Spermatogenesis and Oogenesis
In Lecturio - The subject of gametogenesis as the umbrella term for spermatogenesis and oogenesis is a basic part of embryology. Human germ cells are the basis for the development of new life. It is important to understand this development in detail since errors can occur which make postnatal life impossible or severely change it.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your embryology course now for free!
Development of Germ Cells
In the beginning of the embryonic development, the primordial germ cells lie along the wall of the yolk sac. In the fourth week, they pass the hindgut to reach the differentiating gonads. Depending on if they develop to ovaries or testicles, these cells are referred to as oogonia or spermatogonia, respectively.The special feature of the gametes is that they have a haploid set of chromosomes. So, they contain only 23 chromosomes with mixed maternal and paternal shares. Concerning the later fertilization of the egg cell by the sperms, this makes sense since they form a diploid set of chromosomes together.
Meiosis is responsible for halving the set of chromosomes. In reduction division, the 46 chromosomes are segregated into two cells with 23 chromosomes each so that the DNA content is now 1n2c, that is half the set of chromosomes but the normal number of chromosomes. In the following equational division, no DNA replication occurs so that only the sister chromatids are segregated and the resulting DNA content can be referred to as 1n1c.
Oogenesis – Maturation of Female Germ Cells
Oogenesis starts in the fetal period, but then halts. It is continued in puberty at the age of 12 to 15 years.12th to 16th week of pregnancy: Prenatal maturation of female germ cells
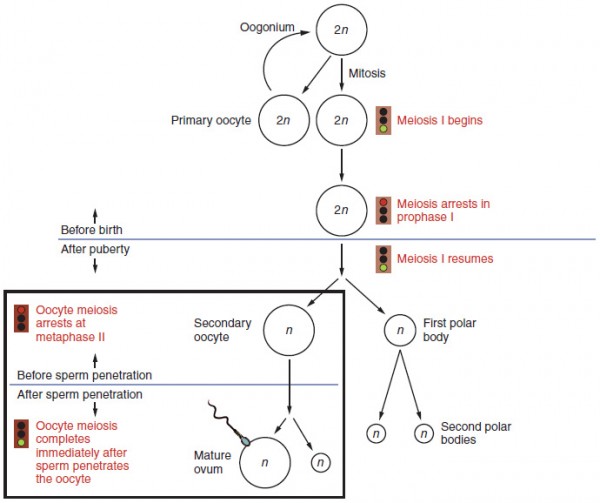
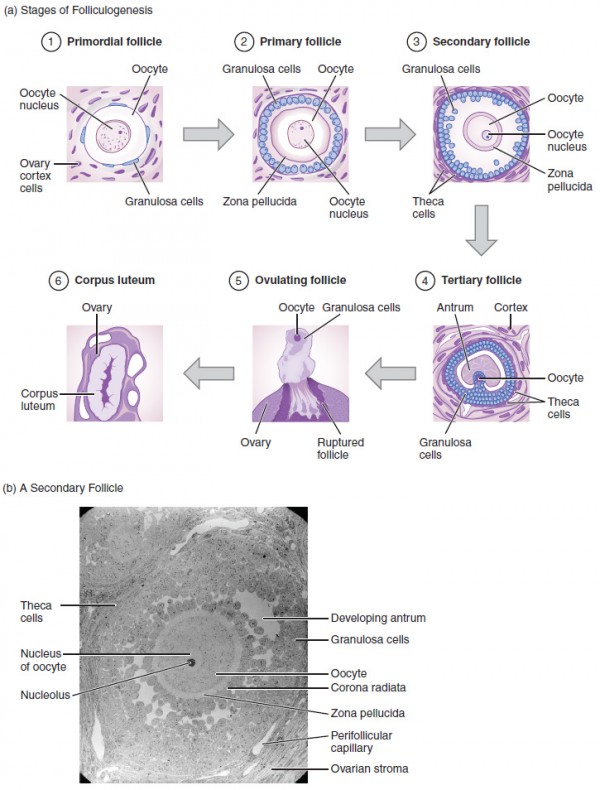
In this time, the primary oocytes or oocytes of first order develop. For this, the oogonia proliferate via mitosis. Also, they grow a little bit. However, the prophase of meiosis is not completed. The cells halt in the diplotene of the prophase and still have a diploid set of chromosomes. Due to the net-like appearance, this idle state is referred to as dictyotene.The primary oocytes are surrounded by follicular epithelial cells, which develop from the decaying sex cords. Thus, they form a flat, single-layer cover around the oocytes. This complex is called primordial follicle. Roughly seven million egg cells are created until the sixth month. Until birth, about five million of them perish. After birth, no more primary oocytes can be created!
