Recurrent Laryngeal Nerve Injury — Causes and Surgery in lecturio
Table of Contents
- Anatomy and Function of the Recurrent Laryngeal Nerve
- Pathology of the Recurrent Laryngeal Nerve Injury
- Causes of Recurrent Laryngeal Nerve Injury
- Clinical Manifestations of the Recurrent Laryngeal Nerve Injury
- Diagnosis of the Recurrent Laryngeal Nerve Injury
- Management of the Recurrent Laryngeal Nerve Injury
- References
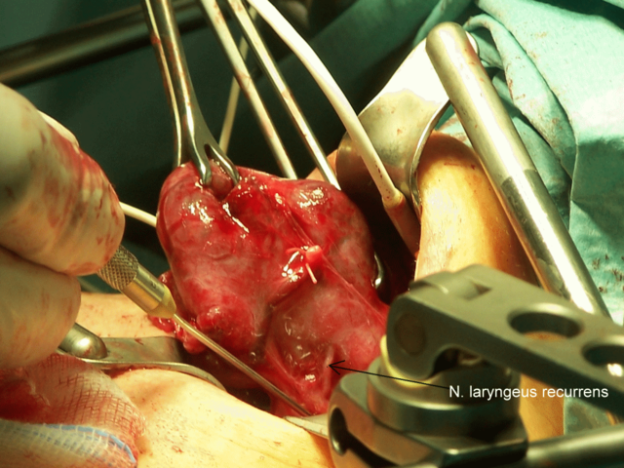
Image: “Strumaresection; N.laryngeus recurrens completely.” by THWZ – Own work. License: CC BY-SA 3.0
Anatomy and Function of the Recurrent Laryngeal Nerve
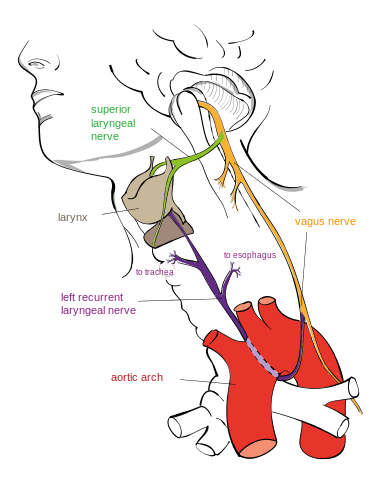
Image: “Drawing of the left recurrent laryngeal nerve.” by Jkwchui – Based on drawing by Truth-seeker2004. License: CC BY-SA 3.0
The recurrent laryngeal nerve receives sensory innervation from the trachea, esophagus and pyriform sinus before it enters the larynx deep to the inferior constrictor muscle and posterior to the cricothyroid articulation. The inferior thyroid artery and its branch; inferior laryngeal artery are responsible for supplying the recurrent laryngeal nerve with blood. The recurrent laryngeal nerve may pass anterior, posterior or between the branches of inferior thyroid artery.
Motor fibers of the recurrent laryngeal nerve supply the lateral and posterior cricoarytenoid muscles and thyroarytenoid, as well as the oblique and transverse interarytenoids. The posterior cricoarytenoid is responsible for vocal cords abduction, while the thyroarytenoid, interarytenoid and lateral cricoarytenoid are responsible for adduction of the vocal folds. The recurrent laryngeal nerve also gives motor innervation to the inferior constrictor muscle and cricopharyngeus muscle. Sensory innervation carried by the recurrent laryngeal nerve supplies both the subglottis and the mucosa of the vocal folds.
Anatomy of the vocal folds
There are two pairs of vocal folds; the true which consist of muscles, ligaments, lining mucosa and false folds which are superior to the true folds. The laryngeal ventricle is a recess which separates both the true and false vocal folds. Vocal folds extend from the arytenoid cartilage posteriorly to the midline anteriorly. Both vocal folds approximate only during Valsalva and cough. The true vocal folds divide the larynx into 3 compartments; supraglottis, glottis and subglottis.
Muscles of the larynx can be subdivided into intrinsic and extrinsic muscles. Intrinsic muscle is responsible for vocal folds mobility and phonation. Intrinsic muscles include; posterior and lateral cricoarytenoid, interarytenoid, cricothyroid and thyroarytenoid muscles. During inspiration, the true vocal folds are abducted laterally, while, during phonation, they move medially towards the midline.
All intrinsic muscles of the larynx are innervated by the recurrent laryngeal nerve except the cricothyroid muscle which is innervated by the external branch of the superior laryngeal nerve. The recurrent laryngeal nerve is responsible for sensory innervation of laryngeal mucosa below the level of the vocal folds.
Pathology of the Recurrent Laryngeal Nerve Injury
Recurrent laryngeal nerve paralysis can involve the left recurrent laryngeal neve, the right recurrent laryngeal nerve or both.The left recurrent laryngeal nerve is more susceptible to injury than the right nerve being more superficial and longer running from the chest up through the neck. Injury can be due to surgery, trauma, bacterial or viral infection, neurotoxic drugs, and tumors.
