Anesthesia for Special Operations
In Lecturio - Anesthesia as a science has massively evolved from ether machines to sophisticated dedicated subspecialty branches, the progress of which equally parallels the booming advancement in corollary fields of surgery. This article encompasses discussion on thoracic anesthesia, endobronchial tube positioning, complications and other issues, cardiac anesthesia, and neuroanesthesia.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your anesthesiology course now for free!

Image: “Bronchoscopy.” by Unknown photographer – This image was released by the National Cancer Institute, an agency part of the National Institutes of Health, with the ID 1951. License: Public Domain
Thoracic Anesthesia
Thoracic anesthesia is one of the most complex anesthetic subspecialties evolved till date.Progress in lung isolation techniques, ventilation management, and pain control strategies have collectively culminated in the improved patient outcome. Airway management is continually improving as more sophisticated technological advances and devices improve the feasibility of lung isolation, ease surgical access, enhance intra-operative visibility and optimize access to the operative field.
Right or Left-lung anesthesia and Double-lumen endotracheal tubes (DLT)
Patients requiring thoracic surgery often require isolation of the right or left lung being operated upon during surgery. This leaves only one lung ventilated and it is vital that this lung is able to provide oxygenation and ventilation adequate to support life.Management of one lung anesthesia is one of the most difficult skills required by anesthesiologists.
Positioning of the endobronchial tube for right lung ventilation
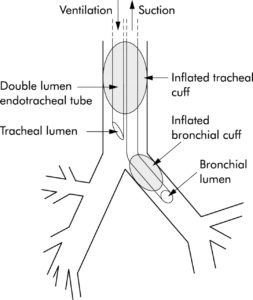
The right mainstem bronchus is shorter than the left and the distal cuff of a right endobronchial tube must be placed so ventilation occurs separately to the right and left lung. It is essential that both these tubes ventilate each bronchus separately. In cases in which a right lung resection is necessary, the left lung is ventilated, and the right is suctioned. Presence of leaks preventing positive pressure ventilation is a complication that may be difficult to handle and may lead to hypoxia.
The anesthesiologist must be an expert at using a fiber-optic bronchoscope to position the tube.
Bronchial blocker
An endobronchial blocker is a device which can be inserted down a tracheal tube after tracheal intubation so as to block off the right or left main bronchus of the lungs in order to be able to achieve a controlled one-sided ventilation of the lungs in thoracic surgery. The lung tissue distal to the obstruction will collapse, thus allowing the surgeon’s view and access to relevant structures within the thoracic cavity.Bronchial blockers are used to achieve lung separation and one lung ventilation as an alternative to double-lumen endotracheal tubes (DLT) and are the method of choice in children and pediatric patients for whom even the smallest DLTs might be too big.
Again, the use of a fiber-optic bronchoscope is essential for positioning of the blocker.
Complications and other issues
Any subspecialty is inevitably accompanied by its fair share of complications and controversies. Thoracic anesthesia is no exception. The potential problems can be tabulated as follows:| Complications | Explanation |
| Dislodgement of the endobronchial tube or blocker | Common complication, aggressive use of a bronchoscope to reposition is the key |
| Hypoxemia (low oxygen in the blood) | It can be minimized by correct tube placement and the addition of PEEP to the non-operated lung and CPAP to the operated lung. |
| Massive hemorrhage | Blood can contaminate the ventilated lung impairing gas exchange. |
| Post-operative ALI | Potentially lethal complication |
| Post-operative pain management | Post-operative pain is the worst of its genre in thoracic surgery patients. Consequently, they tend to splint their chests during respiration leading to decreased air entry in the lungs and higher chances of collapse, atelectasis, and infection. The placement of a thoracic epidural for pain relief allows patients to be comfortable, ambulate early and deep breath and cough when necessary. |
Cardiac Anesthesia
Cardiac anesthesia with cardiopulmonary bypass sets a unique challenge for the anesthetist’s task of ensuring analgesia, amnesia, and adequate muscle relaxation.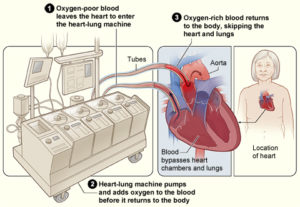
Image: “The image shows how a heart-lung bypass machine works during surgery.” by National Heart Lung and Blood Institute (NIH). License: Public Domain
Cardio-pulmonary bypass (CPB)
The cardio-pulmonary bypass is a testimony to the progress of medical science. However, its use is not free of complications. CPB results in pharmacodynamic and pathophysiologic changes that perturb the usual homeostasis of the body. Here are some examples:- Postperfusion syndrome (also known as “pump head”)
- Hemolysis
- Capillary leak syndrome
- Clotting of blood in the circuit – can block the circuit (particularly the oxygenator) or send a clot into the patient.
