Spinal Cord: Spinal Nerves, Cervical Plexus, Brachial Plexus & Gray and White Matter
In Lecturio - While the brain and the spinal cord make up the Central Nervous System (CNS), the Peripheral Nervous System (PNS) is comprised mainly of nerve fibers and ganglion cells. The two systems cannot be clearly distinguished from one another as they are functionally closely interlinked. The PNS conducts information from the CNS, via numerous nerve fibers, to the effector organs and vice versa. The cranial and spinal nerves belong to the PNS. In this article, we address the spinal nerves and the nerve plexuses that supply the extremities, namely the cervical and brachial plexus.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your anatomy course now for free!
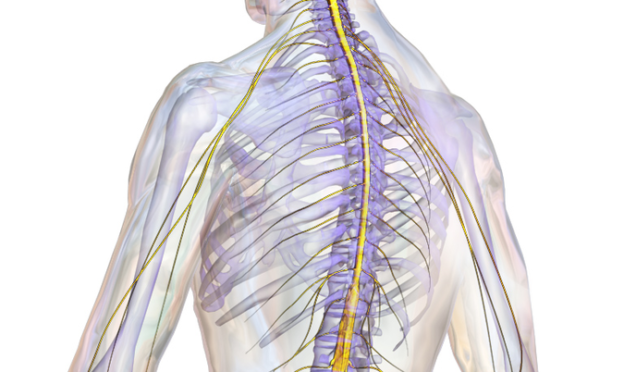
Spinal Nerves
Organisation and Structure of the Spinal Nerves

Image: “Neuraltherapie lumbaler Spinalnerv” by Stefan Methdorf. License: CC BY-SA 3.0
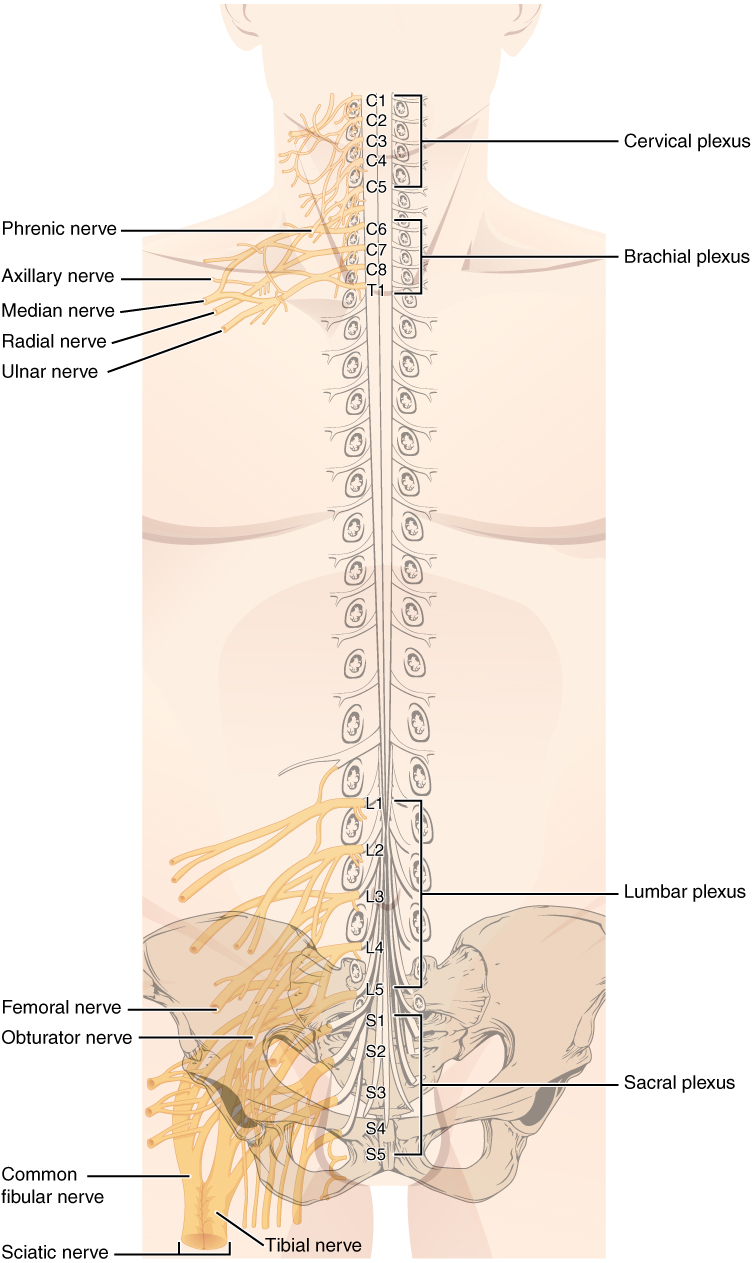
- Neck: 8 cervical nerve pairs (C1 – C8)
- Thorax: 12 thoracic nerve pairs (Th1 – Th12)
- Loins: 5 lumbar nerve pairs (L1 – L5)
- Sacrum: 5 sacral nerve pairs (S1 – S5)
- Coccyx: 1 – 2 coccygeal nerve pairs
Exception: As there are only 7 cervical vertebrae, the nerve pairs exit cranially from the vertebrae.
