Gastrointestinal Motility: Gastric Motility and Intestinal Motility
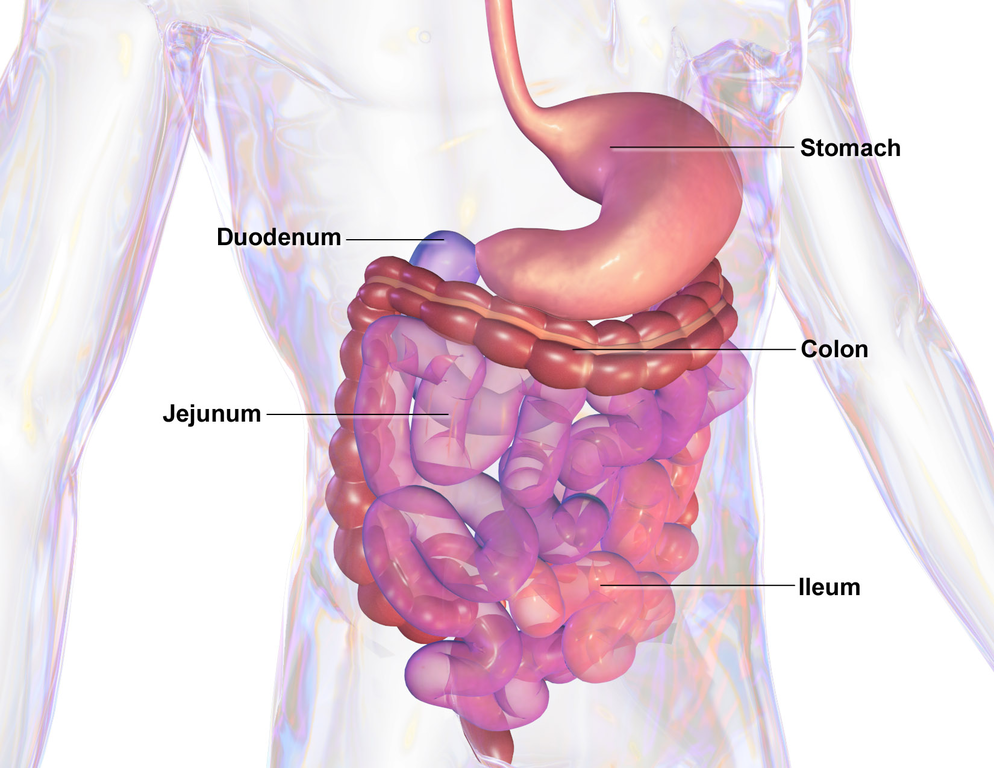
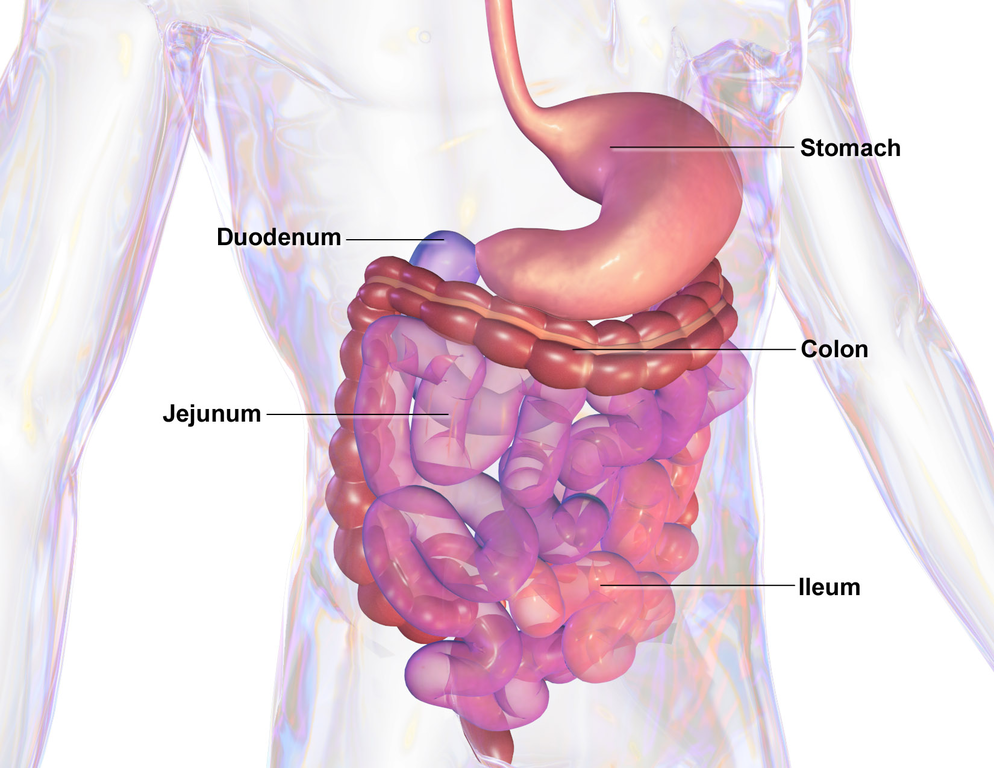
In Lecturio - Gastrointestinal motility is one of the major roles played by the alimentary canal. In the esophagus, it serves to get the ingested bolus of food from the oropharynx to the stomach. In the stomach, this motility is responsible for the churning and mixing of food and turning it into chyme. This continues in the small and large intestines until the digested food can be excreted out of the anus. There are various anatomical and physiological components of gastrointestinal motility. It is very important for medical students and healthcare professionals to have a clear clinical understanding of these components.
The sympathetic nervous system is inhibitory in function, and consists of fibers arising from the spinal cord portions of T8–L2.
 Apart from the pharynx, the upper 1/3 of the esophagus and the external anal sphincter (which consists of striated muscles), the rest of the gastrointestinal tract contractility is dependent on smooth muscles.
Apart from the pharynx, the upper 1/3 of the esophagus and the external anal sphincter (which consists of striated muscles), the rest of the gastrointestinal tract contractility is dependent on smooth muscles.
A Circular layer of muscles contracts to reduce the diameter of the lumen of the GI tract. Longitudinal muscles contract to shorten the segment of the GI tract.
Peristalsis is caused by the myenteric plexus; it is described as the formation of a ring due to muscle contractility that pushes intestinal contents in a forward direction (towards the anus). This ring is formed by muscle contraction above and relaxation distal to the bolus of food being moved. The contraction is due to the release of acetylcholine (a depolarizing factor), whereas the relaxation is due to the release of nitric oxide and vasoactive peptide.
