Herniated Disc (Spinal Disc Herniation) — Symptoms and Diagnosis
In Lecturio :) - Spinal disc herniation is a common cause for pain syndromes in the cervical and lumbar spine. It is the most common trigger for radiculopathies which lead to pain and disturbances of sensation of the dermatomes but can also be accompanied by pareses and loss of reflexes. Both for your examinations as well as in everyday clinical life, knowledge of radicular syndromes as well as their diagnosis and treatment are highly meaningful.
Table of Contents
- Definition of Spinal Disc Herniation
- Epidemiology of Spinal Disc Herniation
- Etiology of Spinal Disc Herniation
- Pathology and Pathophysiology of Spinal Disc Herniation
- Symptoms of Spinal Disc Herniation
- Diagnosis of Spinal Disc Herniation
- Differential Diagnosis of Spinal Disc Herniation
- Treatment of Spinal Disc Herniation
- Course and Prognosis of Spinal Disc Herniation
- Review Questions
- References
Are you more of a visual learner? Check out our online medical courses and start now for free!
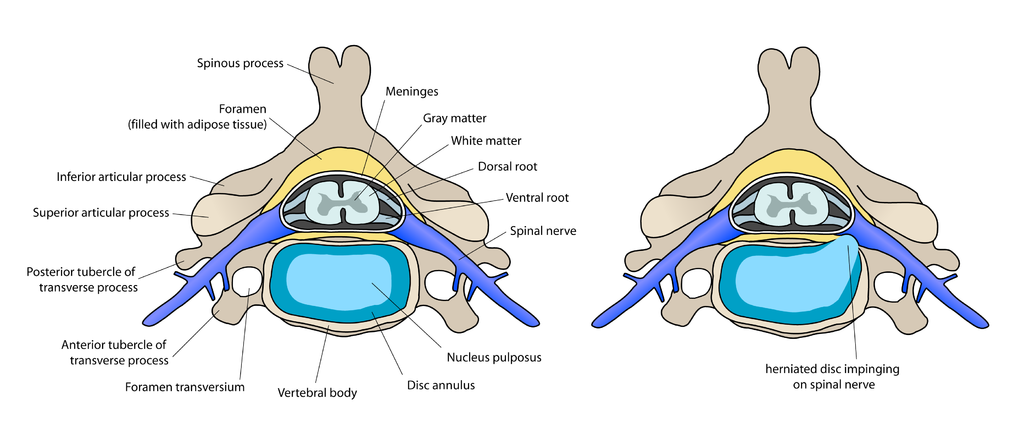
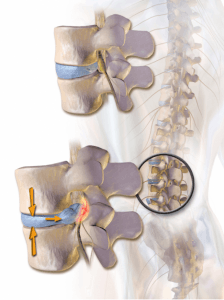
Image: “annotated diagram of preconditions for Anterior cervical discectomy and fusion” by debivort. License: CC BY-SA 3.0
Definition of Spinal Disc Herniation
Spinal disc herniation – slipped disc
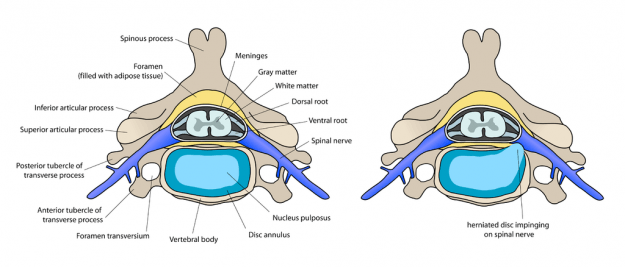
A spinal disc protrusion is a bulging disc while the annulus fibrosus remains intact.
A spinal disc herniation (also known as slipped disc), however, is the condition in which the annulus fibrosus is perforated and the nucleus pulposus is expelled through the area of perforation. The posterior longitudinal ligament of the spine (lig. longitudinale posterius) may in this case be intact or perforated.
Disc sequestration is the condition that is marked by a perforated posterior longitudinal ligament with torn pieces of the nucleus pulposus in the spinal canal.
Symptoms caused by spinal disc problems are varied. It serves to mention the clinical terms lumbago (also called lumbalgia) and lumboischialgia as well as cervicobrachialgia. It is important to know that these terms describe symptoms without etiologic specificity.
Lumbago is described as acute or chronic, non-radiating pain in the lumbar spinal region. Colloquially, this is simply known as “low back pain“.