Postnatal maturation of female germ cells
A few follicles mature to tertiary follicles before puberty, which are, however, removed again. This process is called follicular atresia. In the beginning, there are roughly 200,000 primordial follicles in the arrested state of the dictyotene. Month after month, primordial follicles mature to primary follicles with a cover that is still a single-layer, but now out of cuboid cells.Only a couple of these primary follicles develop further. They become so-called secondary follicles with a multilayer cover out of follicular epithelium cells. They produce a substance out of glycoproteins, which surrounds the egg cell as the zona pellicuda. The oocyte grows larger and adopts an eccentric position. Cavities form, which fuse to form a large one, the antrum, which is filled with follicular fluid. Thus, a tertiary follicle has formed.
In the tertiary follicle, the oocyte, which protrudes into the follicular cavity surrounded by the zona pellicuda, then builds the cumulus oophorus. A layer of granulosa cells is in direct contact with the zona pellicuda, which is referred to as corona radiata since it is serrated. The tissue of the ovary differentiates into the theca interna, which is rich in vessels and produces androgens, and the theca externa, which stabilizes the follicle and consists of connective tissue.
Under the influence of follicle stimulating hormone (FSH) only one of the tertiary follicles becomes the graafian follicle every month. This happens about seven days before ovulation. It has a diameter of 1.5 to 2.5 centimeters and can be seen as the stigma from the outside of the ovary. This graafian follicle is the egg cell, which will eventually ovulate.
Roughly twelve hours before ovulation the first meiotic division is completed in the graafian follicle. In the course of this process, the first polar body with one set of chromosomes is pinched off. The other set stays within the egg cell, which is now called secondary oocyte or oocyte of second order. It contains the major part of the cytoplasm and cell organelles so that the polar body is significantly smaller and quickly degenerates. The nucleus of the egg cell is still diploid.
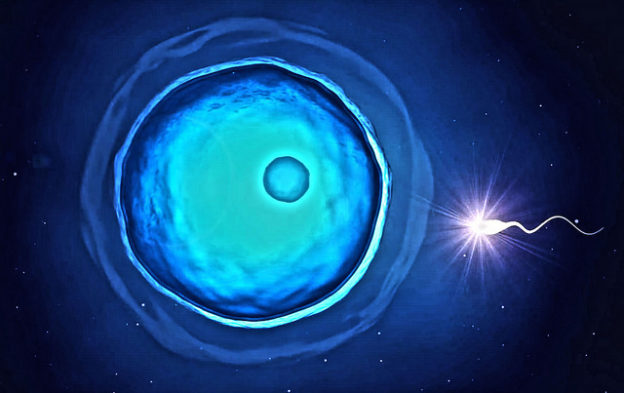
On the 14th day of the female menstrual cycle, ovulation occurs. The egg cell ovulates with the zona pellucida and the corona radiata. This means that it leaves the ovary and is then caught by the fimbriae of the fallopian tube. Simultaneously, the second meiotic division begins. It also halts, but this time in the metaphase. It continues if the egg cell is fertilized.
If the egg cell is fertilized, the second meiotic division is continued. Again, a secondary polar body is pinched off, which contains a minimal amount of cytoplasm. It remains in the fertilized oocyte, the ovum. The nucleus now contains a haploid set of chromosomes, which can fuse with the set of chromosomes of the sperm.
Since the egg cell ovulates with the zona pellicuda and the corona radiata, the rest of the follicle remains in the ovary. It collapses and fills with blood of the theca interna. Thus, it is called corpus hemorrhagicum at this moment.
Under the influence of luteinizing hormone (LH) out of lutein cells, it becomes the yellowish corpus luteum. The yellowish coloration is due to embedded lipids of the lutein cells. The corpus luteum produces progesterone and a little bit of estrogen, which leads to changes in the endometrium. That is the build-up of the uterine mucosa as preparation for a possible implantation of the egg cell.
In the event of fertilization of the egg cell, the corpus luteum becomes the corpus luteum graviditatis and produces hormones until the 20th week of pregnancy. The hormone hCG (human chorionic gonadotropin) maintains it. This hormone is used for diagnostic purposes in pregnancy tests. Then, its function is performed by the placenta and the corpus luteum graviditatis degenerates.
