Polycystic Ovary Syndrome (PCOS, Polycystic Ovaries) — Causes and Treatment
In Lecturio - Polycystic ovary syndrome or disease is a multisystem endocrinological disorder where there is hyperandrogenism, ovarian dysfunction, obesity, menstrual abnormalities and multiple ovarian cysts. The most common presenting features are hirsutism, acne, metabolic syndrome and biochemical hyperandrogenism. Patients also have hyperlipidemia and an impaired glucose metabolism. Treatment involves oral contraceptive pills for menstrual abnormalities and hyperandrogenism, metformin for hyperandrogenism and infertility and clomiphene for infertility. Infertile women who do not respond to clomiphene might benefit from gonadotropins or laparoscopic ovarian drilling (LOD).
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your course “Reproductive System” now for free!
Definition of Polycystic Ovary Syndrome
Polycystic ovary syndrome is a heterogenous multisystem endocrinopathy that is characterized by hyperandrogenism, ovarian dysfunction and multiple cysts in the ovaries. The condition is also associated with metabolic syndrome, hyperinsulinemia and insulin resistance.Epidemiology of Polycystic Ovary Syndrome
Several diagnostic criteria exist for the diagnosis of polycystic ovary syndrome; some of them are stricter than the others and, accordingly, the prevalence of polycystic ovary syndrome is expected to differ according to which diagnostic criteria are used.Regardless of that, the prevalence of polycystic ovary syndrome is estimated to be 8% to 17% of women in their reproductive age and is fast increasing due to change in lifestyle and increasing stress. This figure makes polycystic ovary syndrome one of the most common endocrinological disorders in the population.
A family history of polycystic ovary syndrome, weight gain, sedentary lifestyle, and history of epilepsy disorder all increase the risk of developing polycystic ovary syndrome. A past medical history of valproate use increases the risk of polycystic ovary syndrome. Diabetes is also associated with an increased risk of polycystic ovary syndrome.
According to the NICHD Guidelines the patient must demonstrate both:
- Clinical and/or biochemical signs of hyperandrogenism
- Oligo- or chronic anovulation
Exclusion of other etiologies of androgen excess and anovulatory infertility is necessary.
Pathophysiology of Polycystic Ovary Syndrome
Patients with polycystic ovary syndrome are usually hyperinsulinemic and they have insulin resistance. It is believed that hyperinsulinemia results in a vicious cycle by facilitating weight gain, increasing free fatty acids in the blood, and worsening insulin resistance. This vicious cycle puts the patient at an increased risk of metabolic syndrome, a common encounter in patients with polycystic ovary syndrome.
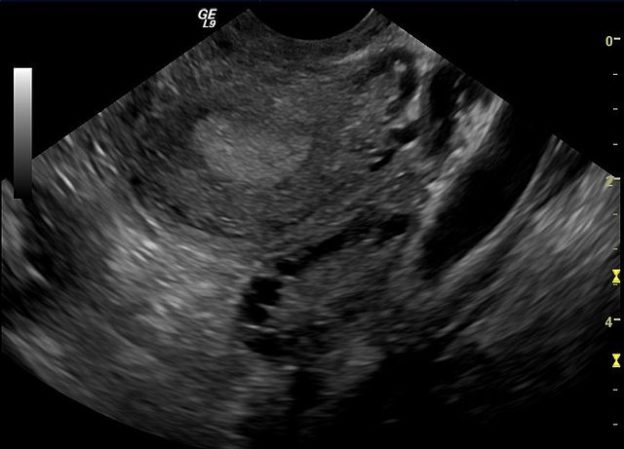
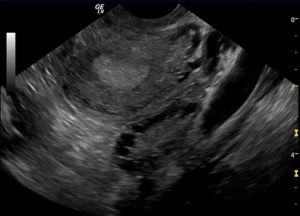
Image: “Ultrasound Image of Polycystic Ovary.” by Je Hyuk Lee – Own Work. License: CC BY-SA 3.0
Dyslipidemia occurs in patients with polycystic ovary syndrome due to insulin resistance and excessive hepatic production of triglycerides.
