Brain Herniation — Types, Symptoms and Radiology
Image: “Unusual tonsillar herniation in meningeal melanocytoma: a case report.” By Samimi K, Gharib MH, Rezaei-Kalantari K, Jafari M. License: CC BY 3.0
Introduction
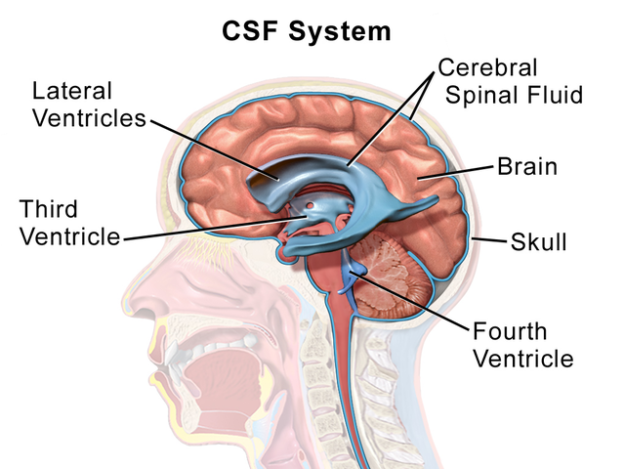
The cranium or cranial vault is anatomically considered as a box, formed by bones. The cranial vault is fixed and non-expandible. It contains the brain tissue, cerebrospinal fluid (CSF) and blood vessels, all of which occupy accurate proportions within the cranium. There is a certain amount of pressure that is exerted by the cranial vault on the internal structures i.e. brain parenchymal tissue, CSF and the blood vessels. This pressure is known as the intracranial pressure (ICP). At rest, in a normal adult, this ICP is 7 – 15 mmHg. It continuously changes due to various physical activities such as coughing, exercise, any other strenuous activity or even due to the respiratory cycle.
The brain parenchyma makes up 80% of the volume, while CSF and blood vessels each account for 10% of volume. All these three structures, namely the brain tissue, cerebrospinal fluid and blood vessels have a unique and fixed relation, because of which even the slightest change in the volume of any of these structures leads to an increase in the intracranial pressure. There are many causes that lead to an increase in the intracranial pressure and these are discussed below. This unique relation within the internal structures of the cranium is well explained by the Monro-Kellie doctrine.
It is important to know that, according to the Monro-Kellie doctrine, there is the existence of an intracranial pressure and there is a self-regulating mechanism which allows the maintenance of a normal intracranial pressure when any injury occurs inside the cranium. For example, if a person suffers an intracranial hemorrhage, the intracranial pressure increases and must be compensated with a decrease of cerebrospinal fluid and venous blood to maintain the total intracranial pressure between 100 – 120 ml.
Etiology of Increased ICP
Intracranial hypertension is defined as a sustained (> 5 min) elevation of ICP of > 20 mmHg.
Herniation syndromes occur as a result of intracranial compartmental pressure gradients. Because of these, there is displacement of the parenchymal tissues that lead to compression or displacement of the cranial nerves, brainstem or cerebral vasculature. There are edema and resultant deterioration in patientcompliance as a result of ischemia or infarction from vascular compression.
When the self-regulation capacity of the cranium is exceeded and the intracranial pressure exceeds the normal limits, the brain tissue is displaced (because of mass effect) from its normal location to adjacent spaces, which is denominated intracranial herniation or brain herniation.
- Mass effect: space-occupying lesions such as brain tumor, brain edema, abscess, contusion, and hematoma lead to deformation of adjacent brain structures.
- Various medical conditions can lead to generalized swelling or edema of the brain. These are an acute liver failure, hypertensive encephalopathy, the state of ischemic-anoxia etc.
- There can be an increase in the venous pressure leading to increase in the ICP. Heart failure, obstruction of superior mediastinal or jugular veins or venous sinus thrombosis can lead to increased venous pressure.
- Certain conditions cause obstruction of the CSF flow, such as hydrocephalus, extensive meningeal disease etc.
Classification of Brain Herniation
Brain herniation syndromes are classified into the following types according to the structure through which the tissue was herniated: subfalcine, transtentorial and cerebellar tonsillar.