Extrinsic nervous signals (parasympathetic nervous system), distention and irritation, lead to peristalsis.
 Two neurocrines are responsible for the relaxation and contraction of GI sphincters. They are synthesized in the neurons found in the GI tract, and travel down the axon to be realized at the end of the nerves by action potential. These two neurocrines are vasoactive intestinal peptide and enkephalins.
Two neurocrines are responsible for the relaxation and contraction of GI sphincters. They are synthesized in the neurons found in the GI tract, and travel down the axon to be realized at the end of the nerves by action potential. These two neurocrines are vasoactive intestinal peptide and enkephalins.
Vasoactive intestinal peptide is homologous to the hormone Secretin and contains 28 amino acids. It works to relax GI smooth muscles, especially the lower esophageal sphincter. Enkephalins work especially to cause contraction in the smooth muscles, making up the sphincters of the GI tract.
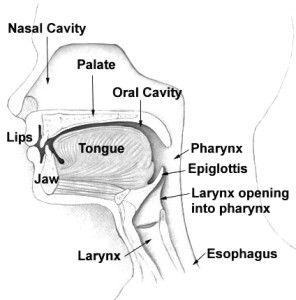 Swallowing or deglutition is a reflex phenomenon through which ingested food is passed from the mouth to the pharynx and esophagus and eventually into the stomach.
Swallowing or deglutition is a reflex phenomenon through which ingested food is passed from the mouth to the pharynx and esophagus and eventually into the stomach.
This reflex is regulated by the medulla. Signals are carried by the fibers of the vagus and glossopharyngeal nerves to and from between the receptors of the GI tract and the medulla, and then to the muscles involved in swallowing.
Deglutition can be divided into one voluntary and one involuntary stage.
Stage 1 – Voluntary Stage
This phase involves the bolus of the food being pushed backward and upwards towards the palate by the tongue. This way the bolus is pushed by the tongue into the pharynx.
