Arteries of the Upper Limb
Table of Contents
Overview of the Arteries of the Upper Limb
The arterial supply of the upper limb is derived from the subclavian artery. The arch of aorta gives off three branches: brachiocephalic trunk left common carotid and left subclavian artery.
The right subclavian artery arises from the brachiocephalic trunk. Both the right and left subclavian arteries to divide further into branches and supply the right and left upper limb respectively. The first artery arising from the subclavian artery is the axillary artery.
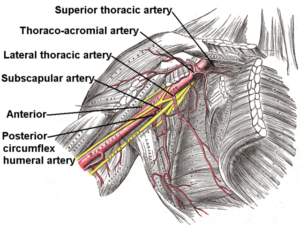
The Axillary Artery
As the subclavian artery crosses the lateral border of the first rib it becomes the axillary artery. The pectoralis minor muscle runs in front of the axillary artery and divides it into three parts. First part lies proximal to the muscle, the second part beneath it and the third part distal to it.
The first part of the artery gives rise to the superior thoracic artery, which supplies blood to the first and second intercostal muscles.
The thoracoacromial artery, arising from the second part nourishes pectoralis major, pectoralis minor, subclavius, and deltoid muscle. It also supplies blood to the shoulder joint.
Image: “Branches of axillary artery” by Häggström, Mikael. “Medical gallery of Mikael Häggström 2014”. Wikiversity Journal of Medicine 1 (2). DOI:10.15347/wjm/2014.008. ISSN 20018762. – Image:Gray523.png, License: Public domain
The lateral thoracic artery, which also arises from the second part of the axillary artery, supplies serratus anterior muscle, and the skin and fascia of the anterolateral thoracic wall.
The anterior circumflex humeral artery and the posterior circumflex humeral artery, both arising from the third part of the axillary artery anastomose around the neck of the humerus. Both of these arteries supply the deltoid muscle and other muscles around the surgical neck of the humerus.
The subscapular artery is the largest branch of the axillary artery, arising from its third part. It further divides into the scapular circumflex artery and thoracodorsal artery. The former supplies blood to the teres major, teres minor, and infraspinatus muscle. The later supplies to the latissimus dorsi muscle.
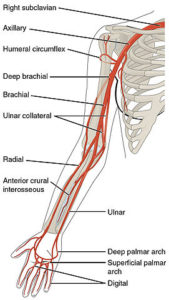
The Brachial Artery
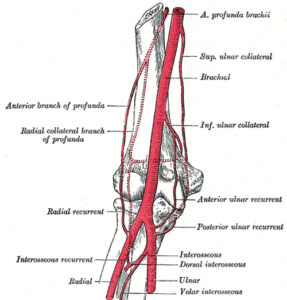
Image: “Arterial supply of arm and forearm” by Henry Vandyke Carter, Henry Gray (1918) in “Anatomy of the Human Body”. Bartleby.com: Gray’s Anatomy, Plate 526. License: Public Domain
As the axillary artery descends the lower border ofteres major muscle, it becomes the brachial artery. This also marks the lower border of the axilla.
The brachial artery runs down the arm to end at the neck of the radius, where it divides into radial and ulnar arteries. It usually runs a superficial course in the arm, just below the deep fascia and gives off its branches.
The profunda brachii artery is a deep branch of the brachial artery, passes posterior to the shaft of humerus and supplies the posterior compartment of the arm. It terminates by dividing into radial collateral and middle collateral arteries. The former supplies the medial part of triceps and anconeus muscles while the later supplies the lower lateral part of the arm. Both of them form a rich anastomotic network around the elbow joint.
The superior and inferior ulnar collateral arteries are branches of the brachial artery supplying the medial arm. Figure 2 demonstrates the arterial supply of arm and forearm with arterial anastomosis around the elbow joint.
The Radial Artery
The radial artery begins at the neck of the radius and passes laterally along the forearm. Proximally, it only has one branch, i.e., radial recurrent artery. As mentioned above, it anastomoses with the radial collateral artery and supplies the lateral side of the elbow. The further course of the radial artery is discussed below under palmar arches.
