Atrial Flutter — Symptoms and Diagnosis
Table of Contents
- Definition of Atrial Flutter
- Epidemiology of Atrial Flutter
- Etiology of Atrial Flutter
- Pathology and Pathophysiology of Atrial Flutter
- Symptoms of Atrial Flutter
- Diagnosis of Atrial Flutter
- Differential Diagnoses of Atrial Flutter
- Therapy of Atrial Flutter
- Progression and Prognosis of Atrial Flutter
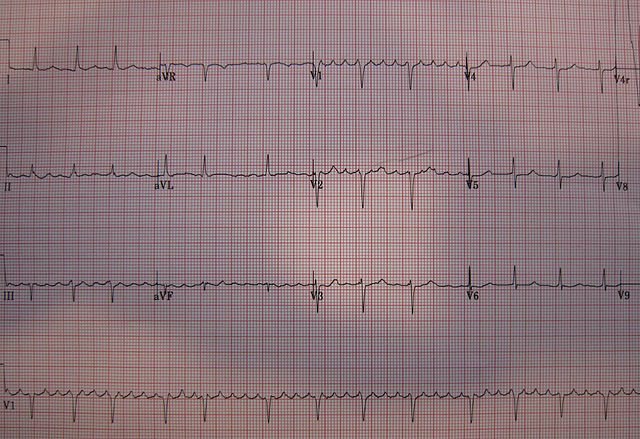
Image: “A 12 lead ECG showing atrial flutter” by James Heilman, MD. License: CC BY-SA 3.0
Definition of Atrial Flutter
Atrial flutter as supraventricular tachycardia
Atrial flutter is defined as a supraventricular tachycardia with an atrial origin that meets two requirements:
- Atrial heart rate between 240–400 beats per minute
- AV node conduction block
Additionally, it is characterized as a sawtooth pattern on ECG in leads II, III, and aVF. The QRS complexes will be narrow because its ectopic signal originates in the atrium. The ventricular heart rate will be constant, elevated above 100 bpm, and is considered a regularly irregular rhythm.
It is important to note that the atrial heart rate seen in atrial flutter is different from the ventricular heart rate. One of every two or three depolarization signals may pass through the AV node. A 2:1 or 3:1 ratio of P waves to QRS complexes are commonly seen on ECG. A patient may have an atrial heartbeat of 300 beats per minute but a ventricular heart rate of only 150 beats per minute. In this situation, the heart rate would be reported as “Atrial flutter with a heart rate of 150 beats per minute”.
Image: “A 12 lead ECG showing atrial flutter” by James Heilman, MD. License: CC BY-SA 3.0
The most common symptoms are palpitations and those symptoms associated with low cardiac output: fatigue, dyspnea, and chest pain. Syncope and congestive heart failure are also possible.
There are two types of atrial flutter:
- Type 1 – common or “typical” atrial flutter: has a reentrant loop type arrhythmia around the tricuspid valve and has an atrial rate of 240–340 beats per minute. Type 1 atrial flutter produces the characteristic sawtooth pattern in leads II, III, and aVF on ECG.
- Type 2 – atypical flutter: has an abnormal reentrant loop type arrhythmia and a much higher atrial rate at 340–440 beats per minute.
Epidemiology of Atrial Flutter
Spread of atrial flutter
Atrial flutter is less common than atrial fibrillation. Atrial flutter is 2.5 times more common in men compared to women and is more common in the elderly with an average age of onset is 64 years.
Etiology of Atrial Flutter
Causes of atrial flutter
A variety of cardiac and pulmonary diseases may result in atrial flutter. Any heart disease that results in inflammation or alteration to the structure of the heart may cause atrial flutter including cardiomyopathy, congenital heart defects, rheumatic disease, and pericarditis. About 1/3 of patients with atrial flutter may suffer from no other cardiovascular diseases at all; however, about 1/3 suffer from coronary artery disease (angina and myocardial infarction), and another 1/3 suffer from hypertension. Other conditions include:
- COPD
- Pulmonary Embolism
- Electrolyte imbalance
- Digitalis toxicity
- Hyperthyroidism
Heart structural defects (scar formation, ablation) and inflammation after surgery may also result in atrial flutter. Pulmonary vein isolation to correct atrial fibrillation is also a risk factor.
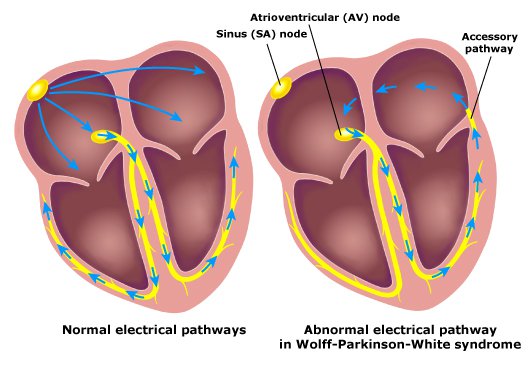
Atrial flutter is considered an unstable rhythm that may progress to atrial fibrillation or revert to sinus rhythm. Other etiologies should be considered in cases of chronic atrial flutter, such as Wolff-Parkinson-White syndrome. Wolff-Parkinson-White syndrome is a disorder of the heart that involves an additional pathway of conducting fibers between the atria and the ventricles. In cases of chronic atrial flutter, there is a possibility that the AV node will begin to conduct every ectopic atrial impulse resulting in potentially lethal ventricular fibrillation.