- Air embolism
- Leakage – a patient can rapidly exsanguinate (lose blood perfusion of tissues) if a line becomes disconnected.
These complications can make CPB a tantalizing challenge.
The cardiopulmonary bypass machine allows the patient’s blood to bypass the heart and lungs during surgery but is pumped back into the patient to assure perfusion to other organs. The heart is at a standstill during bypass allowing the surgeon to work on a stable target. For certain procedures such as valvulotomy and coronary bypass, some surgeons prefer to operate on a beating heart.
The anesthesiologist is usually responsible for maintaining the patient during CPB. Coming off bypass (a critical period in the surgery) is managed by the anesthesiologist.
Left ventricular assist device (LVAD)
The concepts of “destination therapy”, permanent use of an LVAD as a treatment modality for advanced heart failure versus “bridge” therapy as a transition to heart transplant demand specific expectations of the anesthesiologist. Significant issues are summarized as follows:| Issue | Explanation |
| Induction of LVAD flow | May unveil right ventricular dysfunction demanding aggressive management, sometimes to the extent that an RVAD might be indicated as well |
| Recirculation forced by aortic insufficiency | Acutely stress the flow capacity of the LVAD and also reduce its potential functional life |
| Systemic ‘‘vasoparesis” | May necessitate the administration of adrenergic agonists, vasopressin, or methylene blue to achieve optimal systemic arterial pressures |
| Complex coagulation disturbances with subsequent re-exploration for bleeding | Not infrequent in the early postoperative period |
Valves
Valve replacement procedures have stood the test of time and are generally safe, less morbid, and standardized. Any superiority of a particular genre of the valve is equivocal. Post-operative management depends on the valve type used. The important differences can be summarized as follows:| Valve type | Benefits | Risks |
| Metal valves | Longevity: last around 20 years | Lifelong anticoagulation is needed, to prevent strokes and embolic phenomena |
| Tissue valves | Short lifespan: last about 10 years | Anticoagulation is not needed. |
Anesthetic responsibilities
The need for near-continuous TEE combined with the anticipated duration of the procedure favors general endotracheal anesthesia.
Cardiac anesthesia exists to ensure the absence of bradycardia, vasoconstriction, optimum fluid management and observant monitoring.
Short-acting, potent, inhalational anesthetics are preferred; neuromuscular blockers are not necessary. Need for inotropic agents frequently arises prior to bypass and coming off bypass.
When reversed from the bypass, unstable vital parameters often demand intensive care unit transfer. These patients are usually ventilated electively and transferred to floor only once stable.
Complications
Cardiac surgery and CPB used to be a very morbid affair in the not too distant past. Advances in technological know-how and better optimization of the heart while on CPB have dramatically changed the picture. Significant complications are as tabulated below:| Complication | Explanation |
| Failure to come off bypass | This is now relatively rare but used to cause many deaths. |
| Heart failure coming off bypass | May require LVAD or RVAD |
| Massive hemorrhage both from the use of anticoagulants and the effects of the CPB device | Nearly lethal |
| Cardiac arrhythmias, particularly atrial fibrillation | Early detection followed by aggressive rapid reversal is critical. |
| Cardiac tamponade | Potentially life-threatening, immediate correction of the utmost essence; usually requires the transport of an unstable patient back to the OR. |
| Pain from sternal movement post-operatively | Occasionally severe; requires treatment |
| Recall during anesthesia | Much less frequent during modern anesthesia; the use of high doses of opioids for this surgery must be accompanied by amnestic drugs. |
| Cardiac arrest in the OR or the CSICU | he chest should be opened and open cardiac massage employed; external cardiac massage on an unstable chest wall is ineffective. |
| Heart block | Requires the insertion of a pacemaker. |
Neuro-Anesthesia
Most neurosurgical procedures require general anesthesia but few can be done with deep sedation.The most critical aspect of neuro-anesthesia is control of intracranial pressure (ICP).