Shortly after passing through the intervertebral foramen, the spinal nerve gives off a thin meningeal branch (ramus meningeus) which runs back into the spinal canal and provides sensory innervation to the spinal meninges. Next, the spinal nerve divides into an anterior ramus and a posterior ramus.
While the posterior ramus divides into a medial branch and a lateral branch, which supply the skin of the back and the autochthonous back muscles, the anterior ramus innervates the ventrolateral body wall structures and the limbs and contributes to the formation of plexuses.
Furthermore, there is a connection to the sympathetic trunk via the two rami communicantes: the white ramus communicans appears white because of the myelinated fibers that lead to the sympathetic trunk, while the gray ramus communicans carries unmyelinated fibers from the sympathetic trunk to the spinal nerve, which cause the gray colouring.
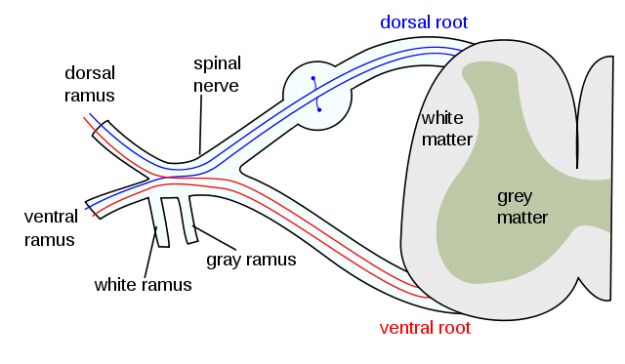
Image: “The formation of the spinal nerve from the dorsal and ventral roots” by Mysid. License: CC BY-SA 3.0
Segmental Innervation vs. Peripheral Innervation
Each spinal cord segment supplies, with its spinal nerves, a certain part of the body (= segmental or radicular innervation). In the thoracic wall, for example, it is intercostal nerves that provide the motor and sensory innervation.
On the sensory level, the segmental innervation creates so-called dermatomes: areas of the skin which can be assigned to the respective spinal cord segments. Only the C1 segment does not possess a dermatome since it consists of only motor fibers. In the thoracic area, the dermatomes lie in regular strips one above the other.
Note: Th10 approximately corresponds to the height of the navel; the boundary between Th4 and Th5 corresponds to the mamilla.
In the cervical, lumbar, and sacral regions, however, the anterior rami exchange fibers and intermix, thus forming the following nerve plexuses:
- Cervical plexus
- Brachial plexus
- Lumbar plexus
- Sacral plexus
Peripheral nerves emerge from the plexuses which each run to a supply area. Their last branches consist mostly of sensory skin nerves (= peripheral innervation). The nerve fibers again end in a segmental arrangement, so that the limb skin can also be divided into dermatomes.
Note: Segmental and peripheral innervations are not identical!

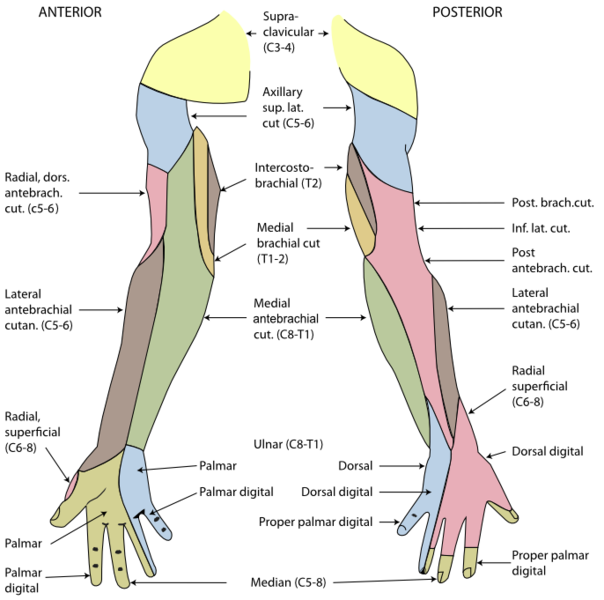
Image: “Dermatomes and major cutaneous nerves in an anterior and posterior view.” von Mikael Häggström.