Stage 2 – Pharyngeal Stage (Involuntary)
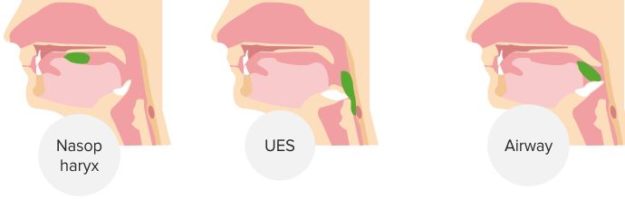
This is an elaborate phase that follows a specific sequence. When the bolus of food comes in contact with the swallowing receptors on the opening of the pharynx and the tonsillar pillars at the back of the mouth, signals are sent to the medulla, and, as a result, the soft palate is pulled upwards, closing the nares and inhibiting breathing. Furthermore, the palatopharyngeal folds move medially towards each other forming a vertical slit that only lets properly masticated food through and blocks bigger food particles. This reduces the chance of choking.
In addition to this, the laryngeal muscles contract which results in the closing of the glottis and the elevation of the larynx. Elevation of the larynx stretches opens the upper esophageal sphincter, allowing the bolus of the food to be transmitted from the pharynx into the esophagus. This is followed by a peristaltic wave starting due to the contraction of the superior constrictor muscles of the pharynx.
There are three-factor aspects of this stage:
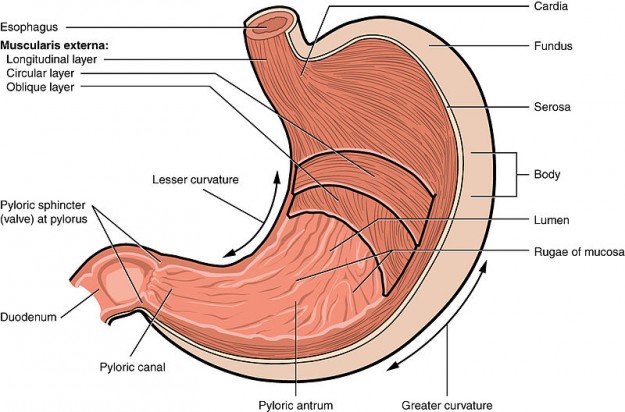 Gastric motility can be understood better when divided into three stages:
Gastric motility can be understood better when divided into three stages:
1. Receptive Relaxation
When the bolus of food enters and causes distention of the stomach, a vagovagal reflex is initiated that causes relaxation of the orad region of the stomach, hence accommodating the ingested food.
2. Mixing and Digestion
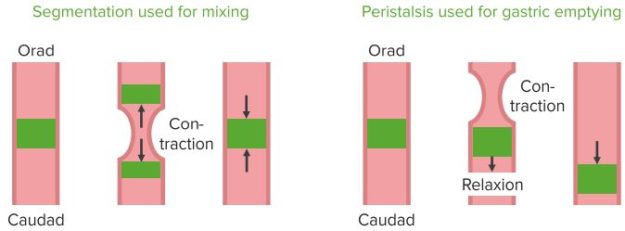
This occurs in the caudal region of the stomach and involves two types of waves:
Slow/weak peristaltic constrictor waves – these waves are regulated by basic electric rhythm and occur every 3–5 minutes. Their function is to mix the gastric secretions and the food together and weak propulsion.
Powerful peristaltic constrictor rings – this causes the contraction of the distal antrum, so when the weak peristalsis waves propel food towards the distal antrum, the power constrictor waves causes it to be propelled back (retropropulsion) therefore mixing the food in the process.
3. Gastric Emptying
Two factors controlling the emptying of the stomach contents into the duodenum are the pylorus (which is usually tonically contracted, therefore controls stomach emptying) and antral peristalsis or pyloric pump (the peristaltic movements that cause the propulsion of chyme into the duodenum).
 Factors that affect Gastric emptying:
Factors that affect Gastric emptying:
Stomach contents: the types of food in the stomach can influence gastric emptying, for example, presence of fat in the stomach contents slows down gastric emptying because of the production of a hormone called Cholecystokinin. Cholecystokinin is produced by the I cells of duodenal and jejunal mucosa in response to the presence of fatty acids and monoglycerides, as well as amino acids. Its function is to inhibit and slow down gastric emptying so that more time can be spent digesting and absorbing food in the small intestines.
