Non-Invasive Breast Cancer: Ductal Carcinoma In Situ (DCIS) — Diagnosis and Treatment
In Lecturio - Non-invasive breast cancer can be either ductal carcinoma in situ or less commonly lobular carcinoma in situ. Ductal carcinoma in situ is of epithelial type, and there is usually no basement membrane invasiveness. Because of the lack of invasiveness, these tumors are unlikely to metastasize by the lymphatics or blood vessels. Ductal carcinoma in situ is usually diagnosed by a mammography and not by physical examination. Microcalcifications on mammography are the most common presenting feature. Local excision of the lesion is recommended to obtain histopathologic data and guide treatment. Total mastectomy or breast conservation therapy are the two options for the treatment of ductal carcinoma in situ.
Are you more of a visual learner? Check out our online video lectures and start your hematology course now for free!
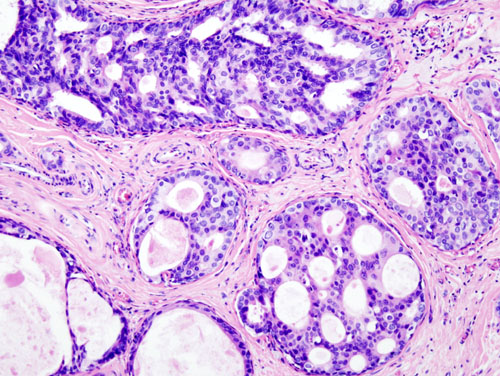
Image: “Histopathologic image from ductal cell carcinoma in situ (DCIS) of breast. Hematoxylin-eosin stain.” by No machine-readable author provided. KGH assumed (based on copyright claims). – No machine-readable source provided. Own work assumed (based on copyright claims). License: CC BY-SA 3.0
Definition of Non-Invasive Breast Cancer
A non-invasive carcinoma, also known as an in-situ carcinoma, is a term used to describe the malignant transformation of epithelial cells that remain in their original site without invading the basement membrane.Classification
Two types of non-invasive breast cancer exist, which are:- Ductal carcinoma in situ (DCIS)
- Lobular carcinoma in situ (LCIS)
| Type | Characteristic | Notes |
| Non-invasive | ||
| Ductal carcinoma in situ (DCIS) | Fills ductal lumen; arisis from ductal hyperplasia | Early malignancy without basement membrane |
| Comedocarcinoma | Ductal, caseous necrosis (A) Subtype of DCIS | Several adjacent ducts are filled by tumor associated with large central zones of necrosis and calcified debris. This type of DCIS most frequently is detected as radiological calcifications. |
Epidemiology of Non-Invasive Breast Cancer
It is the most common type of non-invasive breast cancer.About 60,000 cases of DCIS are diagnosed in the United States each year. The incidence of non-invasive breast cancer is expected to be under-reported due to the lack of any specific symptoms or signs. DCIS, the clinically relevant form of non-invasive breast cancer, can be identified in approximately 15 % of all cases of breast cancer. The introduction of routine mammography screening protocols made the early diagnosis of DCIS possible.The majority of the cases nowadays have a tumor that is less than 10 mm in diameter. Such a small size is unlikely to be detected by palpation, but can be easily identified with mammography.
Most patients with DCIS are aged 45 to 65 years. This is the same age group for invasive breast cancer, and these patients also share several similar risk factors to invasive breast cancer, such as family history of breast cancer, early menarche and late menopause.
Pathophysiology of Non-Invasive Breast Cancer
Ductal carcinoma in situ arises from the ductal epithelium. Due to poorly understood reasons, ductal epithelium can undergo hyperplasia. At a certain point, ductal hyperplasia starts showing dysplastic features and atypical ductal hyperplasia ensues.
Image: “Ductal carcinoma in situ.” by Don Bliss (Illustrator) – This image was released by the National Cancer Institute, an agency part of the National Institutes of Health, with the ID 4353. License: Public Domain
Ductal carcinoma in situ does not invade the basement membrane. Accordingly, DCIS does not have access to lymphatics and/or blood vessels and lymphatic spread or distant metastasis is not usually a problem with non-invasive breast cancer.
Clinical Presentation of Non-Invasive Breast Cancer
The introduction of routine mammography and clear screening guidelines for breast cancer made the diagnosis of non-invasive breast cancer easier and earlier. Accordingly, nowadays, most patients with ductal carcinoma in situ of the breast present to the clinic for their routine mammogram only to find a small, less than 10 mm tumor in the breast. Up to 80% of ductal carcinomas are diagnosed as a lump on mammography.Patients who do not undergo routine mammography, for some reason, might present with a palpable mass, nipple discharge or Paget’s disease of the nipple. These presentations are unlikely to happen when the tumor is less than 1 cm in diameter.
