Physiological Effects of Estradiol and Progesterone & Menstrual and Endometrial Cycle
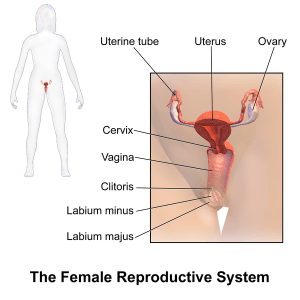
In Lecturio - The female reproductive system consists of two ovaries, two fallopian tubes, the uterus, cervix and external genitalia. Every female undergoes a monthly cycle of 28 days, in which an egg is released from either ovary and the lining of the uterus is prepared for the implantation of an embryo, which eventually sheds off in case fertilization does not occur. This normal physiological mechanism is controlled by a number of hormones, secreted by the hypothalamus, pituitary gland and ovaries themselves. Any aberration in the release of these hormones may result in menstrual cycle abnormalities or infertility.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your pathology course now for free!
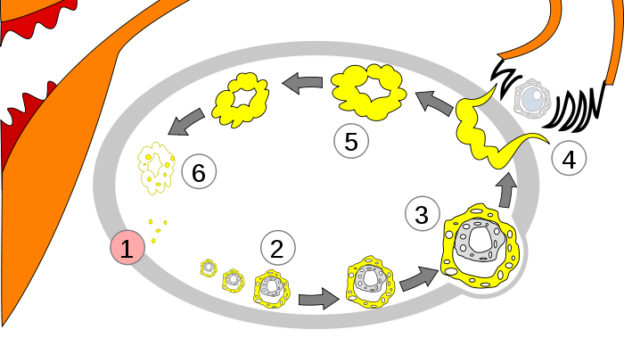
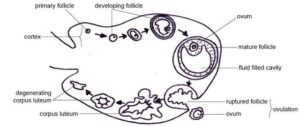
Image: “Order of changes in ovary.” License: CC BY-SA 3.0
The Role of Estradiol
The ovaries secrete two main hormones which play their role in the female reproductive cycle. They are estradiol (estrogen) and progesterone.Estradiol is the most common type of estrogen in females of reproductive age. During childhood, the amount of estradiol secreted by the ovaries is minimal. However, as the puberty is reached, its secretion increases to 20-folds.
This occurs under the influence of pituitary gonadotropic hormones. Estradiol has an important role in the development of primary and secondary female sexual characteristics, some of which are highlighted below:
An overall increase in the size of female reproductive organs and external genitalia. It causes deposition of fat in mons pubis and labia majora. There is also an enlargement of labia minora.
The vaginal epithelium changes from cuboidal to stratified epithelium. This provides resistance to external stress. Young female children who have repeated genital tract infections are often prescribed estrogen creams for local application to provide resistance against infections.
The size of the uterus increases to 3-folds. There is a marked proliferation of endometrial stroma and development of endometrial glands during each menstrual cycle.
The glandular tissues in fallopian tube proliferate with an increase in the number of ciliated epithelial cells. The cilia become more active and propel the ovulated egg towards the uterus. This maximizes the chances of fertilization.
Breast enlargement occurs under the influence of estradiol. There is deposition of fat, and the development of stromal tissues and the ductile system. Estradiol however, does not cause milk production in breasts.
The osteoblastic activity increases in the bones under the influence of estradiol. This causes an overall increase in height during puberty. There is also an early union of epiphyses with the shaft of long bones. The increase in the height of females, therefore, ceases after a few years as compared to males. Osteoporosis in older females after menopause is due to the deficiency of estrogen. Hormone replacement therapy (HRT) is the treatment option given to such females.
The total body protein increases as a result of an enlargement of the sexual organs. At a cellular level, it causes an accelerated rate of transcription of RNA, for the synthesis of new proteins.
The vascularity of skin increases. Estradiol also gives a soft texture to the skin. The hair distribution on the skin is not mainly affected by estrogens, but is controlled by the androgens produced by the adrenal glands.
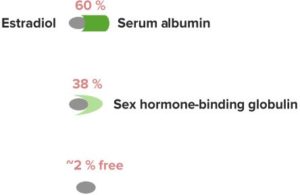
“Transport in the Blood” Image created by Lecturio
Estrogen receptors can be the traditional cytosolic-nuclear complex variety (as in other steroid hormones) or less commonly, a cell-membrane variety.