Similarly, fastest gastric emptying takes place when the gastric contents are isotonic in nature, whereas hypertonic (high osmolality) or hypotonic (low osmolality) stomach contents slows it down.
Other hormones that inhibit gastric emptying include secretin and gastric inhibitory peptide. The condition of the duodenum has a strong influence over stomach emptying as well. Its distention, irritation, acidity and presence of fat slow down gastric emptying. Increased volume of food stimulates the local and vagal myenteric reflexes that result in the increased activity of the pyloric pump and the relaxation of the pylorus.
Gastrin is another hormone that is released in response to the distention of the stomach walls due to increased food volume. It also increases the activity of the pyloric pump and relaxes the pylorus.
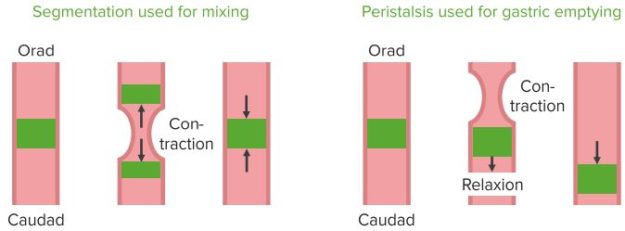
Parasympathetic stimulation increases contractions, whereas the sympathetic nervous system decreases them. There are two types of movements involved in small intestine motility.
Segmentations: When a portion of the small intestines receive chyme and gets distended, a localized response consisting of concentric contractions takes places. These are located at varying intervals throughout the small intestine, hence giving a “segmented” appearance. They work to mix the chyme so the nutrients can be absorbed better.
Peristalsis: They work to propel chyme forward.
Peristaltic rush is a phenomenon seen in the case of intestinal irritation (such as diarrhea) which consists of a very strong and rapid peristaltic wave that sweeps all intestinal contents and deposits them in the colon within one minute. It occurs so the small intestine mucosa can be relieved of the irritating contents.
Migrating motor complex is a peculiar pattern of activity experienced in an empty stomach and small intestines. It consists of slow and rhythmic peristaltic activity that sweeps down the stomach and small intestine every 1.5 – 2 hours to get excess content and secretions into the colon so they don’t build up.

1. A 26-year-old medical student participates in a research about intestinal motility. On further investigation, which of the following part of his gastrointestinal tract will show “segmentation” as a part of motility?
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your gastrointestinal pathology course now for free!
Histology of the Gastrointestinal Tract
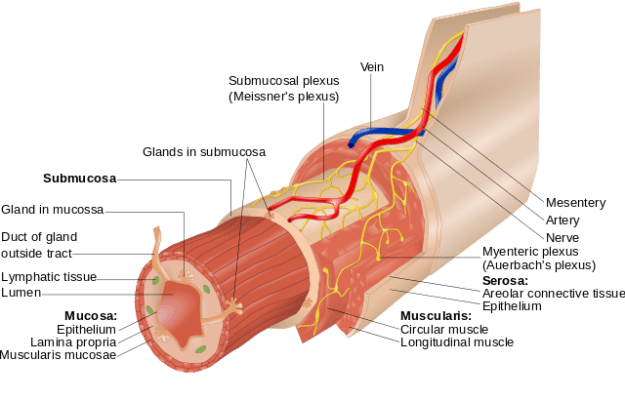
Histology of the gastrointestinal tract helps us understand the underlying mechanisms responsible for gastrointestinal motility. Although there may be some histophysiological variations, the general histology of the gastrointestinal tract consists of the following layers (innermost to outermost):- Mucosa – containing the epithelium and an underlying lamina propria made up of loose connective tissue
- Submucosa – made up of dense connective tissue; contains the Meissner’s plexus and esophageal proper glands in the esophagus and Brunner glands in the duodenum
- Muscularis externa – made up of an inner circular and outer longitudinal layer of smooth muscles; Aeurbach’s/Myenteric plexus is located between the two layers of muscles
- Serosa (last layer of organs covered by peritoneum) or adventitia (last layer of organs not covered by the peritoneum)
Note: Serosa is a serous membrane made up of two layers of epithelial cells whereas adventitia is a thin layer of connective tissue.