1. Subfalcine herniation or cingulate gyrus herniation (also known as midline shift)
It is thought to be the most common of the three types of herniation. It refers to the cingulate gyrus displacement under the falx cerebri due to an increase in pressure in any of the cerebral hemispheres. This ultimately leads to widespread infarction involving the frontal and parietal lobes due to compression of the major blood vessel, i.e. the anterior cerebral artery.
In this type of herniation, there are no associated specific clinical signs and symptoms and, when seen over a long duration, the effects are less severe as compared to other types of herniation. Clinically, the patients present with a decreased level of consciousness that is directly proportional to the degree of midline shift.
2. Transtentorial herniation (also known as downward, central herniation or uncal herniation)
When there is edema of the brain, the cerebral hemispheres are enlarged; thus, the brain parenchymal tissue that is present in the supratentorial compartment is displaced caudally into the infratentorial compartment.
There are various causes that give rise to this displacement. These include supratentorial mass lesions, diffuse edema of the brain (which is seen in patients with traumatic injury to the brain), focal brain edema or acute hydrocephalus.
The downward displacement of brain tissue causes compression of certain vital structures, i.e. the 3rd cranial nerve, the upper brainstem, as well as the cerebral peduncles. Compression of the caudal cerebral artery causes ischemia and infarction of the occipital lobe of the brain. In some cases, distortion or traction of the superior portion of the basilar artery is also seen. Clinically, patients are usually in a state of coma. There is ipsilateral dilation of the pupil (mydriasis) due to stretching of the oculomotor nerve. Parinaud’s syndrome is present, i.e. failure to gaze upwards, mid-dilated or pseudo-Argyll Robertson pupils, eyelid retraction and conjugate down gaze (sun-setting sign). Also, in many patients, diabetes insipidus is present.
3. Tonsillar herniation
This occurs when downward pressure forces the cerebellar tonsils into the foramen magnum. When pushed in a downward direction, the cerebellar tonsils cause compression of the medulla oblongata and the upper cervical spinal cord. The clinical features were seen are coma, apnea, hypertension and neck stiffness.
Image: “Shows six types of brain herniation: Supratentorial herniation Uncal Central (transtentorial) Cingulate (subfalcine) Transcalvarial Infratentorial herniation Upward (upward cerebellar or upward transtentorial) Tonsillar (downward cerebellar).” By Delldot derivative work: RupertMillard. License: CC BY-SA 3.0
Symptoms of Brain Herniation
The symptoms of brain herniation differ according to its cause. In non-traumatic cases, there can be a persistent headache that can lead to nocturnal awakening. A headache is usually localized and its frequency, as well as severity, can gradually increase. There can be a worsening of a headache during coughing, micturition or defecation.
In the case of traumatic head injury, the main features of head injury are seen along with supplementary features that are the presence of a low level of consciousness or unconsciousness, abnormalities in the vital parameters, visual changes and unbearable pain that waxes and wanes.
The presence of a neurocutaneous syndrome, macrocephaly, hormonal abnormalities, lethargy and/or personality change are risk factors for the development of an intracranial pathology and thus must be supervised regularly. Certain other factors, such as constant vomiting, abnormalities in growth patterns, focal neurologic deficit and nuchal rigidity, could be presenting symptoms of an underlying pathology.
There can be early signs of herniation and late signs, too. The early signs include decreased level of consciousness, confusion, difficulty with memory and thinking abilities, restlessness and lethargy. There is deterioration of motor function, along with papillary dysfunction and vision changes. There is the presence of a persistent headache. Certain personality changes could also be seen. Finally, there is a decreasing Glasgow coma score.
Amongst the late signs, if papilledema is present, brain herniation is a confirmatory diagnosis. The pupils are dilated and do not react to light. There is a further decrease in the level of consciousness leading to a stuporous or comatose state. The other features are bradycardia, hyperthermia and progressive hemiplegia.
Radiographic Features
Initial resuscitative measures, hemodynamic stabilization of the patient, securing the airway, circulation, and respiratory systems of the patient and early hyperosmolar therapy should be performed before a cranial computed tomography (CT) scan is performed.