This is, for example, why shingles (herpes zoster) causes painful skin blistering in the corresponding dermatomes because the pathogenic virus (varicella) attacks dorsal root ganglions.

Image: “Herpes zoster” by Fisle. License: CC BY-SA 3.0
Autonomous Zones and Segment-Indicating Muscles of Peripheral Nerves
The innervation areas of neighbouring peripheral nerves overlap at the edges, leading to a double innervation. There are skin areas, however, which are innervated by one peripheral nerve alone. These are known as autonomous zones.| Examples of Autonomous Zones | Nerve |
| Small finger | Ulnar nerve |
| First interdigital space | Deep peroneal nerve |
| Foot sole/heel | Tibial nerve |
| Segment-Indicating Muscle | Segment |
| Deltoid muscle | C5 |
| Biceps brachii muscle | (C5 –) C6 |
| Triceps brachii muscle | C7 |
| Interosseous muscles | C8 |
| Quadriceps femoris muscle | (L3 –) L4 |
| Tibialis muscle | L4 |
| Extensor hallucis longus muscle | L5 |
| Triceps surae muscle | S1 (– S2) |
Cervical Plexus
The interjoining of nerves in the neck (cervical plexus) is formed by the anterior rami of the spinal nerves of segments C1 – C4 and is located on the side of the transverse processes of the cervical spine between the prevertebral muscles (scalenus, levator scapulae) and below the sternocleidomastoid muscle.Sensory Nerves of the Cervical Plexus
At the posterior edge of the sternocleidomastoid muscle, the sensory branches of the cervical plexus emerge from the middle third and come up to the surface (= nerve point of the neck or Erb’s point) and innervate the head and neck region. The nerves are also known as cutaneous nerves and include:- Lesser occipital nerve (C2, C3): lateral, lower part of the back of the head (occiput) i.e posterosuperior to the auricle.
- Great auricular nerve (C2, C3): bottom of the ear and back of the pinna (auricle)
- Transverse cervical nerve (C2, C3): lateral and ventral neck; anastomosis with the cervical branch of the facial nerve, thereby forming the ansa cervicalis
- Supraclavicular nerves (C3, C4): shoulder and upper chest area
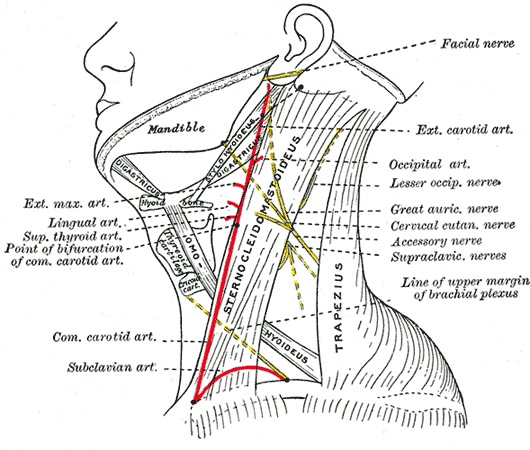
Nerves of Plexus Cervicalis – License: Public Domain
Note: Due to the joint outlet of sensory nerves at Erb’s point, the anaesthesia of the entire skin surface of the neck and nape of the corresponding side can be administered here.
Motor Nerves of the Cervical Plexus
They are nerves that supply various muscles. They include :- The ansa cervicalis that gives motor innervation branches of the infrahyoid muscles. It lies between the levator scapulae muscle and the scalene muscles. The ansa cervicalis arises from C1-C3 and results from the anastomosis of a superior root (C1, C2) with an inferior root (C2, C3). The superior root is temporarily attached to the hypoglossal nerve (cranial nerve (CN) XII).The geniohyoid and thyrohyoid are supplied by the C1 part while the rest give supply to the sternothyroid and omohyoid muscles.
- The cervical plexus also gives off smaller branches which are attached to the accessory nerve (CN XI) and supply the trapezius muscle and the sternocleidomastoid muscle.
- Segmental branches also innervate the anterior and middle scalene muscles.