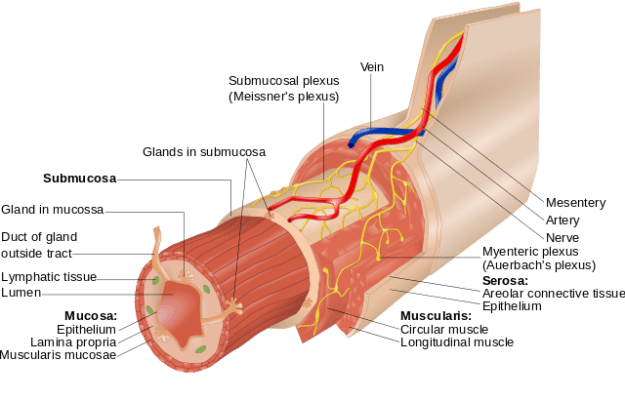
Image: “Layers of the Alimentary Canal. The Wall of the Alimentary Canal has Four Basic Tissue Layers: the Mucosa, Submucosa, Muscularis, and Serosa.” by Goran tek-en. License: CC BY-SA 3.0
Gastrointestinal Tract Innervation
Gastrointestinal innervation is of two types: extrinsic innervation and intrinsic innervation.Extrinsic Innervation
It is made up of parasympathetic and sympathetic nervous systems consisting of efferent and afferent fibers. The parasympathetic nervous system is excitatory in function and consists of Vagus (from esophagus to the first 2/3 of transverse colon) and pelvic nerves (from the last 1/3 of transverse colon up to the anus).The sympathetic nervous system is inhibitory in function, and consists of fibers arising from the spinal cord portions of T8–L2.
Intrinsic Innervation
It is composed of myenteric (Auerbach’s) and submucosal (Meissner’s) plexuses. The myenteric plexus majorly controls the motility of the smooth muscles of the gastrointestinal tract. The Meissner’s plexus controls GI secretions and the local blood flow, as well as receiving sensory input from the chemoreceptors and mechanoreceptors on the mucosa.Peristalsis
Image: “An animated image to show Peristalsis” by Auawise. License: CC BY-SA 4.0
A Circular layer of muscles contracts to reduce the diameter of the lumen of the GI tract. Longitudinal muscles contract to shorten the segment of the GI tract.
Peristalsis is caused by the myenteric plexus; it is described as the formation of a ring due to muscle contractility that pushes intestinal contents in a forward direction (towards the anus). This ring is formed by muscle contraction above and relaxation distal to the bolus of food being moved. The contraction is due to the release of acetylcholine (a depolarizing factor), whereas the relaxation is due to the release of nitric oxide and vasoactive peptide.
Extrinsic nervous signals (parasympathetic nervous system), distention and irritation, lead to peristalsis.
Tonic Contraction of Sphincter
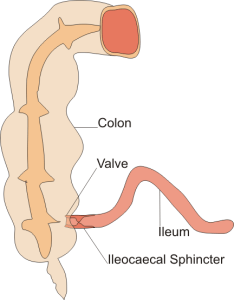
Sphincters of the GI tract experience tonic contraction, that is, contractions can be maintained for longer intervals. It is caused by repetitive spike potentials, constant release of depolarizing hormones and continuous entry of calcium ions. Sphincters of the GI tract, that function this way, include the lower esophageal sphincter, Ileocecal sphincter, pyloric sphincter and external anal sphincter.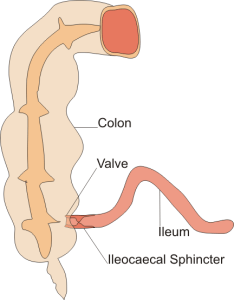
Image: “Diagram of Ileocecal Valve and Sphincter” by Boumphreyfr. License: CC BY-SA 3.0
Vasoactive intestinal peptide is homologous to the hormone Secretin and contains 28 amino acids. It works to relax GI smooth muscles, especially the lower esophageal sphincter. Enkephalins work especially to cause contraction in the smooth muscles, making up the sphincters of the GI tract.