Lumboischialgia or cervicobrachialgia presents with pain in the lumbar and cervical spinal region, respectively, which also radiates pain to the extremities. The segmentally radiating pain is caused by irritation of the nerve root.
Radicular syndrome (also nerve root compression, radiculopathy) describes the collection of symptoms that are caused by a compression or mechanical irritation of a spinal nerve root which can for example include the segmentally radiating pain which is seen in lumboischialgia and cervicobrachialgia.
Note: Spinal disc herniation is the most common cause of a radicular syndrome. Acute inflammation, fractures as well as chronic degenerative, inflammatory and neoplastic processes can cause radicular symptoms as well.
Epidemiology of Spinal Disc Herniation
Commonly afflicted by spinal disc herniation
Low back pain (lumbago), which has a point prevalence of 37 % and a lifetime prevalence of 87 %, is the most important pain syndrome right behind headache.
Pain in the cervical spinal region with radiating pain to arms and shoulders (cervicobrachialgia) is a common problem as well.
Degenerative disc disease is a common cause of vertebral pain syndromes. Most commonly affected is the lumbar spinal region (about 2/3 of cases), second most common is the cervical spinal area. Thoracic spinal disc herniation is quite rare.
Spinal disc herniation most commonly affects people between their 20th and 65th year of life with a maximum occurrence between their 45th and 55th year of life. Men are affected more commonly.
Etiology of Spinal Disc Herniation
Causes of spinal disc herniation
Prerequisite for the development of a spinal disc herniation is a fateful degeneration of the spinal disc with fissures of the annulus fibrosus. Conversely, traumatic destruction of a previously intact spinal disc is extremely rare.
A prolapsing spinal disc can cause compression of the myelon (myeolopathy), the conus medullaris or the cauda equina (conus and cauda syndromes) or irritation of the respective spinal nerve roots (radiculopathy).
Spinal discs (discus intervertebrales) are responsible for the movement and cushioning of the spine. With advancing age, the number of blood vessels reaching the discs decreases which supports fibrosis of the jelly-like nucleus pulposus, while the surrounding annulus fibrosus loses its taut texture. These changes can already be observed histologically in early adulthood.
If for example the annulus fibrosus shall tear with high exertion, parts of the nucleus pulposus can prolapse. Spinal disc herniation occurs. In case of a spinal sequestration, torn bits of nucleus pulposus are in the spinal canal and the posterior longitudinal ligament is perforated. This happens predominantly in the lateral aspects of the posterior longitudinal ligament since it is most strongly attached to the annulus fibrosus at the midline.
Pathology and Pathophysiology of Spinal Disc Herniation
Affected structures of a spinal disc herniation
The spinal disc tissue can shift medially, mediolaterally or laterally during spinal disc hernitaion. Most common are mediolateral herniations which ordinarily damage those nerves in the cervical and lumbar region which are assigned to the vertebra located beneath the disc.
In case of herniation of the disc between C6 and C7, the affected nerve root is C7 since in the cervical spine the nerve roots extend above the assigned vertebral body (in the cervical spinal region there are seven vertebrae but eight nerve roots). In case of a herniation between L5 and S1, the affected root is S1.
Image: “annotated diagram of preconditions for Anterior cervical discectomy and fusion” by debivort. License: CC BY-SA 3.0
A lateral herniation in the lumbar spinal region can damage the nerve root belonging to the higher vertebra as well. This may sound complicated but can be deducted by knowledge of the lumbar spine anatomy: This is where the nerve roots leave the spinal canal underneath the corresponding vertebra while the nerve roots of the next lower segment have their exit medially. This way a lateral herniation at L3/4 can cause L3 syndrome, a mediolateral herniation however causes L4 syndrome.
Note: Cervical spinal disc prolapse often occurs at level C5/6 and C6/7 while lumbar prolapse most often occurs at level L4/5 and L5/S1.