If ICP is lowered too aggressively, cerebral blood flow can be reduced and ischemic brain damage can occur.
| Drug | Effect on cerebral blood flow | ICP |
| Vapors | Increase | Increase |
| Propofol | Decrease | Decrease |
| Ketamine | Increase | Increase |
| Etomidate | Little effect | Decrease |
| Narcotics | Little effect | Little effect |
Osmotic diuretics (mannitol) and loop diuretics (furosemide) reduce water load of the brain and can be utilized as cerebral decongestants.
Role of local anesthesia and sedation in neuro-anesthesia

Image: “Deep brain stimulation in a Parkinson’s patient.” by Hellerhoff – Own work. License: CC BY-SA 3.0
More modern procedures (e.g. deep brain stimulation for patients with Parkinson’s disease) can be done with virtually nothing except local anesthesia and a little sedation. The surgeon inserts probes deep into the brain and stimulates ganglia associated with Parkinson’s disease.
Complications of neuroanesthesia
Neuroanesthesia is an unforgiving branch. One needs to maintain the critical equation between intracranial pressure and cerebral perfusion. Complications are as follows:| Complication | Explanation |
| Massive hemorrhage | Very difficult to treat |
| Cerebrovascular accidents (strokes) | Often lead to permanent morbidity |
| Failure to awaken from anesthesia | A thorough search for a surgical cause and/or a disease cause and/or anesthetic cause must be sought. |
| Increased ICP | Permanent damage to the brain |
| Issue | Explanation |
| Airway management in acromegalic patients | Acromegaly is characterized by macroglossia, prognathism, and hypertrophy of pharyngeal and laryngeal tissues, which lead to mask fit, mask ventilation, laryngoscopy, and correct tracheal tube placement may be difficult. Mallampati classification, that uses degrees of visualization of the pharynx when the patient opens his/her mouth, is used for objective assessment and further management. |
| Neuroendoscopic procedures | Cardiac arrhythmia, hemodynamic changes, cranial nerve dysfunction and intracranial hemorrhage are the anesthetic concerns. |
| Sitting position | Strongly fallen out of favor in many places; cerebral hypoperfusion, pneumocephalus, venous air embolism with hypotension are potential issues. |
| Intracranial lesions located around the speech areas | Fascinating and equally challenging; “awake craniotomy” is often used in these patients. |
| Pain management | Brain lacks pain receptors, but the rich innervation of the skin, periosteum of the skull, and the meninges demolish the old belief that minimal pain management is required in intracranial surgeries. |
Summary
Anesthesia has outgrown its conventional form to encompass various specialties which demonstrate parallel development and progressed as their surgical counterparts.One of the most complex branches, thoracic anesthesia, involves one-lung ventilation, use of endobronchial tubes and blockers and pain management.
Cardiac anesthesia revolves around preservation of heart during the use of CPB machine. Recall during cardiac surgeries is the modern cardiac anesthesiologist’s nightmare.
Neuroanesthesia is as unforgiving and subtle as neurosurgery. The issues are specific and demand customized management.
All these specialized sections of anesthesia abound with complications but one needs to exercise constant vigilance and aggressive management to ultimately bring about effective patient care.
Review Questions
The correct answers can be found below the references.1. Which of the following is true regarding management of dislodged endobronchial tube?
- Remove the tube immediately to avoid atelectasis.
- Remove the tube immediately to avoid hyperinflation.
- Use of bronchoscope solves the problem.
- Do not do anything as it is not significant.
- Potent amnestic agents
- Opioids
- Adequate liquids preoperatively
- Neuromuscular blockers
- Wilson classification
- Murthy classification
- Acromegaly assessment protocol
- Mallampati classification
Comentários
Enviar um comentário