Pathology and Pathophysiology of Atrial Flutter
Atrial flutter is a supraventricular tachycardia with an atrial origin. Both type 1 and type 2 atrial flutter require a conduction block. The most common type, type 1, is caused by a reentrant loop type arrhythmia with an origin in the right atrium that passes around the tricuspid valve. Type 2 atrial flutter may have an origin in the left or right atrium, pulmonary veins (similar to atrial fibrillation), or the mitral valve annulus.
A reentrant loop type arrhythmia is characterized as a depolarization signal that moves in a tight circle through the conducting fibers of the heart, resulting in rapid uncontrolled contractions. In atrial flutter, this reentry circuit is limited to the atria. Only one of every two or three contraction signals passes through the AV node, resulting in a ventricular contraction.
Symptoms of Atrial Flutter
Signs of atrial flutter
The acute symptoms of atrial flutter are regular palpitations. This is usually well tolerated in a healthy heart in a healthy patient. However, if the patient is deconditioned or suffers from underlying heart disease they may develop symptoms including:
- Shortness of breath
- Chest pain
- Lightheadedness
- Dizziness
- Nausea
- Feelings of impending doom
A prolonged course of atrial flutter may result in heart failure. Symptoms include:
- Exertional breathlessness
- Edema
- Orthopnea
- Chest pain
Diagnosis of Atrial Flutter
An electrocardiograph is usually sufficient to diagnose atrial flutter.
ECG
On ECG the atrial heart rate of 250–350 bpm (type 1) or 350–450 bpm (type 2) as expressed by P waves. The P waves will have a distinct sawtooth shape and are sometimes called f-waves or “flutter waves”. Sawtooth flutter waves in ECG leads II, III, aVF are sufficient to diagnose atrial flutter type 1.
If the flutter waves are upright the reentry circuit runs clockwise. If the flutter waves are inverted the reentry circuit loop is counterclockwise (more common). Additionally, the QRS complexes are narrow as the ectopic beat originates in the atria. Finally, the atrial and ventricular heart rates will be at a constant ratio. A 2:1 or 3:1 ratio of P waves to QRS complexes is common.
Occasionally the heart rate is too fast to identify sawtooth flutter waves. An adenosine infusionwill slow the conduction velocity at the AV node, reducing the ventricular heart rate and increasing the number of observable repeating P waves. This may ease diagnosis. Alternatively, a vagal maneuver may provide the same diagnostic assistance. The most commonly used vagal maneuver in the clinic is the Valsalva maneuver
Echocardiogram
A transthoracic echocardiogram will be part of the standard workup for atrial flutter. This procedure will evaluate the left and right atria and help rule out cardiomyopathy, pericarditis, and valvular heart disease. Additionally, a transesophageal echocardiogram will likely be performed to detect any thrombus formed in the left atrium. Atrial flutter and atrial fibrillation both allow thrombi formation in the left atria that may result in a brain embolism.
Differential Diagnoses of Atrial Flutter
- Atrial fibrillation
- Atrial tachycardia
- Multifocal atrial tachycardia
- Tachycardia with variable AV block
- Ventricular tachycardia
Therapy of Atrial Flutter
Treatment of atrial flutter
A complete workup of a patient with atrial flutter would include ECG and transthoracic echocardiogram. Additionally, before cardioversion, a transesophageal echocardiogram will also be performed to rule out thrombus formation in the left atria. Atrial flutter of less than 48-hour duration does not require anticoagulation therapy. Anticoagulation is recommended for episodes of unknown duration or those lasting greater than 48 hours and is required for at least 4 weeks.
Anticoagulation options include:
- Heparin
- Warfarin: maintain an INR of 2–3
- Novel oral anticoagulants (dabigatran, apixaban, and rivaroxaban)
Cardioversion
Atrial flutter may resolve spontaneously or it may progress into atrial fibrillation. There are two cardioversion methods: electrical and pharmacological. Electrical cardioversion uses a jolt of electricity to reset the heart and restore a regular rate and rhythm. Pharmacologic conversion involves the use of medications (dofetilide or ibutilide). There is some risk involved with either procedure.
Ablation
First line treatment, for stable patients, is catheter-based radiofrequency ablation. This procedure is relatively low risk with a high success rate. A successful procedure may cure the condition and not require medication in the future.
Medication
Medication is the alternatives to ablation. The goal is rhythm control or rate control. Ventricular rate control may be achieved using medications that block AV node conduction such as beta blockers (atenolol, metoprolol, and propranolol) or calcium channel blockers (verapamil and diltiazem). Additionally, antiarrhythmic medications may be useful to restore a regular rhythm, specifically class IC, III, and IV.
Progression and Prognosis of Atrial Flutter
Atrial flutter is considered an unstable rhythm that may progress to atrial fibrillation or revert to sinus rhythm. Tachycardia-induced cardiomyopathy may occur if the ventricular rate remains elevated for a prolonged period of time and should be corrected early in the disease process. Additionally, thrombus formation is a concern with atrial flutter or atrial fibrillation. Treatment with catheter ablation is very well tolerated and rarely results in relapse.

Comentários
Enviar um comentário