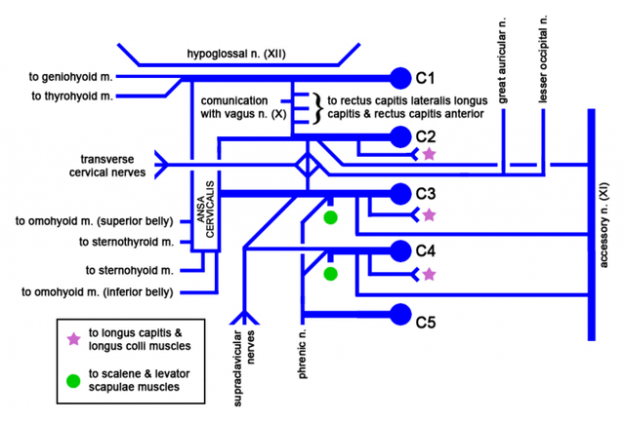
“Cervical plexus” by Mikael Häggström. License: Public Domain
Phrenic Nerve
The phrenic nerve emerges from the C3, C4 and C5 cervical nerve pairs. It extends along the anterior scalene muscle between the subclavian artery and vein into the mediastinum, where it runs between the pleura and the pericardium. It is the only nerve that provides motor innervation to the diaphragm and is therefore essential for breathing.
A unilateral phrenic nerve palsy can lead to an elevated hemidiaphragm on the affected side. The phrenic nerve also provides sensory innervation to the diaphragm, the pleura, the pericardium and the peritoneum.
Note: Three, Four, Five, keep the diaphragm alive!
Brachial Plexus
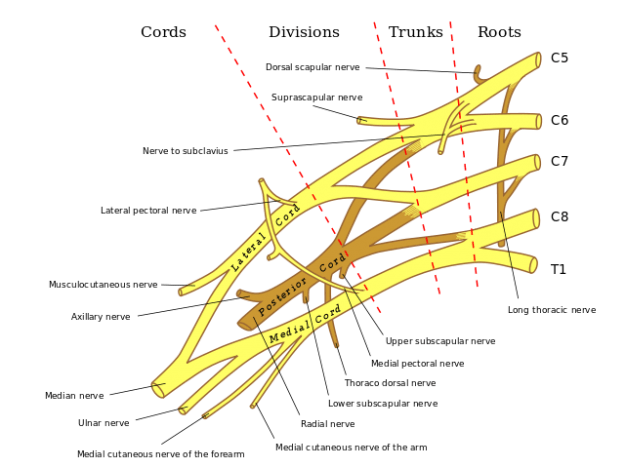
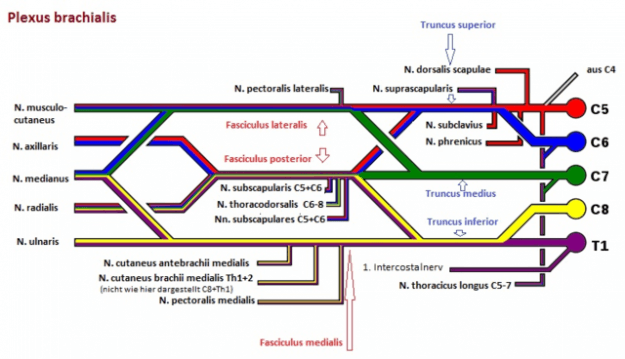
“Anterior view of right brachial plexus” by Mattopaedia. License: Public Domain
Formation of Trunks and Cords of the Brachial Plexus
The spinal nerves of segments C5 – Th1 and, in parts, also of segments C4 and Th2 are involved in the formation of the brachial plexus. They pass through a gap between the scalenus anterior and the scalenus medius muscle (= scalenus gap) in a distal direction. They form the supraclavicular part of the plexus by joining together above the clavicle as three primary strands that run alongside the subclavian artery in caudolateral direction:
- Upper trunk: C5 and C6
- Middle trunk: C7
- Lower trunk: C8 and Th1
Dorsal of the clavicle, they divide into three anterior strands (anterior divisions) and three posterior strands (posterior divisions). After entering the armpit (axilla) below the clavicle, the primary strands join again as secondary strands, the cords (fasciculi), and form the infraclavicular part of the plexus:
- Lateral cord: Upper trunk and middle trunk (C5 – C7)
- Posterior cord: Upper, middle and lower trunk (C5 – Th1)
- Medial cord: Lower trunk (C8 – Th1)
“Plexus brachialis: Schematische Darstellung” by Marshall Strother. License: Public Domain
Supraclavicular Part of the Brachial Plexus
From the supraclavicular part of the brachial plexus, the nerves exit either via the trunks or directly from the spinal nerves to innervate the shoulder girdle muscles:- Dorsal scapular nerve (C4 – C5): levator scapulae muscle, rhomboid major and minor muscle
- Suprascapular nerve (C4 – C6): subclavius muscle
- Long thoracic nerve (C5 – C7): serratus anterior muscle
- Subclavian nerve (C – C6): supraspinatus muscle and infraspinatus muscle