Causes of Recurrent Laryngeal Nerve Injury
Right recurrent laryngeal nerve injury arises from:
- Neck trauma
- Benign or malignant thyroid disease
- Carcinoma of the esophagus
- Surgical traumsa
- Subclavian artery aneurysm
- Idiopathic causes are usually viral neuritis
- Cervical lymphadenopathy
Left recurrent laryngeal nerve injury is likely to arise from:
- Trauma
- Thyroid diseases
- Thyroid and esophageal carcinomas
- Cervical lymphadenopathy
- Bronchogenic carcinoma. It is an important cause that must always be ruled out in the left recurrent laryngeal nerve injury
- Aortic aneurysm
- Enlarged left auricle
- Intrathoracic surgery
- Idiopathic
The most common cause is non-thyroid cervical surgery. Paralysis of the recurrent laryngeal nerve can be due to central causes affecting the vagus nerve; nucleus ambiguous, bulbar and pseudobulbar palsy, jugular foramen syndrome and parotid tumors. Other lesions can be due to demyelinating diseases, skull base tumors, cerebrovascular accidents.
Recurrent laryngeal nerve injury in the neck is due to thyroid tumors or surgery, cervical spine surgery, esophageal tumors and deep penetrating wounds to the neck.
Recurrent laryngeal nerve injury in the chest is due to cardiac surgery, lung cancer, pulmonary tuberculosis, oesophageal cancer, mitral stenosis and thoracic aortic aneurysm.
Bilateral recurrent laryngeal nerve paralysis can be a fatal emergency. It is mostly caused by thyroid and cervical surgery, trauma, endotracheal intubation, central brain disorders, diabetic neuropathy, organophosphorus poisoning, myasthenia gravis and neurodegenerative disorders e.g. poliomyelitis and amyotrophic lateral sclerosis.
Clinical Manifestations of the Recurrent Laryngeal Nerve Injury
The recurrent laryngeal nerve is responsible for motor innervation of the laryngeal muscles. Injury to the nerve leads to the loss of vocal folds adduction and abduction and subsequently their dysfunction during phonation, breathing and deglutition.
In unilateral nerve injury, the paralyzed cord is situated in the paramedian or partially lateral position which will not affect the airway patency, but will affect phonation and deglutition. However, phonation may be achieved with contralateral vocal fold compensation. Therefore, unilateral recurrent laryngeal nerve injury leads to hoarseness of voice and dysphagia that may improve and lead to asymptomatic presentations.
The airway is patent without obstruction due to the abduction of the vocal folds. A weak voice results from the escape of air from the partially closed glottis during phonation. Deglutition is impaired in glottis incompetence especially to fluids and with sensory loss in central lesions to the vagus nerve fibers.
In bilateral injury that is mostly sustained during surgery, there are more serious manifestations that may be witnessed as soon as after extubation.
Bilateral vocal folds paralysis leads to stridor, difficulty breathing and aspiration. The breathing can be mildly distressed or severely impaired with biphasic stridor. The positioning of the denervated vocal folds is close to the midline with narrow glottis opening. Phonation may still be preserved in bilateral paralysis, but with inadequate intensity. Preoperative assessment of the vocal folds functions is mandatory in every case for legal purposes. Postoperative assessment is also needed for early detection of malfunction, even if the patient is asymptomatic.
Diagnosis of the Recurrent Laryngeal Nerve Injury
Careful history taking to evaluate for the possible etiology. History can exclude heavy metal neurotoxicity e.g. lead and mercury, neurodegenerative disorders, alcoholism, diabetes and neurotoxic drugs e.g. phenytoin and isoniazid. Imaging of the head, neck, chest with an MRI/CT and esophagoscopy can be helpful to diagnose any neoplastic lesion affecting the nerve.
Examination of the vocal folds is achieved with an indirect or fiberoptic laryngoscope. The rigid laryngoscope is helpful in differentiating between neurogenic paralysis of the vocal folds and cricoarytenoid arthritis secondary to prolonged endotracheal intubation or rheumatoid arthritis.
Management of the Recurrent Laryngeal Nerve Injury
Unilateral nerve injury can be managed conservatively for up to 6 months to allow for spontaneous healing in case of neurapraxia. For total nerve transection during surgery, corrective surgery should be considered as early as possible. Surgical interventions include augmentation, medicalization and reinnervation to improve voice quality. Electromyography is considered to evaluate for spontaneous healing or the need for corrective surgery. Nimodipine is a drug that has been suggested for the treatment of idiopathic and iatrogenic unilateral and bilateral vocal fold paralysis without a total transaction. It helps with neuronal regeneration and recovery.
Vocal fold augmentation (injection laryngoplasty) involves transoral or transcervical injection of collagen, hyaluronic acid and autologous fat into the paralyzed cord. The result will bring the cord closer to the midline to prevent aspiration and improve phonation and cough.
Medialization thyroplasty is done by inserting an implant lateral to the paralyzed cord to bring it more medially. The implant is silicone or Gore-Tex implanted transcervical through thyroid cartilage. It is adjustable to allow tuning of the voice.
Reinnervation of the vocal folds using microsurgical techniques, but with limited success.
In the case of bilateral nerve injury, patients will need breathing assistance and airway reconstruction. Certain measures can be performed urgently including; permanent or temporary tracheostomy, endotracheal intubation and reinnervation. Posterior establishment of the airway through the glottis with laser cordectomy is the best for both breathing and phonation quality. Cordectomy is achieved via posterior transaction of the part of the cords and the arytenoid to establish an airway through the glottis. Some patients can benefit from lateralization of the vocal cords after arytenoidectomy, but the results of lateralization on phomation are not favorable.
Comentários
Enviar um comentário