The Ulnar Artery
Image: “Course of ulnar artery” by Henry Vandyke Carter, Henry Gray (1918) in “Anatomy of the Human Body”. Bartleby.com: “Gray’s Anatomy”, Plate 529. License: Public Domain
The ulnar artery passes along the medial aspect of the forearm. The anterior and posterior ulnar recurrent arteries originate from the proximal part of the ulnar artery. They anastomose with the superior and inferior ulnar collateral arteries. Both of them supply the medial side of the elbow and proximal portions of the flexor muscles of the forearm.
As we move distally, the ulnar artery gives off another branch called common interosseus artery, which supplies the deep structures of the forearm and further divides into anterior and posterior branches.
The posterior branch gives off interosseus recurrent artery, which anastomoses with the middle collateral artery around the elbow joint.
The anterior interosseous artery supplies:
- Flexor pollicis longus
- Flexor digitorum profundus
- Pronator quadrates muscles
- Radius
- Ulna and carpal bones
The posterior interosseus artery supplies the following muscles of the posterior forearm compartment:
- Supinator
- Abductor pollicis longus
- Extensor pollicis longus
- Extensor pollicis brevis
- Extensor indicis muscles
Its interosseus recurrent branch nourishes elbow joint and anconeus muscle.
The ulnar artery, along with the radial artery, forms the palmar arches, which are discussed below.
The Palmar Arches
The radial and ulnar arteries give off branches to form superficial and deep palmar arches. The ulnar artery usually supplies the medial aspect of the index finger and the third, fourth and fifth finger. The thumb and the lateral half of the index finger are supplied by the branches given off by the radial artery.
The superficial palmar arch lies superficial to the flexor tendons and deep into the palmar aponeurosis. The deep palmar arch lies deep to the flexor tendons and above the metacarpal bones.
The palmar carpal branch of the ulnar artery anastomoses with the palmar carpal branch of the radial artery on the palmar surface of the hand.
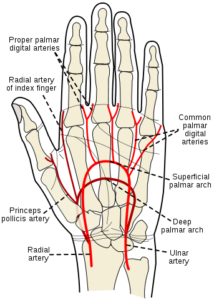
Image: “Superficial and deep palmar arches” by Rhcastilhos – Gray1237.png. License: Public Domain
The dorsal carpal branch of the ulnar artery anastomoses with the dorsal carpal branch of the radial artery on the dorsal surface of the hand and forms an arch. This arch gives off three dorsal metacarpal arteries, which further divide into dorsal digital arteries.
The deep palmar branch of the ulnar artery anastomoses with the branch of the radial artery to form the deep palmar arch. It supplies the deep palm, digits including the dorsum of the distal phalangeal segment.
The ulnar artery itself terminates by forming the superficial palmar arch. Here it anastomoses with the superficial palmar branch of the radial artery. It supplies the superficial palm, palmar surface of the digits excluding the thumb and the dorsum of the distal phalangeal segments of digits 2-5.
Common palmar digital arteries arise from the superficial palmar arch to supply the palmar aspect of two adjacent digits. These further divide into proper palmar digital arteries to supply the palmar aspect of each digit. These arteries also anastomose with the palmar metacarpal arteries, arising from the deep palmar arch.
The radial artery, after giving the superficial palmar branch, enters the dorsal surface of the hand, passes over the floor of the anatomical snuff box, gives off the dorsal first metacarpal artery and finally passes between the heads of the first interosseus muscles to re-enter the palmar aspect of the hand. It then gives the deep palmar branch, forming a deep palmar arch and two other branches called princeps pollicis and radialis indicis.
The Allen test is a medical sign used in the physical examination of the adequacy of the arterial blood flow to the hand. The modified version is commonly used. The test is used to identify adequacy of blood flow to the hand prior to cannulation of the radial artery for blood draw and continuous blood pressure monitoring. One hand is examined at a time.
The test is done as follows:
- The hand is elevated and the patient is asked to clench their fist for about 30 seconds.
- Pressure is applied over the ulnar and the radial arteries so as to occlude both of them.
- Still elevated, the hand is then opened. It should appear blanched (pallor may be observed at the fingernails).
- Ulnar pressure is released while radial pressure is maintained, and the color should return within 5 to 15 seconds.
If color returns as described, Allen’s test is considered to be “positive” or normal. If color fails to return, the test is considered “negative” or abnormal and it suggests that the ulnar artery supply to the hand is not sufficient. This indicates that it may not be safe to cannulate or needle the radial artery.

Comentários
Enviar um comentário