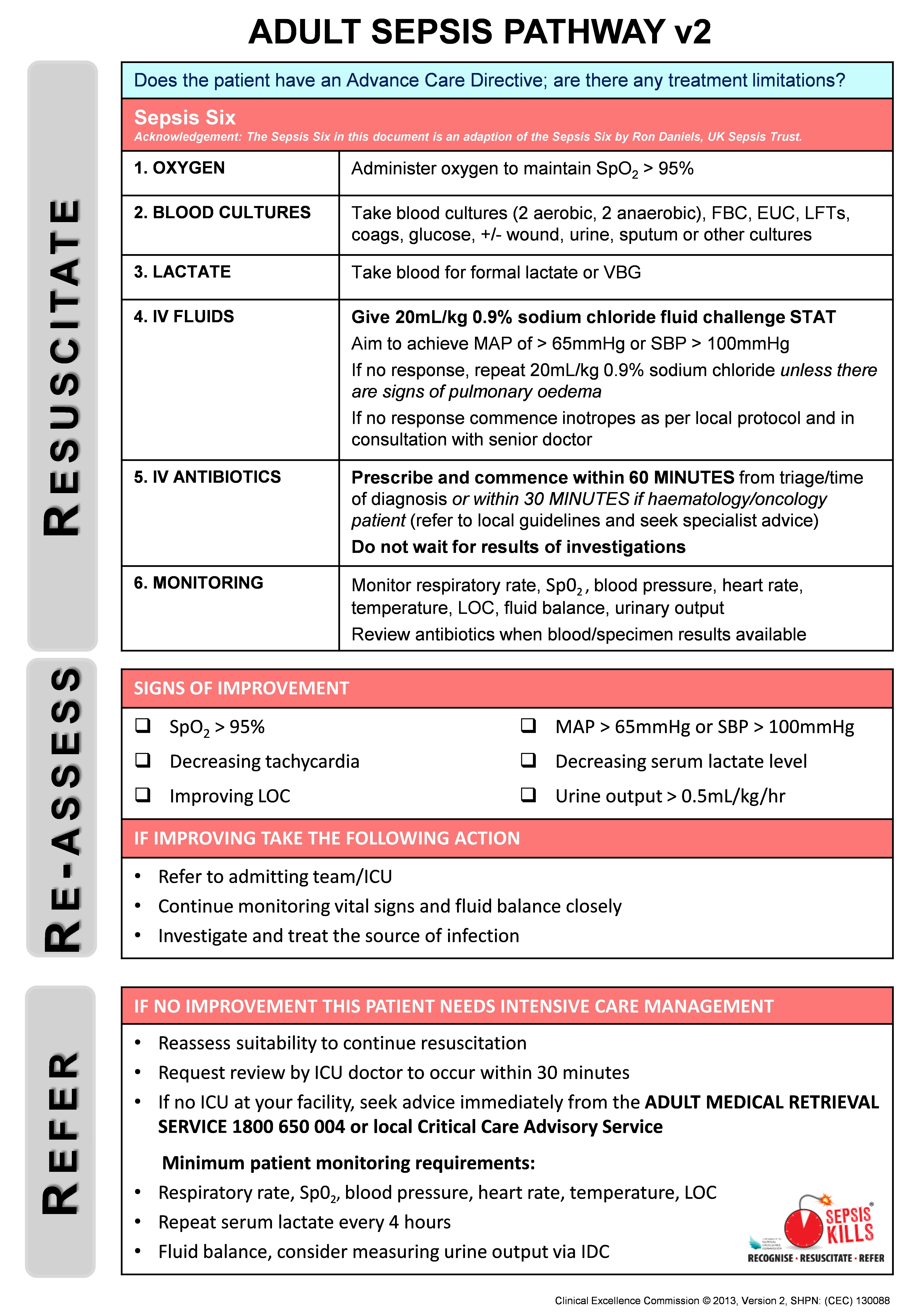
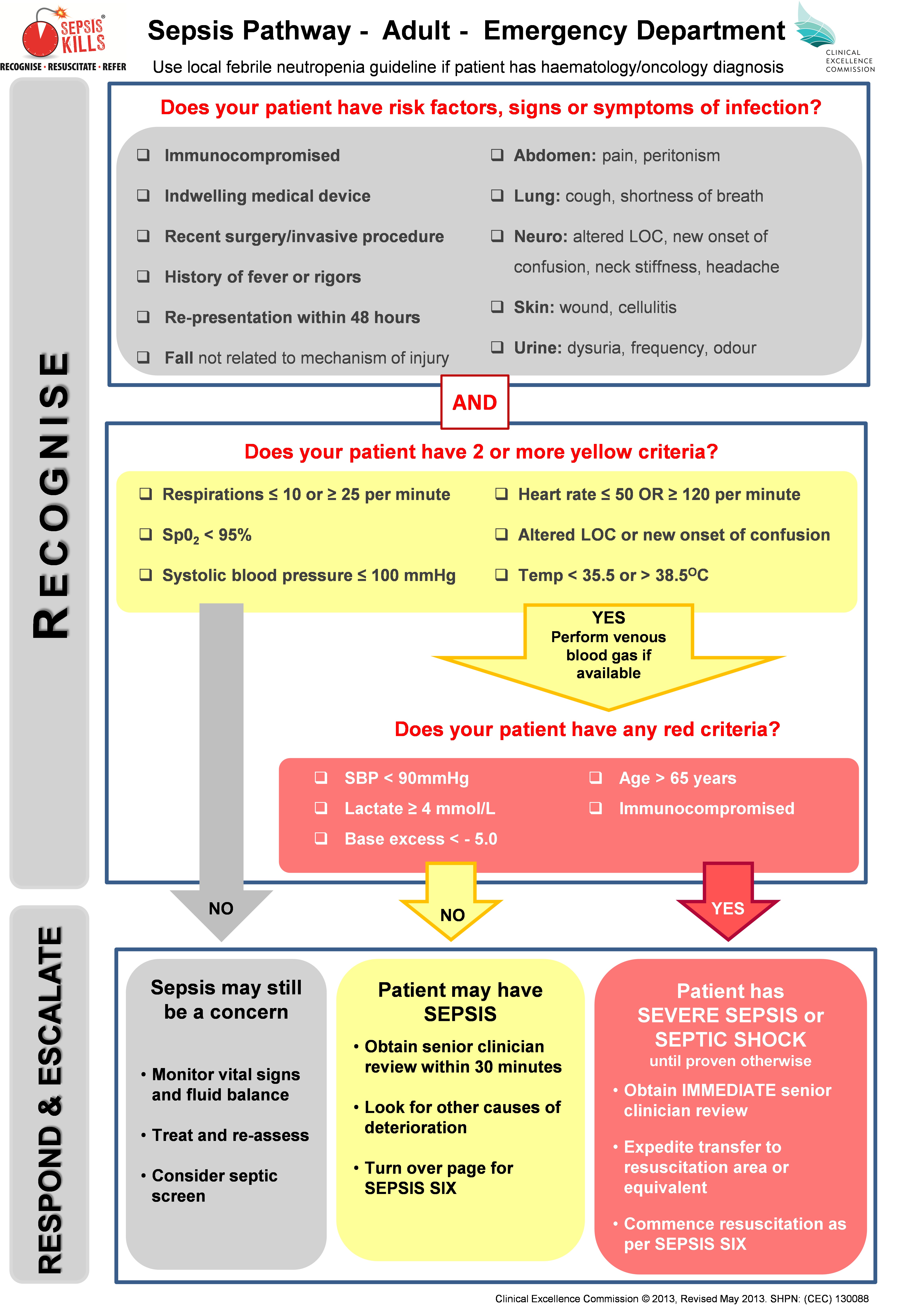
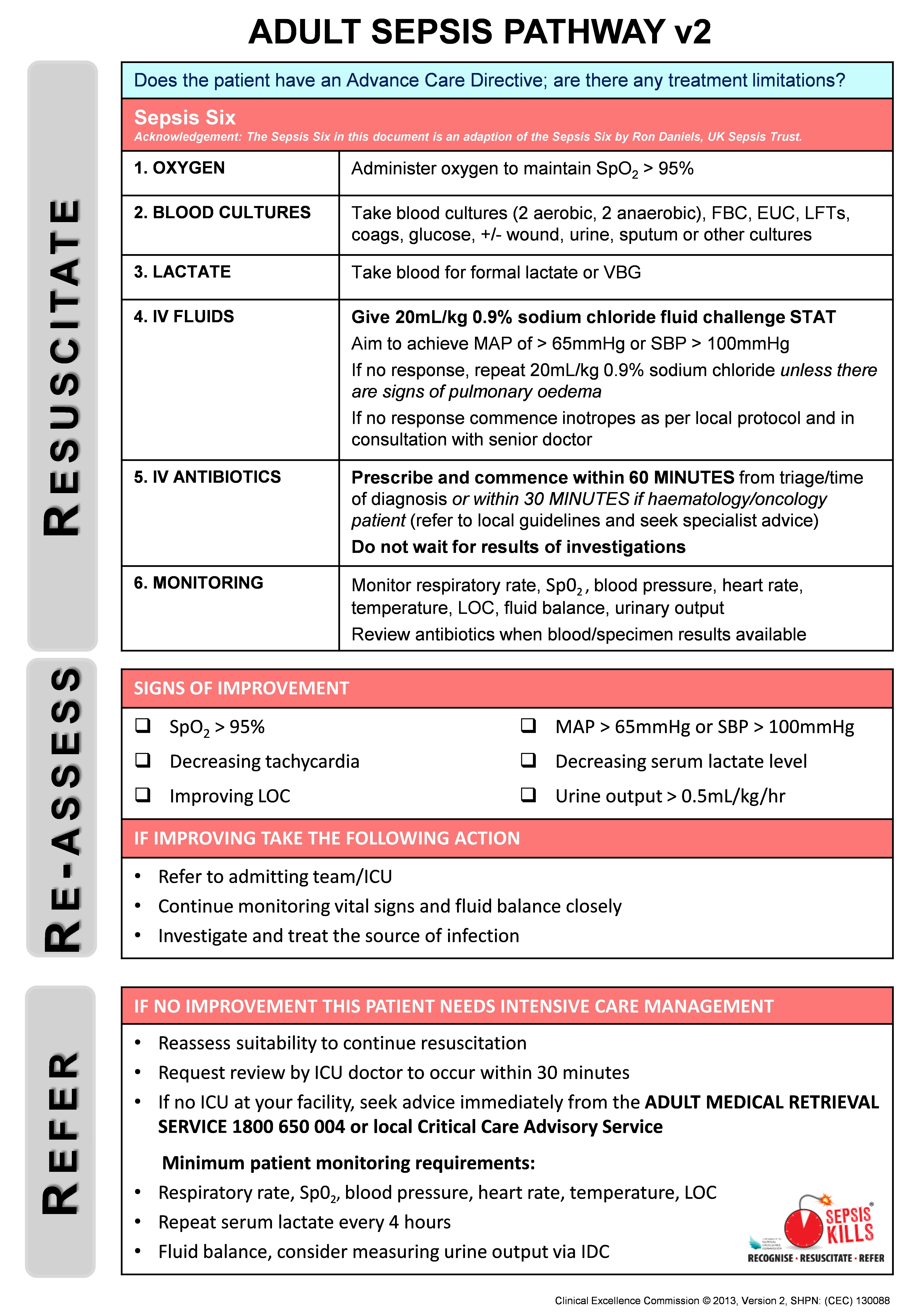
Table 1
Surviving Sepsis Campaign one-hour bundle.
Bundle element Grade of recommendation and level of evidence Measure lactate. Re-measure if initial lactate > 2 mmol/L. Weak recommendation. Low quality of evidence. Obtain blood cultures prior to administration of antibiotics. Best practice statement. Administer broad-spectrum antibiotics. Strong recommendation. Moderate quality of evidence. Rapidly administer 30 ml/kg crystalloid for hypotension or lactate ≥4 mmol/L. Strong recommendation. Low