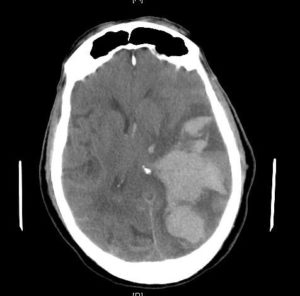
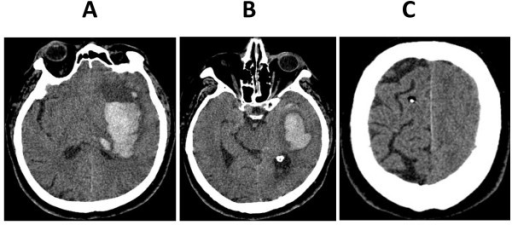
Imaging is essential to find the underlying cause for the elevated ICP. Generally, computed tomography is used to rule out the lesions that cause a mass effect, such as a tumor or edema due to hemorrhage. It is also helpful in the demonstration of physical findings, such as midline shift, lateral displacement of midbrain etc.
CT is preferred over magnetic resonance imaging due to its wide availability and speed of imaging.
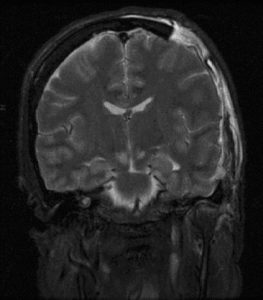
Imaging of cases with subfalcine herniation shows a shift in the septum pellucidum at the midline. There is effacement of sulci and ventricle on the affected side. There is hydrocephalus on the affected side as well.
In the case of transtentorial herniation, if it is central, there is the total obliteration of the basal subarachnoid cisterns and small lateral ventricles suggestive of brain edema. There is an increase in the sagittal diameter of the brain stem and the basilar artery is displaced inferiorly.
In the case of tonsillar herniation, the midbrain is effaced and displaced laterally along with effacement of suprasellar cisterns. The uncus and medial temporal lobe are displaced medially.
Image: “CT scan images after clinical signs of brain herniation developed. (A) Basal ganglia hemorrhage with perifocal edema. (B) Left-sided transtentorial herniation of the parahippocampal gyrus. (C) Edema of the left hemisphere with normally appearing right hemisphere.” By Dahlqvist MB, Andres RH, Raabe A, Jakob SM, Takala J, Dünser MW: Brain herniation in a patient with apparently normal intracranial pressure: a case report. License: CC-BY 2.0
Treatment of Brain Herniation: A General Approach
A correct diagnosis of the type of herniation and its underlying etiology are important parameters in its treatment as it helps in taking definitive steps that reduce the chances of the herniation entering into other compartments and its further complications. Thus, it is very important to know all the general measures if a brain herniation is suspected so that prompt intervention can be instituted.
Among the general measures of treatment, the most important include a constant control of vital signs, maintaining the head of the bed elevated to more than 45° and avoiding neck compression and using (if needed) an endotracheal tube (ETT) to secure the airway.
Image: “Diagram of an endotracheal tube that has been inserted into the airway.” By PhilippN – Modification of http://commons.wikimedia.org/wiki/Image:Endotracheal_tube_inserted.png. License: Public Domain
A high CO2 pressure (between 25 and 30 mmHg) Diagram of an inserted endotracheal tube to induce hyperventilation of the patient and increase vasoconstriction. Also, an adequate supply of oxygen must be maintained to minimize vasodilation.
Mannitol infusion in a dose of 2 g/kg (if it is not possible to use Lasix) helps to reduce the elevated intracranial pressure, as it decreases cerebral edema. A 30 cc bolus of hypertonic saline serum can be given. If the need arises, in order to decrease cerebral metabolism, the patient is sedated.
Image: “Medical equipment, focusing on External Ventricular Drain. Drain is leveled 4 cm above the external auditory meatus. CSF in drain is bloody from a subarachnoid hemorrhage due to a spontaneous ruptured aneurysm.” By Rmosler2100. License: CC BY-SA 3.0
An external ventricular drain (EVD) is instituted to decrease the cerebrospinal fluid amount and, in effect, the intracranial pressure.
It is essential to find and eliminate the injury responsible for the mass effect. In the case of a tumor, it is important to use intravenous steroids to decrease its size as much as possible. If the injury corresponds to a hematoma or abscess, it must be drained as soon as possible (decompressive craniectomy).
