Stable and Unstable Angina Pectoris — Symptoms and Diagnosis
In Lecturio - The main symptom of coronary heart disease is angina pectoris, which can be divided into a stable and an unstable form.
Table of Contents
- Definition of Stable Angina Pectoris
- History of Stable Angina Pectoris
- Examination of Stable Angina Pectoris
- Investigations of Stable Angina Pectoris
- Treatment of Stable Angina Pectoris
- Definition of Unstable Angina Pectoris
- Diagnosis of Unstable Angina Pectoris
- Treatment of Unstable Angina Pectoris
- References
Are you more of a visual learner? Check out our online video lectures and start your pathology course now for free!
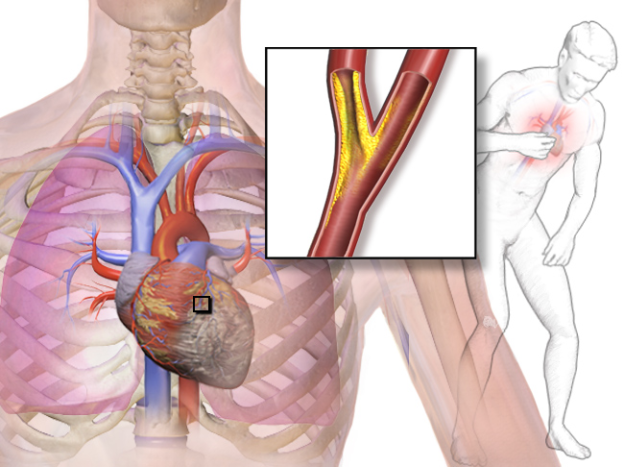
Image: “Angina” by Bruce Blaus, Blausen.com staff. “Blausen gallery 2014”. Wikiversity Journal of Medicine. DOI:10.15347/wjm/2014.010. ISSN 20018762. – Own work, License: CC BY 3.0
Definition of Stable Angina Pectoris
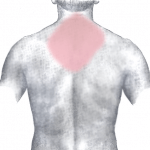
Image: “Pain in acute myocardial infarction (rear)” by J. Heuser. License: CC BY-SA 3.0
Stable angina is responsive to treatment with nitrates within minutes, and is always of the same pain intensity and quality.
It’s an episodic chest pain due to transient myocardial ischemia. The characteristic chest pain occurs with exertion or exercise (also termed: exertional angina) in a patient with narrow coronary arteries due to fixed atheromatous stenosis.
History of Stable Angina Pectoris
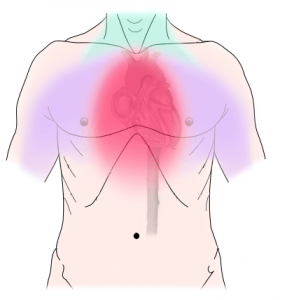
Image: “Diagram of discomfort caused by coronary artery disease. Pressure, fullness, squeezing or pain in the center of the chest. Can also feel discomfort in the neck, jaw, shoulder, back or arm.” By lan Furst. License: CC BY-SA 3.0
Onset, course and duration
The pain starts gradually, with the intensity increasing and decreasing (crescendo-decrescendo in nature) within minutes, typically lasts 2–5 minutes. It generally does not last for 20 to 30 minutes, unless the patient has acute coronary syndrome.
Site of pain
coronary pain is usually described as central substernal discomfort in which patient can’t localize the site of pain, and typically places his hand or clenched fist over the sternum.Radiation
The pain radiates to any dermatome from C8 to T4, most often to the left shoulder and left arm (especially the ulnar surface). Also it can radiate to interscapular region, back, epigastrium and lower jaw.Precipitating and relieving factors
Episodes of angina is provoked by physical exertion and intense emotion, and relieved within minutes by rest and sublingual nitroglycerin.Associated symptoms
Angina is usually associated with shortness of breath, diaphoresis, dizziness, lightheadedness, and fatigue.Examination of Stable Angina Pectoris
Physical examination is usually unremarkable in patients with stable angina when they are asymptomatic, but clinicians should search for:- Important risk factors: hypertension and diabetes mellitus
- Evidence of atherosclerosis at other sites, as carotid bruits and peripheral vascular disease
- Evidence of valvular diseases and left ventricular dysfunction
Investigations of Stable Angina Pectoris
Resting ECG
It is normal between attacks, and may show evidence of previous myocardial infarction. During the pain, reversible ST segment depression or elevation, with or without T-wave inversion, is suggestive of myocardial ischemia.Exercise ECG
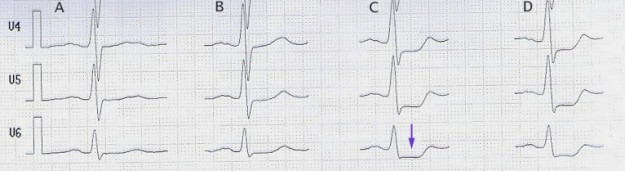
Image: “stress-ecg with st-segment-depression (arrow) beginning at 100 W (column C)” by J. Heuser. License: CC BY-SA 3.0
Isotope scanning
Thallium scan can show areas of diminished uptake of radioactive isotope by coronary myocardium at rest or during exercise.Angiography
It visualizes the location, number and severity of coronary artery stenosis, and indicated in whom coronary revascularization is being considered.Treatment of Stable Angina Pectoris
General measures
- Life style modification and control the previously mentioned risk factors
- Assessment of the extent and severity of atherosclerosis affecting different body organs
Medical treatment
1. Antiplatelet therapy: Low-dose aspirin or Clopidgorel (if aspirin intolerant) should be prescribed for all patients.2. Antianginal therapy:
- Nitrates:
- Causes venous and arterial dilatation, thus lowering myocardial oxygen demand by reducing the preload and after load on the heart
- Sublingual glyceryl trinitrate (GTN) should be taken during attack, relieves the pain within 2–3 minutes
- Taken prophylactically before strenuous exercise
- Beta-Blockers:
- Lower myocardial oxygen demand by reducing heart rate and force of contraction
- Aim of therapy: relieve angina and ischemia, and reduce mortality and re-infarction rates after myocardial infarction
- Calcium channel antagonists:
- Lower myocardial oxygen demand by reducing blood pressure and myocardial contractility
Coronary revascularization
It’s more appropriate to start treatment of stable angina initially with the medical treatment. Coronary revascularization should be considered in:- Low exercise capacity or ischemia at low workload
- Large area of coronary myocardium
- Impaired LV function with ejection fraction < 40 %
Definition of Unstable Angina Pectoris
The unstable angina refers to complaints that persist longer than 20 minutes, are of increasing intensity and occur even at rest. Together with the myocardial infarction, unstable angina pectoris is referred to as an acute coronary syndrome.Unstable angina (UA) is characterized by absence of myocardial damage, in contrast to the non-ST-elevation MI (NSTEMI) which presents with evidence of myocardial necrosis.
Diagnosis of Unstable Angina Pectoris
The diagnosis of UA/NSTEMI depends mainly on the history, abnormalities on ECG and the cardiac biomarkers.History
Chest pain is similar in character to stable angina pectoris, but it is characterized by at least one of the following three features:- It’s severe and of new onset.
- It occurs on minimal exertion or even at rest, and lasts longer.
- It’ characterized by being more intense and rapidly worsening (crescendo angina), not fully relieved by rest or nitroglycerin.
Abnormalities on ECG
- Transient or persistent ST-segment depression and/or T-wave inversion in 30–50 % of patients.
- ST segment elevations and Q waves are absent in both UA and NSTEMI
- ECG can be normal
Cardiac biomarkers
Cardiac enzymes are used to differentiate between Unstable Angina (UA) and non-ST-elevation MI (NSTEMI) :- Unstable angina → No myocardial damage → thus, normal cardiac enzymes
- Non-ST-elevation MI (NSTEMI) → evidence of myocardial damage → elevated cardiac enzymes such as CK-MB and troponin I and T (more specific & sensitive marker)
Treatment of Unstable Angina Pectoris
Since initial ECG is not diagnostic, patients with UA/NSTEMI should rest on bed with serial ECG monitoring for any ST-segment deviation until pain resolves on definitive diagnosis is made.Medical treatment
It involves simultaneous administration of anti-coronary and anti-thrombotic treatment.1. Anti-coronary treatment:
- Nitrates:
- Sublingual Nitroglycerin , maybe repeated at 3-5 minutes if chest discomfort persists. If no response after 3 doses, consider IV nitroglycerin.
- Beta-Blockers:
- Metoprolol is given with a target heart rate: 50-60 beats/minute.
- If beta-blocker is contraindicated, consider calcium channels blockers (CCBs): verapamil or diltiazem.
- Aspirin:
- High dose (375 mg/day) then lower doses (75 mg/day) for long-term treatment
- Clopidogrel:
- As early as possible in addition to aspirin unless there’s risk of bleeding
- Pretreatment with clopidogrel is recommended prior to PCI
- Anti-coagulant:
- In addition to aspirin and clopidogrel, four anticoagulant options are available:
- Unfractionated heparin (UFH)
- Low-molecular-weight heparin (LMWH) “enoxaparin”: is superior on UFH with less risk of hemorrhage
- Fondaparinux: indirect Factor Xa inhibitor, and it is equal in efficacy with enoxaparin but lower risk of bleeding
- Bivalirudin: direct thrombin inhibitor, and it is equal in efficacy with UFH and LMWH
- In addition to aspirin and clopidogrel, four anticoagulant options are available:
Early invasive strategy
Only high risk patients can benefit from coronary revascularization (PCI or coronary artery bypass grafting):- Age > 65 years
- > 3 CAD risk factors
- ST deviation
- > 2 anginal events < 24h
- Elevated cardiac markers
Comentários
Enviar um comentário