Estradiol Effects
| Tissue | Effect |
| Bone | ↑ Growth via osteoblasts |
| Endocrine | ↑ Progesterone responses |
| Liver |
|
| Reproductive organs |
|
The Role of Progesterone
Progesterone is another important ovarian hormone playing its role in the female reproductive cycle. The following are its major roles:It promotes the secretary functions of the uterine endometrium. This prepares the endometrium for implantation of the fertilized ovum in the second half of menstrual cycle.
The secretory functions of the lining of the fallopian tubes are also enhanced, to nourish the dividing zygote after fertilization.
The development of lobules and alveoli of the breasts is regulated by progesterone. These lobules and alveoli become secretory in nature. However, they are unable to produce milk without the action of the prolactin hormone.
Progesterone in large amounts may enhance the reabsorption of sodium, chloride, and water from the distal tubule of the kidney.
Progestin Effects
| Tissue | Effect |
| Breast |
|
| Reproductive organs |
|
| Temperature | ↑ Internal temperature |
The Endometrial and Ovarian Cycle
The endometrial cycle is an average cycle of 28 days in the females of reproductive age, characterized by the shedding of the endometrial lining of the uterus. This process of loss of endometrial lining is called menstruation.Another important event occurring during this cycle is the release of mature follicle or egg from one of the two ovaries. This is known as ovulation. Both menstruation and ovulation occur under rhythmic control of hypothalamic, pituitary and ovarian hormones.
The female menstrual cycle primarily consists of two phases – the proliferative phase and the secretory phase. This may be followed by menstruation if fertilization does not occur.
The proliferative phase (estrogen phase)
The primordial follicle, in which the ovum is surrounded by a single layer of granulosa cells, remains inhibited by the oocyte-maturation inhibiting factor in childhood.At puberty, when the pituitary gland starts producing luteinizing hormone (LH) and follicle-stimulating hormone (FSH), the process of follicular growth is initiated. FSH causes an increase in the number of granulosa cell layers around the ovum, converting it to the primary follicle. It is responsible for the growth of 5 – 6 primary follicles each month. The rise of FSH precedes LH by a few days. Many spindle cells from the interstitium of the ovary surround the granulosa cells to form a layer of cells called theca.
Theca divides into two layers – theca interna and theca externa. The theca externa becomes the outer capsule of the developing follicle. After the initial few days, the granulosa cells secrete a follicular fluid that forms the antrum. This follicular fluid secretes estrogen hormone. Estrogen increases the FSH receptors on granulosa cells, thereby creating a positive feedback response.
After a week of initial growth, one growing follicle outgrows all others. The other follicles undergo atresia. The one follicle that is left behind starts producing more estrogen. This causes a surge in LH which leads to release of an egg from the ovary, at around day 14 of the cycle.
After the previous menstruation, most of the endometrial lining is desquamated and only a deep layer is left behind. Under the influence of estrogen, secreted by the ovaries, the stromal cells and the epithelial cells proliferate.
The endometrial thickness is regained within 4 – 7 days following menstruation. There is an increase in the number of stromal cells, the growth of endometrial glands and increased vascularity. This continues to occur until ovulation occurs, during which it is approximately 3 – 4mm in thickness. When ovulation occurs, the cervical glands secrete thin, stringy mucus which forms channels to direct sperm towards the uterus.
The secretory phase (progesterone phase)
After the ovulation has occurred, corpus luteum is formed in its place that consists of granulosa and theca cells. This corpus luteum secretes both estrogen and progesterone in large quantity. While estrogen causes further proliferation of the stromal cells of the epithelial lining of the uterus, progesterone is responsible for the secretory development of the cells.The blood supply to the endometrium increases and the blood vessels become increasingly tortuous. The ‘uterine milk’ secreted by the endometrium nourishes the fertilized ovum. In addition, there is lipid and glycogen deposition in the stromal cells cytoplasm. The endometrium is thus prepared for the implantation of the developing embryo.
If implantation occurs, the trophoblastic cells lining the blastocyst digest the endometrial cells and absorb these stored substances. The lining of the endometrium at the end of the secretory phase is 5 – 6mm thick. The figure illustrates the developmental stages of the ovarian follicle.