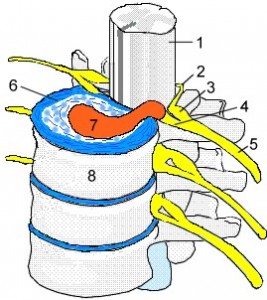
Image: “Discusprolaps” by Uwe Gille, Scuba-limp. License: CC BY-SA 3.0
- Spinal cord
- Dorsal root
- Spinal ganglion
- Ventral root
- Spinal nerve
- Spinal disc
- Spinal disc
- Annulus fibrosus
Conus/cauda syndrome caused by spinal disc herniation
The adult spinal cord ends at about the L1 level at the conus medullaris. Underneath, the lumbar and sacral nerve roots run as cauda equina in the spinal canal. Marked medial spinal disc prolapse in the lumbar region can cause compression of the conus medullaris or all nerve roots of the cauda equina at the corresponding level which cause a conus or cauda syndrome (see below). If cauda equina and conus medullaris are affected at the same time, it is referred to as a conus-cauda syndrome.
Myelopathy caused by spinal disc herniation
Massive cervical or thoracic spinal disc prolapse can cause myelopathy by compressing the spinal column. This causes spastic pareses, pyramidal signs and bladder control dysfunction.Symptoms of Spinal Disc Herniation
Generalized inflammatory symptoms of spinal disc herniation
Leading symptom of a lumbar spinal disc herniation is lumbar pain. Trigger can be new or physiologically awkward movement. Pain can be magnified by coughing, straining or sneezing. In case of nerve root irritation in the L5/S1 region the Lasegue sign can be positive (that is the reversed Lasegue sign in the L3/4 area).
Cervical involvement also causes pain in the affected spinal area. Often there will be certain avoidance postures (caput opstipum = “wry neck”, abnormal straightening, scoliosis, torsion), as well as restricted movement and paravertebral myogeloses.
Radicular symptoms of spinal disc herniation
Most commonly, nerve root compression syndrome develops with spinal disc herniation (= radiculopathies, radicular syndrome). Through irritation of the exiting nerve roots there will be radiating pain and sensitivity disturbances in the corresponding dermatomes. In case of cervical disc herniation, pain radiates into the arm (cervico-brachialgia). Lumbar disc herniation is hallmarked by lower back pain which affect buttocks and legs (lumbo-ischialgia). Depending on severity and position of the herniation there can be pareses and decreased muscle reflexes.
These are the important cervical radicular syndromes:
| Syndrome | Paresis | Pain radiation, paresthesia, sensitivity disturbance | Weakened reflexes |
| C5 | Deltoideus | Lateral shoulder | Biceps reflex |
| C6 | Biceps brachii, M. brachioradialis | Radial arm extending to thumb | Biceps reflex, radial reflex |
| C7 | Triceps brachii | Regio antebrachii dorsalis, dorsal hand extending to 2nd-4th finger | Triceps reflex, biceps reflex |
| C8 | Small hand muscles | Ulnar arm, lateral hand extending to 5th finger | Tromner reflex |
| Syndrome | Paresis | Pain radiation, paresthesia, sensitivity disturbance | Weakened reflexes |
| L3 | Deltoideus | Transverses anterior aspect of the thigh towards knee | Adductor reflex, perhaps patellar reflex |
| L4 | Quadriceps, M. tibialis ant. | Anterior and medial lower leg | Patellar reflex |
| L5 | Extensor hallucis longus (lifts big toe), perhaps M. tibialis ant. and post., M. gluteus med. | Lateral and anterior lower leg, dorsal foot extending to big toe | Tibialis posterior reflex |
| S1 | Triceps surae (plantar flexion, test perhaps through standing on toes), M. glutaeus max., M. biceps femoris | Posterior and lateral thigh, lateral foot | Achilles tendon reflex |
| S2 – S4 | Bladder and rectum dysfunction (CAVE: neurologic emergency, see cauda syndrome) | Posterior thigh, anal region (cauda syndrome: breeches pattern) | Anal reflex |
Symptoms of myelopathy
If medial spinal disc herniation causes compression of the spinal cord in the cervical or thoracic region, it can lead to spastic pareses of the lower extremities via damage of the neural pathways (upper motoneuron). Reflexes are heightened and pyramidal signs occur. Further, there may be continence dysfunction of the bladder and colon as well as a positive Lhermitte‘s sign in case of cervical myelopathy.
Note: Typically, symptoms do not display complete paraplegia but rather through one-sided compression of the spinal cord Brown-Séquard syndrome: spastic paresis and hypesthesia below the lesion, contra laterally removed pain and temperature sensation (dissociated sensitivity dysfunction).
