Factors of Multiple Sclerosis
Auto-immune Factors of Multiple Sclerosis
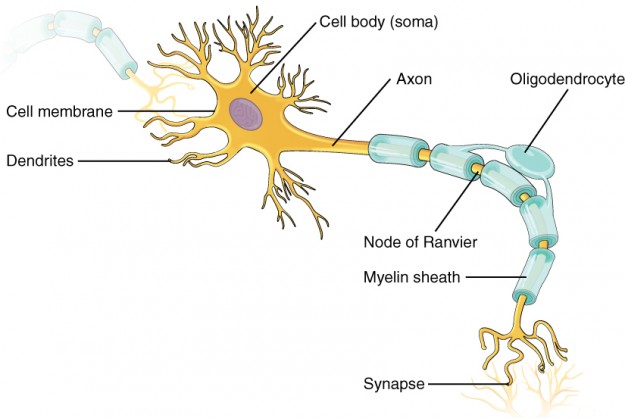
With MS, the immune system attacking the body’s own components refers to a reaction against CNS myelin antigens. This results in a reversible inflammatory reaction with demyelination. If this reaction is strong, the neuronal system experiences axonal damage with subsequent irreversible decay of nerve fibres.
At the functional level, the demyelinated nerves already begin losing the ability to effectively transmit action potentials, and the transmission of information is slowed. The periventricular white matter, the optic nerve, the brain stem, the cerebellar peduncles, the corpus callosumand the myelon are the most important predilection sites for these so-called demyelination lesions.
Clinical Course and Symptoms of Multiple Sclerosis
The clinical manifestations of multiple sclerosis can be distinguished into acute exacerbations versus the basic clinical course. These two components can be compiled to form a full picture of the disease. This is significant insofar as the management of an acute exacerbation differs from the prophylactic long-term treatment oriented toward the overall clinical course.
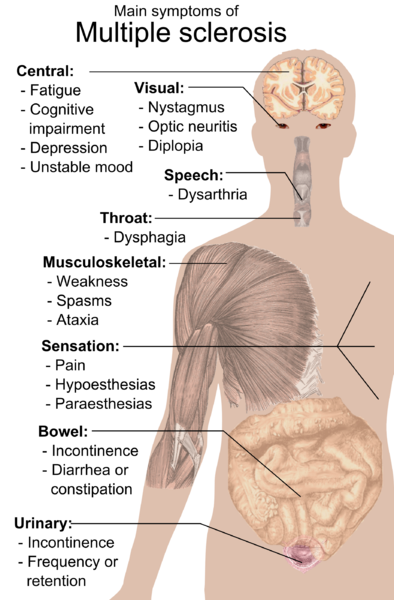
Image: “Main symptoms of Multiple sclerosis.” by Mikael Häggström. License: Public Domain
Definition of an Acute MS Exacerbation
A transient dysfunction lasting for at least 24 hours and which cannot be explained by fever or infections is considered an inflammatory exacerbation. Various neuronal qualities may be disrupted. This often results in:
- Sensory disturbances with dysesthesia, hypoesthesia, or neuralgiform pains. Along with tingling paresthesia, the Lhermitte sign (triggering of rapid downward paresthesia along the spine and/or extremities due to passive forward leaning of the neck) is often positive.
- Motor abnormalities with (spastic) paresis and disrupted fine motor skills. This leads to positive pyramidal signs, a lack of abdominal skin reflexes with increased muscular reflexes and cloni.
- Inflammation of the optic nerve (retrobulbar neuritis, optic neuritis) with hazy vision, central scotoma and painless loss of vision for hours or days, and pain when moving the bulb. Double vision, internuclear ophthalmoplegia, or mononuclear vision impairment typically manifest.
- Vegetative functional disorders with urge incontinence, residual urine buildup and sexual dysfunction.
- Brain stem symptoms like vertigo, impaired walking, loss of balance or coordination, and dysarthria.
- Charcot’s triad with scanning speech, volitional tremor, and nystagmus as expression of an inflammatory reaction around the cerebellum and the cerebellar peduncles.
As the inflammatory reaction can fundamentally affect the entire central nervous system, the symptoms of MS are accordingly manifold. The so-called pseudo-manifestations must be separated from the true ones. These are neurological disorders stemming from infections, fever, physical strain, hot baths or saunas, compiled together under Uhthoff’s phenomenon.
Clinical Course of Multiple Sclerosis
There are different clinical courses of MS. These courses vary greatly in terms of the distribution and severity of the symptoms, which makes MS a very heterogenous disease. The level of impairment is determined by the Expanded Disability Status Scale (EDSS).
The first, or non-recurring, inflammatory manifestation is called a clinically isolated syndrome.
Relapsing-remitting MS is initially present in 70 – 80% of all patients. This means that the neurological symptoms arise relatively suddenly and then recede once more.