If the egg cell is not fertilized corpus luteum stops secreting progesterone and decays. It degenerates after only ten days. In both cases, white scar tissue remains, that is the corpus albicans. This process repeats as the ovarian cycle until the eventual absence of menstruation, the menopause.
Spermatogenesis – Maturation of Male Germ Cells
In contrast to oogenesis, the male germ cells are able to not only develop before birth, but to also replicate after birth.Prenatal maturation of male germ cells
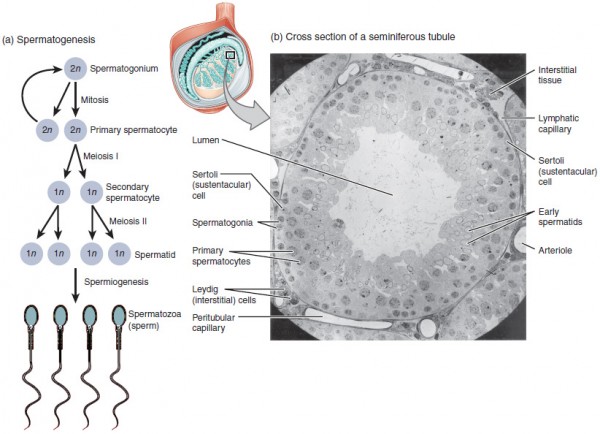
Prenatally, sertoli cells stop the male germ cells in their maturation process after their immigration into the testicle. As mainly undifferentiated cells, they remain in the testicle whose tubuli are not canalized yet. With the onset of puberty, the seminiferous tubules develop and the maturation of the spermatogonia to sperms begins.Postnatal maturation of male germ cells
When puberty begins, the spermatogonia significantly proliferate. One distinguishes two types: The first type always provides new spermatogonia; the second type begins with maturation. In the first step, the primary spermatocyte or spermatocyte of first order develops out of the second type when the spermatogonia enter the prophase of meiosis. They have a diploid set of chromosomes (2n2c). This phase last roughly three weeks.Further phases of the first meiotic division follow the long prophase. At the end of it, there are two spermatocytes. These are referred to as secondary spermatocytes or spermatocytes of second order. They undergo the second meiotic division, resulting in four haploid spermatids. With each division, the size of the cells is halved so that the spermatids amount to about a quarter of the size of the spermatocytes.
The following process is called spermiogenesis. It is the last step of spermatogenesis and makes the spermatids become functional sperms. The secondary spermatocytes are connected with each other via bridges of cytoplasm, since both the first and the second meiotic divisions are performed with an incomplete diakinesis. Now four separated mature sperms develop.
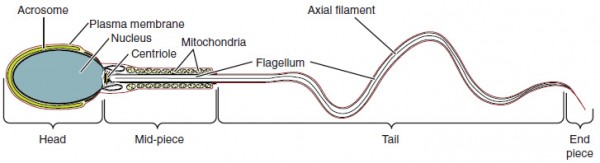
Firstly, the organelles and the excess cytoplasm are pinched off in residual bodies and the tail of the sperm, is formed. This process begins in the seminiferous tubules and continues all the way to the epididymis. This is where the final maturation takes place. The result is a functional sperm with head, neck, and tail.
The head of the sperm contains the nucleus and is covered with the acrosome. The neck part follows, it contains the proximal centriole, which is important for the fertilization of the egg cell. The last part of the sperm is the tail, which is divided into three parts:
- Mid-piece
- Main piece
- End piece
However, the sperms have to undergo a final maturation. After ejaculation a so-called conditioning or capacitation takes place, which takes roughly seven hours. During this process, the membrane components change, but not the sperm’s morphology. Mostly, this happens in the fallopian tube and is essential for fertilization, as the acrosome reaction cannot be performed without the conditioning of the sperms.
Abnormal Gametogenesis
Pathological processes during spermatogenesis and oogenesis primarily refer to the chromosomal level. An example for disturbed gametogenesis is non-disjunction, the incorrect segregation of chromosomes into the gametes. It can occur in the course of the first and the second meiotic division and leads to gametes with too many or too less chromosomes. Only a few of these incorrect segregations are consistent with postnatal life.A typical example for meiotic non-disjunction is trisomy 21 or Down syndrome. In this case, all or part of a third copy three chromosomes 21 are present and it only rarely occurs via translocation. The clinical picture is mainly shaped by the characteristic face and the Simian crease. Patients with trisomy 13 and 18 are also capable of surviving. These chromosomal abornmalities can be caused by non-disjunction.