Swallowing
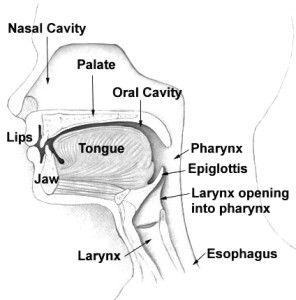
Image: “Head and Neck Overview” by Arcadian. License: Public Domain
This reflex is regulated by the medulla. Signals are carried by the fibers of the vagus and glossopharyngeal nerves to and from between the receptors of the GI tract and the medulla, and then to the muscles involved in swallowing.
Deglutition can be divided into one voluntary and one involuntary stage.
Stage 1 – Voluntary Stage
This phase involves the bolus of the food being pushed backward and upwards towards the palate by the tongue. This way the bolus is pushed by the tongue into the pharynx.
Stage 2 – Pharyngeal Stage (Involuntary)
This is an elaborate phase that follows a specific sequence. When the bolus of food comes in contact with the swallowing receptors on the opening of the pharynx and the tonsillar pillars at the back of the mouth, signals are sent to the medulla, and, as a result, the soft palate is pulled upwards, closing the nares and inhibiting breathing. Furthermore, the palatopharyngeal folds move medially towards each other forming a vertical slit that only lets properly masticated food through and blocks bigger food particles. This reduces the chance of choking.
In addition to this, the laryngeal muscles contract which results in the closing of the glottis and the elevation of the larynx. Elevation of the larynx stretches opens the upper esophageal sphincter, allowing the bolus of the food to be transmitted from the pharynx into the esophagus. This is followed by a peristaltic wave starting due to the contraction of the superior constrictor muscles of the pharynx.
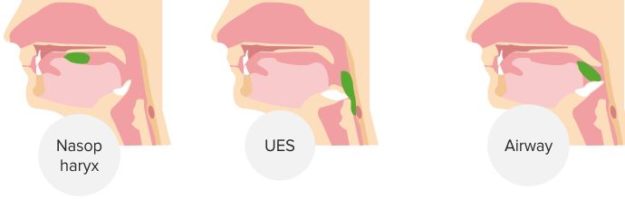
“Swallowing. Timing of Opening and Closing” Image created by Lecturio
Esophageal Motility
Esophageal motility is a completely involuntary act that starts with the entrance of the bolus of the food into the esophagus from the pharynx and ends with its exit into the stomach.There are three-factor aspects of this stage:
- Primary peristalsis: This is a continuation of the peristaltic wave that started in the pharynx due to the contraction of the superior constrictor muscles. The primary peristaltic wave propels the food downward.
- Secondary peristalsis: This is controlled by the myenteric plexus. Distension of the esophagus, caused by the bolus of the food, sets off a vagal reflex that causes the lower/gastroesophageal sphincter to relax (by releasing vasoactive intestinal peptide) in anticipation of the food bolus which is then pushed into the stomach.
- Gravity: When a person is standing, gravity assists in the downward movement of the food bolus in the esophagus.
Gastric Motility
In order to understand gastric motility, one needs to appreciate the physiological divisions of the stomach. They include two parts:- Orad region – made up of the fundus and the proximal part of the body. It functions to receive the ingested food from the esophagus.
- Caudad region – made up of the antrum and the distal half of the stomach. It functions to mix and churn food and then pushing it into the duodenum.
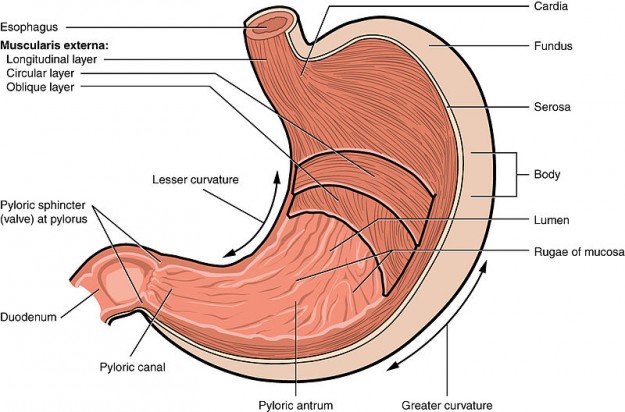
Bild: “Illustration from Anatomy & Physiology, Connexions Web Site” von OpenStax College. Lizenz: CC BY-SA 3.0
1. Receptive Relaxation
When the bolus of food enters and causes distention of the stomach, a vagovagal reflex is initiated that causes relaxation of the orad region of the stomach, hence accommodating the ingested food.