Infraclavicular Part of the Brachial Plexus
The infraclavicular part consists of short nerve branches, which run at level with the fasciculi towards the shoulder, and of long nerves, which represent the terminal branches of the secondary strands and run to the arm. The following three motor and two sensory nerves belong to the short branches:- Thoracodorsal nerve (C6 – C8): latissimus dorsi muscle
- Subscapular nerves (C5 – C6): subscapular muscle, teres major muscle
- Medial pectoral nerve (C8 – Th1) and lateral pectoral nerve (C5 – C7): pectoralis major and minor muscles
- Medial cutaneous nerve of the arm (Th1): upper arm skin
- Medial cutaneous nerve of the forearm (C8 – Th1): forearm skin
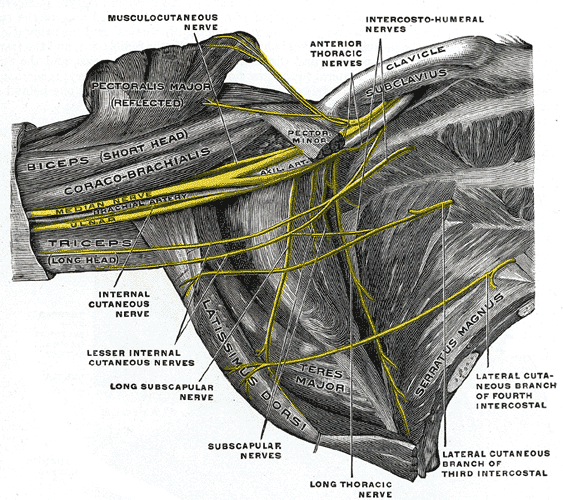
“The right brachial plexus in the axillary fossa” by Henry Gray. License: Public Domain
Musculocutaneous Nerve (C5 – C7)

Image: “Depicts the path of the musculocutaneous nerve in a cadaver.” by Frank Scali. License: CC BY-SA 3.0
The musculocutaneous nerve branches off from the lateral cord, pierces the coracobrachialis muscle, and runs between the brachial muscle and biceps brachii muscle to the forearm, where it ends as the lateral cutaneous nerve of the forearm which supplies sensory innervation to the lateral side of the forearm. The three flexor muscles it passes by receive motor innervation from it.
Axillary Nerve (C5 – C6)
The axillary nerve exits the posterior cord dorsally and runs with the posterior humeral circumflex artery through the lateral axillary space to the rear of the humerus. There, it runs along the surgical neck. It provides motor innervation to the deltoid muscle and the teres minor muscle. It ends in the superior lateral cutaneous nerve—a sensory nerve that innervates the skin on top of the deltoid muscle.
Note: Humeral fractures frequently occur at the surgical neck, which is why the axillary nerve is particularly vulnerable due to its proximity to this breaking point.
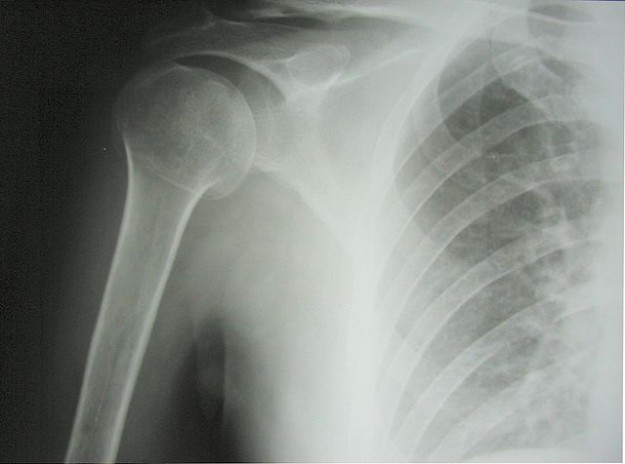
Image: “Surgical neck fracture of humerus” by Jojo. License: CC BY-SA 3.0

“The suprascapular, axillary, and radial nerves” by Henry Gray. License: Public Domain
The radial nerve runs as a continuation of the posterior cord in a distal direction. Already in the proximal upper arm area, it gives off sensory branches (posterior cutaneous nerve of arm and inferior lateral cutaneous nerve of arm) that supply the skin and a motor branch for innervation of the triceps muscle.