In 50% of these patients, this is followed by conversion into a secondary progressive course, in which progressive deterioration of the symptoms occurs and manifestations are no longer clearly recognizable.
15% of all patients experience a primary proggressive course from the onset. This group of patients is generally somewhat older without frequency by gender. It should be noted that this manifestation is incredibly difficult to treat.
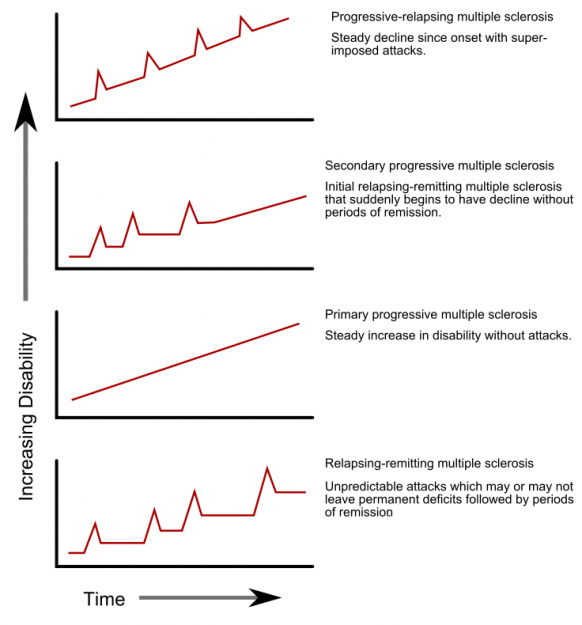
Image: “Progression types of multiple sclerosis” by Faigl.ladislav. License: Public Domain
Diagnosing Multiple Sclerosis
Diagnosing MS is based on the patient’s history and clinical examination, imaging of the entire CNS, liquor diagnostics, and electrophysiological performance diagnostics. Past symptoms must especially be enquired and examined.
As multiple sclerosis can fundamentally affect every structure of the central nervous system, extensive diagnostics are absolutely necessary. The thorough physical, neurological evaluation should comprise all qualities, and especially enquire about and evaluate the aforementioned typical symptoms.
As MS can often be made apparent in the form of visual and oculomotoric symptoms, supplementary ophthalmological examinations are useful. McDonald’s diagnostic criteria have proven useful in clinical practice as well. This stipulates the fulfilment of the following diagnostic requirements:
- Enquiring about and investigating the prior progression of the illness
- Verification of temporal and spatial dissemination of the disease via…
- …the clinical course with the presence of at least two manifestations (temporal dissemination)
- …the presence of one manifestation and verification of activity via MRT imaging
- Neurological symptoms cannot be better explained by anything other than MS; MS is thus a diagnosis of exclusion
Imaging of Multiple Sclerosis
MRT plays a particularly significant role here. The typical predilection sites (see above) should especially be examined. Should the clinical symptoms indicate a lesion in the region of the myelon, a spinal MRT should be conducted.
Various sequences can be used to find various indications of MS:
- T1 sequence: hypointensive lesions (black holes) and loss of brain volume as a sign of tissue loss
- T1 sequence + contrast agent (gadolinium): contrast agent enhancement of freshly active lesions as an indication of acute inflammation, fading inflammatory foci (old lesions) do not absorb any contrast agent
- T2 sequence, FLAIR sequence: hyperintensive lesions as signs of inflammation, cerebral edema, demyelination, and remyelination
Fluid Diagnostics of Multiple Sclerosis
Fluid diagnostics serve to determine the typical central inflammatory reaction of MS, and are also an opportunity to rule out several differential diagnoses. For instance, a cell count increase in the cerebrospinal fluid of approx. 10 – 50/yl speaks to the presence of MS, whereby a lymphocellular and monocytic image forms. However, it is not uncommon for the cell count in MS patients to remain normal.
Furthermore, the diagnostics are intended to examine the presence of fluid-specific, oligoclonal bands as indication of intrathecal IgG synthesis. If oligoclonal bands are present in the fluid, but not in the serum, this is an indication of MS. Also typical of MS is if the fluid contains positive antibodies for various neurotropic viruses, such as measles, rubella and shingles. Should the findings in the fluid be insignificant with suspected MS, this should be reexamined after approximately one year. The fluid results typical of MS are not specific.
Electrophysiological Diagnostics of Multiple Sclerosis
The various evoked potentials are examined via electrophysiological diagnostics. These potentials can be used to infer functional impairments in the central nervous system. If demyelination processes are occurring, this results in latency delays in the cortical stimulus response as a sign of retarded transmission of stimuli.
The visual (VEP), acoustic (AEP), sensory (SEP), or motor evoked potentials (MEP) are common examinations. Should the clinical evaluation reveal uncertainties as to whether the neuronal pathology is peripheral or central, the electrophysiological examination may, for instance, be supplemented with neurography or electromyography in a few differential diagnostic areas.

Comentários
Enviar um comentário