2. Mixing and Digestion
This occurs in the caudal region of the stomach and involves two types of waves:
Slow/weak peristaltic constrictor waves – these waves are regulated by basic electric rhythm and occur every 3–5 minutes. Their function is to mix the gastric secretions and the food together and weak propulsion.
Powerful peristaltic constrictor rings – this causes the contraction of the distal antrum, so when the weak peristalsis waves propel food towards the distal antrum, the power constrictor waves causes it to be propelled back (retropropulsion) therefore mixing the food in the process.
3. Gastric Emptying
Two factors controlling the emptying of the stomach contents into the duodenum are the pylorus (which is usually tonically contracted, therefore controls stomach emptying) and antral peristalsis or pyloric pump (the peristaltic movements that cause the propulsion of chyme into the duodenum).
“Functions of the various stomach areas. The orad is the top of the stomach and caudad is the bottom portion” Image created by Lecturio
Stomach contents: the types of food in the stomach can influence gastric emptying, for example, presence of fat in the stomach contents slows down gastric emptying because of the production of a hormone called Cholecystokinin. Cholecystokinin is produced by the I cells of duodenal and jejunal mucosa in response to the presence of fatty acids and monoglycerides, as well as amino acids. Its function is to inhibit and slow down gastric emptying so that more time can be spent digesting and absorbing food in the small intestines.
Similarly, fastest gastric emptying takes place when the gastric contents are isotonic in nature, whereas hypertonic (high osmolality) or hypotonic (low osmolality) stomach contents slows it down.
Other hormones that inhibit gastric emptying include secretin and gastric inhibitory peptide. The condition of the duodenum has a strong influence over stomach emptying as well. Its distention, irritation, acidity and presence of fat slow down gastric emptying. Increased volume of food stimulates the local and vagal myenteric reflexes that result in the increased activity of the pyloric pump and the relaxation of the pylorus.
Gastrin is another hormone that is released in response to the distention of the stomach walls due to increased food volume. It also increases the activity of the pyloric pump and relaxes the pylorus.
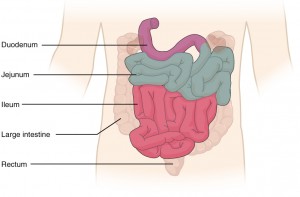
Intestinal Motility
Small intestines work to absorb many of the important nutrients needed by the body. Therefore, motility there consists of mixing contents with digestive enzymes and propelling them towards the large intestines. Slow waves are found in the intestinal motility, they cause the basic electric rhythm which is, at points, overridden by action potentials for stronger contractions. Slow waves are 12/mins.Parasympathetic stimulation increases contractions, whereas the sympathetic nervous system decreases them. There are two types of movements involved in small intestine motility.
Segmentations: When a portion of the small intestines receive chyme and gets distended, a localized response consisting of concentric contractions takes places. These are located at varying intervals throughout the small intestine, hence giving a “segmented” appearance. They work to mix the chyme so the nutrients can be absorbed better.
Peristalsis: They work to propel chyme forward.
Peristaltic rush is a phenomenon seen in the case of intestinal irritation (such as diarrhea) which consists of a very strong and rapid peristaltic wave that sweeps all intestinal contents and deposits them in the colon within one minute. It occurs so the small intestine mucosa can be relieved of the irritating contents.
Migrating motor complex is a peculiar pattern of activity experienced in an empty stomach and small intestines. It consists of slow and rhythmic peristaltic activity that sweeps down the stomach and small intestine every 1.5 – 2 hours to get excess content and secretions into the colon so they don’t build up.

“Gastric Motility” Image created by Lecturio
Review Questions
The correct answers can be found below the references.1. A 26-year-old medical student participates in a research about intestinal motility. On further investigation, which of the following part of his gastrointestinal tract will show “segmentation” as a part of motility?
- Stomach
- Esophagus
- Gall bladder
- Small intestines
- External Anal sphincter
- Cholecystokinin
- Histamine
- Bile
- Vasoactive intestinal peptide
- Somatostatin
Great post.
ResponderEliminarhttp://medicalassistance.mystrikingly.com/