Symptoms of Conus and Cauda syndrome
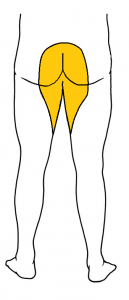
Image: “Saddle anesthesia” by Lesion. License: CC BY-SA 3.0
Marked medial spinal disc herniation which is isolated to the conus medullaris region cause loss of sensitivity in the pattern of so-called “breeches anesthesia” (perianal and medial thighs on both sides). The polysynaptic reflexes, anal reflex and bulbocavernosus reflex (S3 – S5 or S3/4), are gone. The anal sphincter is flaccid. There will be dysfunction of urinary and fecal continence and sexual dysfunction.
Cauda syndrome is caused by a lesion below L1 which is affecting the cauda equina and leads to segmentally limited and limp paraparesis, limited reflexes as well as radicularly limited sensitivity dysfunction. Depending on level of the lesion the cremasteric reflex (L2) may be gone.
Note: Paresis of the legs does not belong to the isolated conus syndrome. Conus syndrome occurs with isolated damage of the conus medullaris (S3 – S5) at the L1 level. In case of involvement of conus medullaris as well as cauda equina, the appropriate terminology is conus-cauda syndrome.
Diagnosis of Spinal Disc Herniation
Anamnesis for spinal disc herniation
Anamnesis is an important part of diagnosing pain in the spinal area. Try to capture the pain characteristics and accompanying symptoms as well as previous illnesses which may serve as warning signals for specific causes of the pain with urgent call for action. The following red flags serve early detection of preventable dangerous courses which should always be asked:
Fracture
|
Severe trauma (motor vehicle accident, fall from great height, sports injury), minor trauma for elderly or patients potentially affected by osteoporosis; systemic steroid therapy
|
Tumor
|
Advanced age, history of tumors, generalized symptoms (fatigue, loss of appetite), pain which increases in supine position; strong pain at night
|
Infection
|
Generalized symptoms (acute fever, chills, loss of appetite, fatigue) past infection, consummating general illness; drug abuse; immune suppression; strong pain at night
|
Radiculopathy
|
Pain radiating in lanes into the legs perhaps with feeling of numbness or tingling paresthesia or feeling of weakness; Cauda syndrome: sudden bladder or rectal dysfunction, perianal and perineal loss of sensation; marked/increasing neurologic deficit; Cessation of pain with increasing paralysis up to complete loss of function of the reference muscle (nerve root death)
|
Clinical examination of spinal disc herniation
With suspicion of radicular syndrome, a careful clinical examination should follow. Because of pain radiation, possibly existing paresis and reflex limitations as well as loss of sensitivity a damaged nerve root can be assumed.
Note: Loss of sensitivity in radiculopathy runs in a striated fashion along the dermatomes. For differential diagnosis purposes one must delineate segmented loss of sensitivity from peripheral nerve damage which rather affects areas of limited skin regions.
Examination of sharp or dull discrimination is of help to associate sensitivity dysfunction of corresponding segments since the thus examined sensation of pain in the dermatomes is not as overlapping as sensitivity of touch.
Positive Lasegue test for spinal disc herniation
The positive Lasegue sign is a positive indicator of nerve root irritation. A positive Lasegue test occurs when the stretching of the N. ischiadicus (roots L5/S1) causes pain. The patient is in a supine position while the examiner lifts the patient’s extended leg. If there is radiating pain at about 45° the result is considered pathologic.
The reverse Lasegue test shows a painful stretching of N. femoralis (roots L3/L4) an. For this test the patient is in prone position while the leg is bent at the knee and the foot is guided toward the buttocks with a lifted thigh. Radiating pain and attempted evading motion by the patient constitute a positive test result.
Radiologic diagnosis of spinal disc herniation
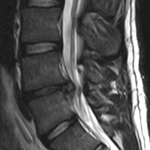
Image: “L4-l5-disc-herniation” by Edave. License: CC BY-SA 3.0
MRI (axial and sagittal) is the method of choice to confirm spinal disc herniation. In order to judge osseous structures, conventional x-ray as well as CT can be performed. Further diagnostic clues can be gathered with myelographic imaging.
Note: It is possible for disc herniation to be asymptomatic and, conversely, there can be radicular dysfunction without prolapse that can be proven diagnostically or surgically.
Neurophysiological examinations
Under certain circumstances, electrophysiological examinations can serve to differentiate between radiculopathy and peripheral nerve damage. In principle, no additional electrophysiological confirmation is necessary for monoradicular syndrome with appropriate imaging and corresponding proof of compression.