The radial nerve courses through the groove for the radial nerve (also called a spiral groove) in a spiralling fashion alongside the deep artery of the arm passing behind the humerus; it then pierces through the lateral intermuscular septum and finally, it runs between the brachial muscle and the brachioradialis muscle, which receive motor innervation from it, towards the elbow.
Here, it divides into two branches: the purely sensory superficial branch runs together with the radial artery along the brachioradialis muscle and towards the back of the hand, which it supplies, as well as the radial 2 ½ fingers.
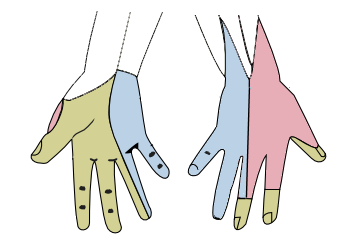
The cutaneous innervation of the right hand by Henry Gray. License: Public Domain
The deep branch supplies and pierces the supinator muscle, and ends as the posterior interosseous nerve of the forearm at the wrist, and innervates all of the extensors of the forearm and hand (see table).
| Location/Nerve | Sensory Innervation | Motor Innervation |
| Before radial tunnel | Lateral upper arm, lower half | Triceps brachii muscle |
| Within radial tunnel | Dorsal side of the upper arm and forearm | – |
| After radial tunnel | – | Brachoradial muscle; extensor carpi radialis longus muscle; extensor carpi radialis brevis muscle |
| Deep branch | – | Supinator muscle; extensor digitorum muscle; extensor digiti minimi muscle; extensor carpi ulnaris muscle; extensor pollicis longus muscle; extensor pollicis brevis muscle; extensor indicis muscle; abductor pollicis longus muscle |
| Superficial branch | Dorsal palm (lateral ¾) Radial 2 ½ fingers | – |
Note: In case of a fracture in the area of the humeral shaft, a lesion of the radial nerve may occur leading to a wrist drop (radial neuropathy). Because the extensors are not functioning properly, the hand and finger joints can no longer be stretched.
Median Nerve (C6 – Th1)
A branch of the medial cord—the medial root—unites with a branch of the lateral cord—the lateral root—before the axillary artery, to form the median nerve. It primarily innervates the flexor muscles of the forearm, as well as the pronators (see table).
Nerves of the left upper extremity by Henry Gray. License: Public Domain
There, it passes through the carpal tunnel—which is formed by the flexor retinaculum of the hand (ligamentum carpi transversum)—and divides on the palm into terminal branches to provide motor innervation to the thenar muscles and sensory innervation to the inner side of the radial 3½ fingers (common and proper palmar digital nerves).
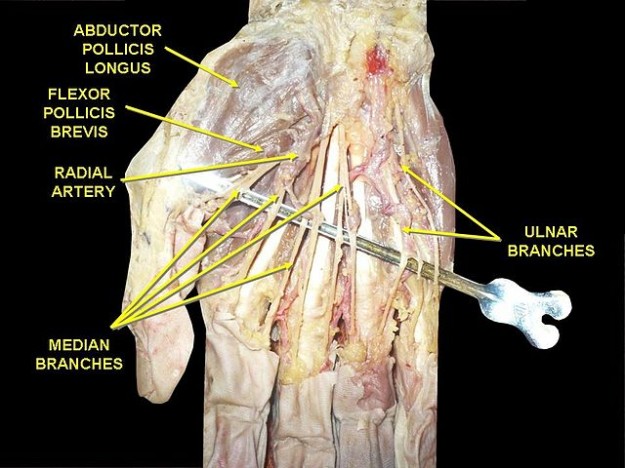
Image: “Branches of median nerve” by Anatomist90. License: CC BY-SA 3.0
| Location/Nerve | Sensory Innervation | Motor Innervation |
| Forearm, before passing the carpal tunnel | Thenar eminence (palmar branches of the median nerve); palm (radial 2/3) | Flexor carpi radialis muscle; palmaris longus muscle; flexor digitorum superficialis muscle; flexor digitorum profundus muscle (radial part); flexor pollicis longus muscle ;pronator teres muscle; pronator quadratus muscle |
| Hand, after passing the carpal tunnel | Radial 3½ fingers (palmar); parts of fingers 2 – 4 (dorsal); autonomous zone: distal fingers 2 and 3 | Abductor pollicis brevis muscle; flexor pollicis brevis muscle; opponens pollicis muscle; lumbrical muscles I and II |
Note: A lesion of the median nerve proximal to its passage through the carpal tunnel, results in the characteristic appearance of the hand called simian hand or ape hand: the patient cannot bend the thumb, index or middle fingers. Flexion is still possible in the two ulnar fingers (innervation of flexor digitorum profundus by the median nerve and the ulnar nerve).