Finally, if the intracranial mass is a tumor, it can be diagnosed using advanced imaging techniques i.e. MRI and CT. The tumor mass must be aggressively treated and removed immediately after diagnosis to prevent further complications and morbidity.
In children, the basic treatment is decided to depend upon the clinical presentation of the child and the cause of increased ICP. In any case, it must be made sure that proper airway has been established. Also, two important factors that have to be constantly supervised are the blood pressure and ventilation of the child which must be maintained at normal. There is a risk of cerebral ischemia if the blood pressure is not maintained. Also, sufficient ventilation is necessary as it does not allow vasodilation which takes place as a result of hypercapnia. In accordance with the standard Pediatric Advanced Life Support (PALS), primarily the cardiopulmonary status of the child must be stabilized. Once the child is stabilized, further investigations, such as advanced imaging (head CT without contrast), must ensue.
In certain cases, wherein children have an elevated ICP, endotracheal intubation is a must; indications include refractory hypoxia, hypoventilation or a loss of airway protective reflexes. In acute herniation, endotracheal intubation is necessary as controlled hyperventilation is required and resuscitation medications can also be administered endotracheally.
Treatment of Brain Herniation Per the Emergency Neurological Life Support Guidelines
The emergency neurological life support (ENLS) guidelines are helpful in managing a patient with brain herniation as they can classify the treatment plan into four tiers.
Tier 0:
- Brain-code resuscitation is initiated.
- Assessment of circulation, airway patency and ventilation must be carried out.
- The head of the bed should be elevated to more than 30 degrees.
- Tracheal suctioning should be minimized.
- Normalize body’s temperature.
- Hyperosmotic fluids such as hyperosmotic saline should be used during resuscitation.
- High-dose corticosteroid therapy is started for patients with vasogenic brain edema.
- Once the patient is stabilized, non-contrast cranial CT should be performed.
Tier 1: Initiate only if Tier 0 standard measures do not correct ICP and brain herniation.
- Hyperosmolar therapy with mannitol or hypertonic saline is initiated.
- Brief course, less than 2 hours in duration, of induced hypo-capnia is tried: PaCO2 between 30 and 35 mmHg.
- If the patient does not improve, consider decompressive surgery.
- If surgery is not possible, move to Tier 2 treatments. Moreover, consider repeating the cranial CT scan if you see a worsening in the patient’s condition.
Tier 2:
- Consider an induced state of hypernatremia, but sodium levels should not be above 160 mmol/L.
- Propofol sedation is recommended in this tier.
- If Tier 2 measures do not correct the state of ICP, rescue decompressive surgery should be considered.
- If the patient is not a surgical candidate, move to Tier 3 interventions.
Tier 3: Consider only if Tier 2 interventions fail and rescue decompressive surgery is not an option.
- Consider the administration of pentobarbital.
- Continuous electroencephalographic monitoring is indicated while the patient is receiving pentobarbital.
- Induce a status of moderate hypothermia (target core temperature between 32 and 34 C).
- The induction of a state of moderate hypo-capnia with a PaCO2 between 25 and 35 mmHg.
- Hyperventilation should not be attempted for a duration above 6 hours.
Decompressive Surgery
Decompressive surgical interventions include:
- The placement of a ventricular drain.
- The evacuation of an epidural hematoma in patients with traumatic brain injury if it is the cause of brain herniation.
- Resection of the intracerebral lesion that is causing the mass effect that is responsible for brain herniation.
- Removal of brain parenchyma.
- Unilateral or bilateral craniectomy.
A rescue decompressive surgery usually means performing a decompressive craniectomy. It is usually required in patients with diffuse brain swelling due to traumatic brain injury who usually do not respond to Tier 0 to 2 interventions.
Conclusion
Cerebral herniation can be the result of different injuries that cause an increase in the intracranial pressure and exceed the brain’s auto-compensatory mechanisms. In any case, treatment should be instituted as early as possible. This is helpful for the prevention of the impending complications. The symptoms of different types of cerebral herniation are different and are indicative of the possible brain structure that has received the trauma leading to change in its position or compression. Thus, careful observation of symptoms helps in early diagnosis and treatment.





Comentários
Enviar um comentário