Differential Diagnosis of Spinal Disc Herniation
Spinal disc herniation in the lumbar region can be differentiated from unspecific back pain with pseudo-radicular radiating pain as well as other causes of radicular syndrome.
Pseudo-radicular syndrome of spinal disc herniation
Back pain that appears radicular in nature and radiates into arms and legs but is not immediately caused by nerve root compression is called pseud-radicular syndrome. Pain does not typically radiate strictly radicularly; perhaps there may be paresthesia (however without strong correlation to dermatomes). The cause for this syndrome is usually orthopedic in nature, perhaps through facet syndrome or iliosacral joint syndrome. This constitutes joint distortions (“blockages”) which are consequences of degenerative changes or poor posture.
Peripheral nerve lesions of spinal disc herniation
Peripheral nerve lesions or plexus lesions can mimic nerve root damage clinically. Aside from an exact analysis of clinical symptoms neurography can help with differentiation.
Radiculitis of spinal disc herniation
Radiculitis caused by either a bacterial or viral infection (mainly borreliosis and herpes zoster), autoimmune or cryptogenic inflammation should be considered in differential diagnosis. Aside from spinal disc herniation, localized demand on space (tumor, bone metastases) can cause radiculopathy. Also, degenerative spinal changes, spinal abscesses or spondylodiscitis should be considered as well as the possibility of diabetic radiculopathy.
Treatment of Spinal Disc Herniation
Conservative treatment of spinal disc herniation
Radiculopathy should be treated conservatively initially. In case of cervical radiculopathy, limiting motion via a neck brace may be called for as well as recommending mobilizing physiotherapy. Rest for patients with lumbalgia in its acute phase is no longer recommended. Also patients with radicular syndromes are advised to seek physiotherapy and be active four days after the acute event at the latest.
Pain is treated with analgesics (Acetaminophen, NSAID) and muscle relaxers. If non-opioid analgesics prove ineffective, weak opioid analgesics may be prescribed. Principally, treatment follows the st\
ep-care of the WHO.
ep-care of the WHO.
Note: Chiropractic treatment is contraindicated for spinal disc herniation.
Surgical treatment of spinal disc herniation
Absolute indicators for surgical treatment of spinal disc herniation are:- Damage to bladder and rectum
- Conus-Cauda syndrome
- Noted paresis (3/5)
- Signs of myelopathy
Relative indicators are spinal disc sequestration and failure of conservative therapy (persisting pain syndrome over for weeks in spite of conservative therapy).
Spinal disc material can be removed through micro-surgical discectomy: Under certain circumstances there will be intercorporal spondylodesis (fusion, “stiffening”) following surgery.
Course and Prognosis of Spinal Disc Herniation
Abatement of the spinal disc herniation
With adequately administered conservative therapy, up to 80 % of spinal disc herniation cases and effects of acute radicular syndrome will abate. With good observation of indications, this compares to the surgical success rate.
The rate of recidivism, however, is rather large. Appropriate prophylaxis consisting of muscle building exercises, sufficient motion and reduction of excess weight are important.
Review Questions
The answers are below the references.1. A 40-year old man feels sudden pain with lifting of a heavy moving box in lower lumbar spinal region which radiates to the right dorsal foot and his right big toe and is more severe when coughing. What is the most likely condition he is presenting with?
- Lumbar spondylolisthesis
- Lateral spinal disc herniation between L3 and L4, right
- Conus syndrome
- Radiculopathy of the L5 nerve root, right
- None of the above
- Neuro-borreliosis
- Vertebral fracture
- Spinal disc herniation L4/5
- Diabetic radiculopathy
- None of the above
- Sensitivity dysfunction perianally and of both medial thighs
- Weakened lift of the lateral foot
- Loss of anal reflex
- Flaccid anal sphincter
- None of the above.
Este comentário foi removido por um gestor do blogue.
ResponderEliminarSorry by mistake I eliminated your comment, when I was going to answer it, thank you for your words. My goal is that profesionals and students or citizens can learn something with the articles, because in some countries even when people are struggling to do a health degree is imposible to buy a book, that´s my hope.
EliminarAmazing post !! This is so informative blog. Keep sharing. if you are looking for Pain Management. Check the Link.
ResponderEliminarthank you