Diagnostic Work-up for Non-Invasive Breast Cancer
Physical examination
Annual breast examination has been recommended for screening of breast carcinoma and DCIS could be diagnosed early as a mass/lump. Masses that cannot be felt on physical examination are diagnosed via mammography.Mammography
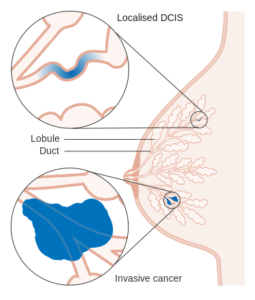
Image: “Diagram showing ductal carcinoma in situ (DCIS).” by Cancer Research UK – Original email from CRUK. License: CC BY-SA 4.0
High-grade DCIS, which also has comedo necrosis, presents with linear-branching microcalcifications. On the other hand, low-grade DCIS usually presents with fine granular microcalcifications.
Bilateral mammography is indicated.
Histologic examination
The tissue for histology could be obtained via:- FNAC (fine needle aspiration for cytology)
- Core needle biopsy that may be under mammography or ultrasound guidance
After the removal of the tumor, several features need to be noted to determine prognosis. The tumor size, if more than 1 cm, might predispose the patient to possible microinvasion.
Additionally, the nuclear grade and presence or absence of comedo-type necrosis is also important prognostic factors in DCIS.
Treatment of Non-Invasive Breast Cancer
Treatment of non-invasive breast cancer or DCIS involves total mastectomy, breast conservation therapy and/or breast irradiation.Total mastectomy, with or without axillary lymph node clearance, provides effective and curative treatment of DCIS, but can be easily judged as an over-treatment for a relatively non-invasive disease. Additionally, up to 15 % of patients with breast cancer are diagnosed in this early stage, and providing a total mastectomy to this large number of patients is indeed challenging.

Image: “Total (simple) mastectomy.” by National Cancer Institute – This image was released by the National Cancer Institute, an agency part of the National Institutes of Health, with the ID 7129. License: Public Domain
Because of these reasons, more research has been done to evaluate the role of either breast conservation therapy or local excision of the tumor alone as possible treatments for DCIS.
Breast conservation therapy includes local excision of the tumor plus radiotherapy.
Local excision should be mammographically guided and care should be taken to achieve a safe negative margin of the resection. A repeat mammogram after excision should be negative for microcalcifications before initiating radiotherapy.
Approximately four weeks after the local excision of the non-invasive breast cancer lesion, radiotherapy is usually started. Current approaches utilize whole breast irradiation therapy. Current protocols for adjuvant radiotherapy do not include lymph node irradiation.
Patients with very small tumors and without any occult invasive breast cancer can benefit from local excision alone without adjuvant radiotherapy.
Local recurrence after local excision alone is estimated to be about 33 % for patients with high-grade DCIS and 2 % for low-grade DCIS. This interesting finding can help the patient choose a more appropriate approach, such as conservative breast therapy instead of local excision alone when they have high-grade DCIS.
Patients with high-grade DCIS, or a tumor that is large in size with evidence for occult invasive breast cancer disease, might not be possible candidates for breast conservation therapy due to other comorbidities and contraindications to radiotherapy, such as pregnancy, collagen vascular diseases, or a previous history of chest irradiation therapy. In this case, total mastectomy remains the most effective method to prevent local recurrence.
Low to intermediate grade DCIS was found to express estrogen and progesterone receptors. Accordingly, tamoxifen was used for primary and secondary prevention of DCIS. It was found that primary prevention of breast cancer is possible with the use of tamoxifen, but there is still debate on who should receive tamoxifen for primary prevention of breast cancer.
Tamoxifen was used for secondary prevention of breast cancer in the contralateral breast with very good results and is currently recommended. Currently, tamoxifen is used for secondary prevention of DCIS only in clinical trials.
I was diagnosed with stage 3 breast cancer in August of 2010. A precious friend told me about Dr Itua Herbal Center in West Africa,She gave me his contact number and email address,I contacted him quickly so he give me guaranty that his herbal medicine will cure my cancer and i will be heal forever I said Okay.I ask him about the process for the cure,he ask me to pay for the fees which i did and within 7 working days he sent me the herbal medicine then he instructed me on how to drink it for two weeks to cure.I told Gomez my friend about the herbal medicine so he gave me go ahead to drink it.So after drinking it for two weeks i was cured I'm so grateful and i promise i will recommend anyone with cancer to him and that what i'm doing.Dr Itua Herbal Medicine makes me believes there is a hope for people suffering from,Parkinson's disease,Schizophrenia,Cancer,Scoliosis,Bladder Cancer,Colorectal Cancer,Breast Cancer,Kidney Cancer,Leukemia,Lung Cancer,Skin Cancer,Uterine Cancer,Prostate Cancer,Fibromyalgia,a
ResponderEliminarSyndrome Fibrodysplasia ,Epilepsy Dupuytren's disease, Diabetes ,Coeliac disease, Angiopathy, Ataxia,Arthritis,Amyotrophic Lateral Sclerosis,Alzheimer's disease,Adrenocortical carcinoma.Asthma,Allergic diseases.Hiv_ Aids,Herpes,Inflammatory bowel disease ,Copd,Diabetes.
Here Is His Contact Info......[Email...drituaherbalcenter@gmail.com/ info@drituaherbalcenter.com. Whatsapp...+2348149277967]