quality of evidence. Apply vasopressors if patient is hypotensive during or after fluid resuscitation to maintain MAP ≥ 65 mm Hg. Strong recommendation. Moderate quality of evidence.
mmol/L, millimoles per liter; ml/kg, milliliters per kilogram; mmHg, millimeters of mercury; MAP, mean arterial pressure.
Surviving Sepsis Campaign one-hour bundle.
| Bundle element | Grade of recommendation and level of evidence |
|---|---|
| Measure lactate. Re-measure if initial lactate > 2 mmol/L. | Weak recommendation. Low quality of evidence. |
| Obtain blood cultures prior to administration of antibiotics. | Best practice statement. |
| Administer broad-spectrum antibiotics. | Strong recommendation. Moderate quality of evidence. |
| Rapidly administer 30 ml/kg crystalloid for hypotension or lactate ≥4 mmol/L. | Strong recommendation. Low quality of evidence. |
| Apply vasopressors if patient is hypotensive during or after fluid resuscitation to maintain MAP ≥ 65 mm Hg. | Strong recommendation. Moderate quality of evidence. |
mmol/L, millimoles per liter; ml/kg, milliliters per kilogram; mmHg, millimeters of mercury; MAP, mean arterial pressure.
Table 2
Various definitions for sepsis spectral illnesses.
Comentários
Enviar um comentário