Hormonal changes in PCOS
Hormones Increased | Hormones Decreased |
|
|
Clinical Presentation of Polycystic Ovary Syndrome
Patients with polycystic ovary syndrome present with hyperandrogenism-related symptoms such as hirsutism, changes in the voice, infertility, and obesity. The menstrual cycle is either irregular or the patient can have amenorrhea. Among infertile women, about 20% are due to anovulation caused by PCOS.In addition to this picture, patients with polycystic ovary syndrome also show signs of insulin resistance which are weight gain, glucose intolerance, hyperlipidemia, increased blood pressure and acanthosis nigricans.
Evaluation of Women with PCOS
| Gynecological history | Family history | Medication |
|
| 
“Medication” created by Lecturio
|
Diagnostic Work-up for Polycystic Ovary Syndrome
A large part of the diagnostic work-up is aimed at excluding other causes of hyperandrogenism. Adrenal and ovarian tumors, hyper- or hypothyroidism, acromegaly and Cushing syndrome should be excluded.Late-onset congenital adrenal hyperplasia can have a similar presentation to polycystic ovary syndrome and should be excluded. Serum 17-hydroxyprogesterone levels are elevated after cosyntropin challenge in patients with this disease, but not in polycystic ovary syndrome.
24-hour urine collection for cortisol can be used to exclude Cushing syndrome. Patients with no signs of acromegaly do not need further work-up to exclude the diagnosis. If the patient has a picture that is similar to acromegaly, serum insulin-like growth factor 1 can be checked which is not elevated in polycystic ovary syndrome.
Once the exclusion of the other diseases known to cause hyperandrogenism is finished, the first criterion for the diagnosis of polycystic ovary syndrome is met.
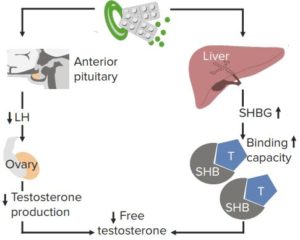
The next step is to confirm hyperandrogenism biochemically. Free to total testosterone is very specific and is usually elevated in patients with polycystic ovary syndrome. Additionally, patients with polycystic ovary syndrome have a low level of sex hormone-binding globulin. Dehydroepiandrosterone sulfate is elevated in hyperandrogenism from adrenal origin but not in polycystic ovary syndrome.
As we explained in the pathophysiology section, hyperinsulinemia alone is unlikely to cause hyperandrogenism in these patients. Luteinizing hormone (LH) is also elevated in polycystic ovary syndrome, but follicle-stimulating hormone (FSH) is normal. This gives an LH/FSH ratio that is usually above 3 in polycystic ovary syndrome.
A glucose tolerance test is indicated in the evaluation of these patients to exclude glucose intolerance, a common complication of the disorder. Additionally, women with polycystic ovary syndrome who become pregnant are at risk of developing gestational diabetes and they should be closely monitored. Dyslipidemia can complicate the picture and the patient might have a total cholesterol level that is above 200 mg/dl or an LDL-cholesterol level above 160 mg/dl.
After the exclusion of the other causes of hyperandrogenism and the confirmation of biochemical and clinical hyperandrogenism, ovarian dysfunction has to be confirmed as well. Ovarian dysfunction in polycystic ovary syndrome can be identified from the clinical history, amenorrhea or irregular menstrual cycle, or from the abnormal LH/FSH ratio. The final criterion in the diagnosis of polycystic ovary syndrome is to visualize polycystic ovaries on imaging or laparoscopy.
Transvaginal ultrasonography is preferred for the visualization of the pelvic organs including the ovaries. This helps confirm the diagnosis by visualizing multiple ovarian cysts and also excluding other causes of menstrual dysfunction, such as endometriosis or anatomical uterine abnormalities.