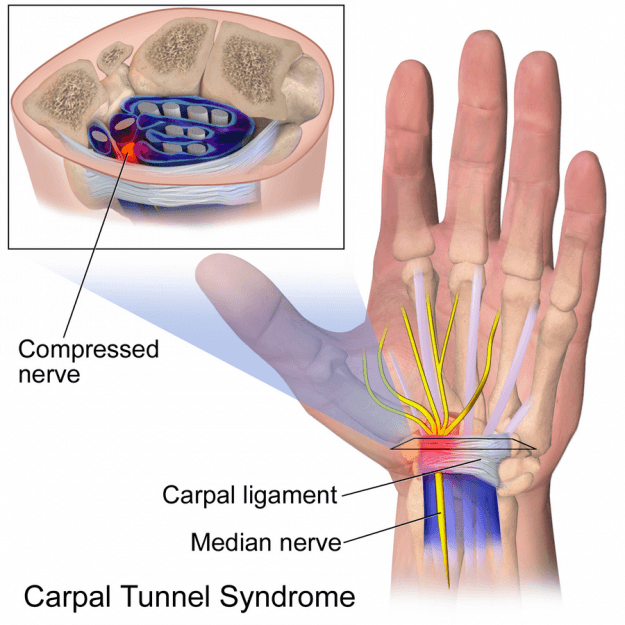
Median Nerve and Carpal Tunnel Syndrome
Median nerve supplies all the intrinsic muscles of the hand thus has a long course from the brachial plexus all the way through the flexor retinaculum where entrapment and a mononeuropathy ensues. The disorder is known as Carpal Tunnel Syndrome (CTS): however other syndromes have been reported such as the pronator teres syndrome or the anterior interosseous nerve syndrome.
It is characterized by paresthesias of the finger, typically nocturnal (brachialgia paraesthetica nocturna). When it progresses, symptoms may radiate to the entire hand and even arm, and occur also during the day. Further symptoms include painful sensitivity to pressure above the flexor retinaculum, sensory loss of the radial 3½ fingers and atrophy of the thenar muscles.
“Untreated Carpal Tunnel Syndrome” by Dr. Harry Gouvas. License: Public Domain.
A clinical sign is that patients can no longer hold a bottle since the abductor pollicis brevis muscle is weakened. Other indications include Tinel’s sign, in which a tap on the flexor retinaculum triggers an electrifying pain in the hand, and the Phalen sign, in which the hand is held in volar flexion for 30 seconds which causes dysesthesia.
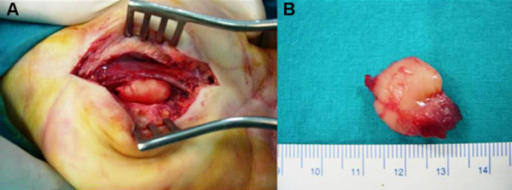
Carpal tunnel syndrome is initially treated with a forearm splint that is worn during the night and immobilises the wrist. For decompression of the nerve, the transverse carpal ligament is surgically split.
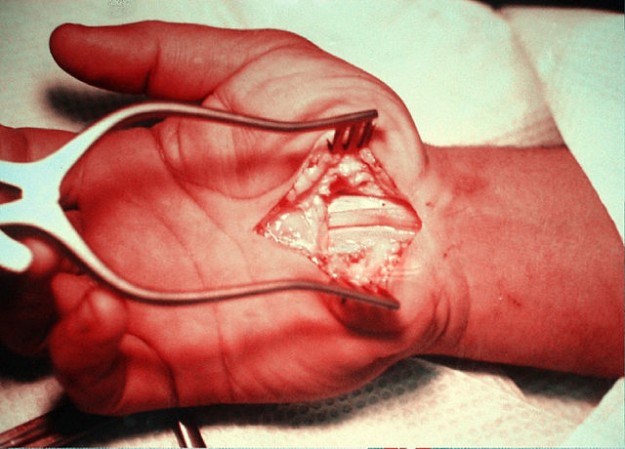
“Karpaltunnelsyndrom Operation” by Dr. Harry Gouvas. License: Public Domain
The ulnar nerve continues directly from the medial cord. It runs behind the brachial artery through the medial bicipital groove. Since it is relatively exposed in this area and lies directly on top of the bone, this part of the elbow is particularly sensitive to pain (“funny bone”). Still in the area of the upper arm, the ulnar nerve courses to the arm’s extensor side by piercing the medial intermuscular septum.