Menstruation
The levels of estrogen and progesterone decline 2 days prior to the end of menstrual cycle. The hormonal effect on the endometrial lining diminishes. It is followed by the involution of the endometrium to 65% of its previous thickness. This causes vasospasm of the tortuous blood vessels. Prostaglandins, which are released in higher quantity at this stage, are also responsible for the vasospastic response.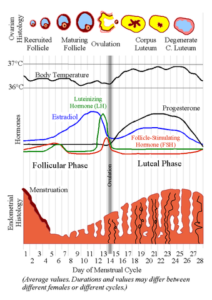
Image: “Female Menstrual Cycle.” by Lyrl – Derived from Image: MenstrualCycle.png, an image made by the user Chris 73. License: CC BY-SA 3.0
During menstruation, approximately 40ml of blood and 30ml of serous fluid is lost. The fibrinolysin present in blood prevents clotting of blood. However, if excessive bleeding occurs, the fibrinolysin becomes insufficient and clots of blood may be seen. The normal menstrual blood flow lasts for 3-7 days.
Leukorrhea during menstruation is a normal physiological phenomenon which prevents infection. The endometrium becomes resistant to micro-organisms despite being denuded. The figure gives a detailed account of the female menstrual cycle.
Regulation of the Female Menstrual Cycle
There is an interplay between the ovarian and hypothalamic-pituitary hormones, summarized below:The hypothalamus is connected to the pituitary gland through the hypothalamic-hypophyseal portal system. The former secretes gonadotropin-releasing hormone (GnRH) in a pulsatile manner. This, in turn, results in the pulsatile release of luteinizing hormone (LH) by the pituitary gland. To some extent, follicle stimulating hormone (FSH) is also influenced by the pulsatile manner of GnRH; however, the effect is more prolonged.
Estrogen initially has a suppressive effect on FSH and LH, but just before ovulation, the amount of FSH secreted by the pituitary gland increases 2-folds while LH increases by 6-folds. This is known as LH surge and is mandatory for ovulation to occur. Estrogen is thought to play positive feedback.
After ovulation has occurred, progesterone and estrogen secreted by corpus luteum have a negative feedback effect and decrease the production of LH and FSH. However, just before menstruation, when the corpus luteum involutes, the levels of estrogen and progesterone begin to fall. This will reinitiate the production of FSH and LH for the next cycle.
Inhibin is another hormone that works synergistically with estrogen and progesterone in lowering the production of FSH. However, it does not have a significant role in lowering the amount of GnRH released by the hypothalamus.
Menstrual/Ovarian Cycle Disorders
- Anovulation is the absence of ovulation. These cycles occur during the first few cycles of puberty or prior to menopause. They may also occur in polycystic ovarian syndrome (PCOS) and is the most common cause of primary infertility among females.
- Oligo-ovulation means irregular ovulatory cycles.
- Amenorrhea is the absence of menstruation. It is either primary in which the female has never menstruated, or secondary in which there is a cessation of menstruation after the start of normal menstruation.
- Oligomenorrhea refers to scanty menstrual flow with cycle length exceeding 35 days.
- Polymenorrhea is frequent menses with each cycle lasting <22days.
- Menorrhagia is excessive menstrual bleeding.
- Dysmenorrhea is lower abdominal pain during menstrual cycle.
Review Questions
The correct answers can be found below the references.1. A 17-year-old female came with a complaint of discharge from the genital tract for a few days, along with a low-grade fever with chills. Her vitals are HR 110/min, RR 25/min, BP 100/70 mmHg and temperature 99 F. On local examination, a whitish fowl smelling discharge was seen coming out from the genital tract. There is also a history of similar infection twice in the last 6 months. A cream for local application, containing which of the following, must be advised for treatment?
- Progesterol
- Estradiol
- Misoprostol
- Lignocaine with bacitracin
- Oligimenorrhea; Endometriosis
- Polymenorrhea; dysmenorrhea
- Amenorrhea; Amyloidosis
- Menorrhagia; dysmenorrhea
- Decreased estrogen; increased testosterone and androstenedione
- Increased estrogen and decrease progesterone
- Increased progesterone and decreased testosterone
- Increased prolactin, GnRH and LH
- Polycystic ovarian syndrome
- Cushing disease
- Cushing syndrome
- Posterior Pituitary adenoma
Comentários
Enviar um comentário