If the risk of ovarian malignant cyst is high, abdominal CT scan or MRI is indicated to further study the cyst and exclude tumor extension.
If more than 12 cysts can be identified in one ovary, the diagnosis of polycystic ovaries is made. This is different from polycystic ovary syndrome in which the number of the ovarian cysts need not to be 12.
Treatment of Polycystic Ovary Syndrome
Treatment of polycystic ovary syndrome includes treatment that is against the hyperandrogenism state, treatment of menstrual abnormalities, and treatment of infertility when pregnancy is wanted. Another symptomatic treatment of hyperinsulinemia and metabolic syndrome is also indicated.Premenopausal women with polycystic ovary syndrome, who present with hirsutism, benefit from oral contraceptive pills. Additionally, laser and mechanical hair removal is usually required for better results. After six months, if the patient still complains from hirsutism, then antiandrogens can be used.
“Medical Management of PCOS” Image created by Lecturio
As we have explained, hyperinsulinemia plays a role in the hyperandrogenic state in polycystic ovary syndrome by a co-androgenic effect with the luteinizing hormone. Accordingly, metformin and thiazolidinediones have been used with success in the treatment of hirsutism and hyperandrogenism in this condition. These drugs work by increasing insulin sensitivity and they are also expected to help the patient lose weight, improve their lipid profile, and improve glucose intolerance.
Patients with polycystic ovary syndrome also have menstrual abnormalities that need to be fixed. Combined oral contraceptive pills help by fixing the cycle irregularity. Additionally, weight loss improves the semiology of these patients by decreasing insulin resistance and can also help with the menstrual abnormalities.
Polycystic ovary syndrome can be identified as the etiology of infertility in some women and these women need treatment to help with getting pregnant. The first-line therapy to improve fertility in polycystic ovary syndrome is to lose weight.
Clomiphene citrate is used in women with polycystic ovary syndrome who are infertile. Clomiphene is an antiestrogenic that acts on the hypothalamus and leads to an increase in the pulse frequency of gonadotropin releasing hormone (GnRH) which manifests as an elevation in FSH concentration. This fixes the LH/FSH ratio which is known to be impaired in polycystic ovary syndrome, which results in more ovulatory cycles and the probability of having an ovulatory cycle is estimated to be about 85% after starting treatment.
As the main cause of infertility in polycystic ovary syndrome is related to anovulation, restoring ovulation can achieve pregnancy in up to 60% of the women in the first six months of treatment.
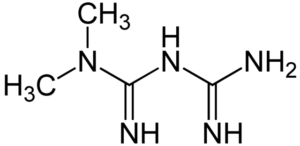
Image: “Chemical Formula of Metformin” by Jü – Own Work. License: Public Domain
Women who do not achieve ovulation by medical treatment are candidates for laparoscopic ovarian drilling (LOD) or gonadotropins. FSH administration, a gonadotropin, can achieve pregnancy but has several side effects, such as ovarian hyperstimulation syndrome. LOD is recommended when the patient does not want gonadotropin therapy, or when surgery is indicated for other reasons.
Surgery is reserved for cases in whom :
- Medical therapy fails
- Hyperstimulation occurs
- Infertile Women
- Previous Pregnancy loss
Women who do not achieve pregnancy with the above methods are candidates for in-vitro fertilization. Fortunately, the risk of miscarriage or other complications in women with polycystic ovary syndrome who undergo in-vitro fertilization is similar to the general population of in-vitro fertilization patients.
Complications of PCOS
If women conceive having PCOS, condition like carbohydrate intolerance, diabetes and hypertension may develop during pregnancy and pregnancy loss is as high as 20%. Other common complications for PCOS are- Increased risk of CVS disorders
- Increased risk of diabetes
- Increased risk of endometrial and breast carcinoma
- Hirsutism
- Increased risk of mood disorders
Comentários
Enviar um comentário