At the elbow, it runs underneath the medial epicondyle in the groove of the ulnar nerve. Together with the vasa ulnaria, the nerve passes between the two heads of the flexor carpi ulnaris muscle to the wrist. Here, it courses—contrary to the median nerve—above the flexor retinaculum in the Guyon’s canal to the inner side of the hand where it divides into its terminal branches: superficial and deep branch.
| Location/Nerve | Sensory Innervation | Motor Innervation |
Forearm
|
Ulnar side of the dorsal and palmar hand; fingers 4 and 5 (dorsal; dorsal branch)
|
Flexor carpi ulnaris muscle; flexor digitorum profundus muscle (ulnar part)
|
Hand: deep branch – motor; superficial branch – sensory
|
Fingers 4 and 5 (palmar); Autonomous zone: distal small finger
|
Palmaris brevis; abductor digiti minimi; flexor digiti minimi; opponens digiti minimi; lumbricals III and IV; palmar and dorsal interossei; adductor pollicis; flexor pollicis brevis
|
Note: Injury to the ulnar nerve, in its groove, leads to the symptom of claw hand: When active finger flexors are innervated by the median nerve, it causes the malfunction of lumbrical and interosseous muscles. Also, hypothenar and interosseous atrophy can be observed.
Hint: For remembering the characteristic effects that nerve injuries have on the hand, use the “Dr. Cuma” mnemonic: wrist Drop – Radial nerve, Claw hand – Ulnar nerve, Median nerve – Ape hand.
For an overview of sensory innervation of the upper limbs, see the following illustration:
Gray and White Matter
The formation of the spinal nerve from the dorsal and ventral roots
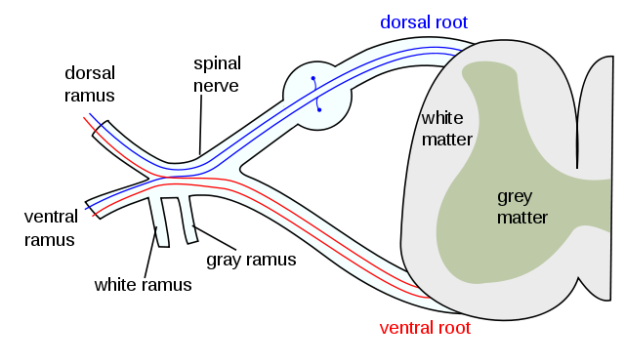
Image: “The formation of the spinal nerve from the dorsal and ventral roots.” by Mysid (original by Tristanb) – Vectorized in CorelDraw by Mysid on an existing image at en-wiki by Tristanb.
License: CC BY-SA 3.0
License: CC BY-SA 3.0
MRI: White matter structure
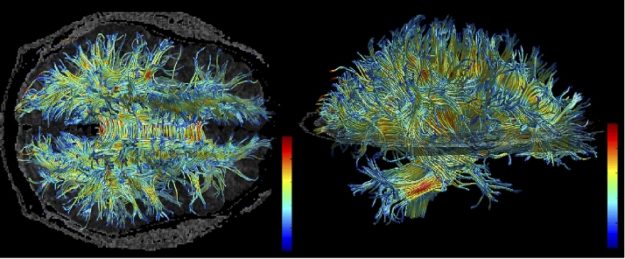
Image: “White matter structure of human brain (taken by MRI).
High resolution data acquired on 3 Tesla magnet and post-processed using automated tracking procedure. Voxels within fiber bundles are color coded according to their FA values (i.e., blue, low anisotropy; and red, high anisotropy).” by Kubicki M., McCarley R.W., Westin C-F., Park H-J., Maier S.E., Kikinis R., Jolesz F.A., Shenton M.E. A review of diffusion tensor imaging studies in schizophrenia. J Psychiatr Res. 2007 Jan-Feb;41(1-2):15-30. PMID: 16023676. PMCID: PMC2768134.
License: CC BY-SA 3.0
High resolution data acquired on 3 Tesla magnet and post-processed using automated tracking procedure. Voxels within fiber bundles are color coded according to their FA values (i.e., blue, low anisotropy; and red, high anisotropy).” by Kubicki M., McCarley R.W., Westin C-F., Park H-J., Maier S.E., Kikinis R., Jolesz F.A., Shenton M.E. A review of diffusion tensor imaging studies in schizophrenia. J Psychiatr Res. 2007 Jan-Feb;41(1-2):15-30. PMID: 16023676. PMCID: PMC2768134.
License: CC BY-SA 3.0
Comentários
Enviar um comentário