While the mentioned trisomies are characterized by a numeric aberration of the autosomes, there are syndromes with a numeric aberration of the gonosomes. The Turner syndrome with a 45, X0 set of chromosomes and the Klinefelter syndrome with at least 47, XXY are two of these aberrations.
If non-disjunction occurs in one of the blastomeres after fertilization, it is possible that only a few cells carry this chromosomal abnormality, which results in a mosaic. This formation of a mosaic can also occur in the mentioned trisomies and the Klinefelter and Turner syndromes. In this case, the clinical changes are less distinctive compared to the case where all cells carry the abnormality.
Especially, the age of the mother plays a role in the occurrence of chromosomal defects. At late pregnancies, the oocytes can halt in the prophase for more than 40 years and are exposed to the environmental impact. Thus, the risk for chromosomal defects significantly rises at the age of 35.

Bild: “X-ray image of the legs of a 10-year-old boy with achondroplasia” by Kinderradiologie Olgahospital Klinikum Stuttgart . License: CC BY-SA 3.0
Review Questions
The solutions can be found below the references.1. Which of the following is correct?
- Primordial follicles mature to secondary follicles.
- Secondary oocytes develop prenatally.
- Secondary oocytes halt in the diplotene of the prophase.
- Primary oocytes begin the first meiotic division prenatally.
- The first meiotic division begins after ovulation.
- …are characterized by incomplete diakinesis.
- …need not further maturation or change in order to fertilize the egg cell.
- …consist of main, middle, and end piece.
- …complete maturation in the seminiferous tubules.
- …have a head, which is covered by the acrosome.
- Oogonia
- Spermatogonia
- Oocytes
- Primordial germ cells
- Sperms

Hello everyone
ResponderEliminarI am Angelica, 36yrs.I was diagnosed with PCOS/insulin resistance, me and my husband have been trying for more than 12years so we went to the obgyn and he put me on metformin 500mg 1x a day progesterone, Clomid 50 mg first month no ovulation 2nd month he upped the dosage on clomid to 100 that didn't make me ovulate either i am not on my last day of progesterone and will be taking clomid 150mg i am also taking dexamethasone and pregnitude to help me ovulate. my next step was the injections and looking into them they are very costly and steel no positive result then i saw on the internet how people uses herbal herbs from Dr James herbal made medicine to get pregnant and cures all kinds of diseases so i gave a try and here 2017 i got pregnant and got a baby girl and i decided to try again and i contacted Dr James again earlier this year and I'm now 5 weeks pregnant thanks DR James.. if you are in my situation and you are suffering from such diseases like dont go and wast your money on drugs and injections Alzheimer’s disease,Bechet’s disease,Crohn’s disease,Parkinson's disease,Schizophrenia,Lung Cancer,Breast Cancer,Colo-Rectal Cancer,Blood Cancer,Prostate Cancer,siva.Fatal Familial Insomnia Factor V Leiden Mutation ,Epilepsy Dupuytren's disease,Desmoplastic small-round-cell tumor Diabetes ,Coeliac disease,Creutzfeldt–Jakob disease,Cerebral Amyloid Angiopathy, Ataxia,Arthritis,Amyotrophic Lateral Sclerosis,Fibromyalgia,Fluoroquinolone Toxicity
Syndrome Fibrodysplasia Ossificans ProgresS sclerosis,Seizures,Alzheimer's disease,Adrenocortical carcinoma.Asthma,Allergic diseases.Hiv_ Aids,Herpe ,Copd,Glaucoma., Cataracts,Macular degeneration,Cardiovascular disease,Lung disease.Enlarged prostate,Osteoporosis.Alzheimer's disease,
Dementia.Lupus.
,Cushing’s disease,Heart failure,Multiple Sclerosis,Hypertension,Colo_Rectal Cancer,Lyme Disease,Blood Cancer,Brain Cancer,Breast Cancer,Lung Cancer,Kidney Cancer, HIV, Herpes,Hepatitis B, Liver Inflammatory,Diabetes,Fibroid,(A just reach him ON : drjamesherbalmix@gmail.com And You can call/WhatsApp dr James on +2348152855846