Plexopathy — Definition and Causes
In Lecturio - Plexopathy is a peripheral neuropathy at the level of the brachial or lumbosacral plexuses leading to sensory, motor or sometimes autonomic deficits. The etiology for this pathology vary from compression, inflammation, or ischemia to radiation.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your neurology course now for free!
Image : “Vasoconstriction – Constricted blood vessel” by Manu5. License: CC BY-SA 4.0
Brachial Plexus Plexopathy
Neuropathy at brachial plexus can result from various causes like inflammations, trauma, malignancies and associated complications.
Anatomy of the brachial plexus
Nerve roots from the cervical spine merge to form the brachial plexus, which supplies both upper limbs. The roots fuse to form trunks, divisions then cords and finally nerves. There are three trunks in the brachial plexus: upper, middle and lower.
The upper trunk is formed by C5 & C6, while the middle trunk is formed by C7 and the lower trunk is formed by C8 & T1 nerve roots. The upper and middle trunks both divide and give branches to the posterior and lateral cords. The lower trunk gives branches to the posterior and medial cords.
The medial cord gives rise to the ulnar nerve, while the lateral cord forms the musculoskeletal nerve and the posterior cord forms the radial nerve and the axillary nerve. The median nerve is formed by both the medial and lateral cords. The brachial plexus has sensory fibers, motor fibers and autonomic fibers from the vertebral ganglia.
Etiology of brachial plexopathy
Thoracic outlet syndrome (TOS)Thoracic outlet syndrome can be vascular or neurogenic. Neurogenic thoracic outlet syndrome is more common in females with weakness and atrophy of the intrinsic muscles of the hand and numbness in the distribution of the ulnar nerve. The syndrome is caused by traction injury of the lower brachial plexus over the elongated transverse process of the 7th cervical vertebra or a cervical rib.
Vascular TOS occurs due to compression of the subclavian vessels with a different clinical picture of claudications and venous thrombosis. Nerve conduction studies will show diminished conduction in the lower branches or the brachial plexus, especially with T1 root.
Imaging studies may help identify the cause of neurogenic compression. Treatment is mainly surgical to release the compression.
Hereditary brachial plexopathy
This autosomal dominant genetic mutation of the Septin 9 gene leads to recurrent attacks of pain, parenthesia, weakness and autonomic manifestation in the distribution of the brachial plexus. Lumbar plexus, phrenic nerve and laryngeal nerve can also be affected. Long-lasting weakness may occur with muscle atrophy. Other features include short stature, neck creases and skin folds. Nerve studies show a delay in motor conduction.
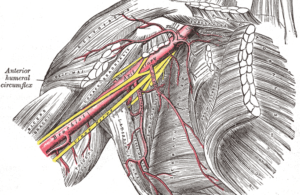
Image: “The axillary artery and its branches in the brachial plexus.” by Henry Vandyke Carter, Henry Gray (1918): Anatomy of the Human Body. Bartleby.com: Gray’s Anatomy, Plate 523. License: Public Domain
The etiology of plexopathy is due to iatrogenic traction of the fetal head during delivery, especially with shoulder dystocia. It can be divided into erb palsy and total brachial palsy.
Erb palsy involves C5, C6 and sometimes C7. The deformity adduction, internal rotation with the extension of the arm and forearm. The wrist and fingers are flexed in case of C7 involvement.
Total brachial palsy with the involvement of all brachial plexus roots from C5 to T1 manifests with arm paralysis and Horner’s syndrome. The diagnosis is made after birth with typical clinical presentation and conduction studies. Treatment is mainly physical therapy until the recovery of the nerve function. Few cases may fail to recover after one year and need surgical intervention.
Neoplastic brachial plexopathy
The most common causes for neoplastic brachial plexopathy are invasive lung and breast cancers. Pancoast syndrome presents with pain and weakness in the lower brachial plexus distribution and Horner’s syndrome due to pressure from non-small cell lung cancer in the lung apex.
The clinical picture of brachial plexopathy included pain and numbness in the upper limb with muscle weakness, atrophy and diminished deep tendon reflexes.
Brachial neuritis
This is also called Parsonage-Turner syndrome. It is an idiopathic or inherited form of brachial plexopathy with severe shoulder pain followed by muscle weakness and atrophy. Numbness and weakness occur in the distribution of the brachial plexus. Treatment is supportive with analgesics and physical therapy.
Prognosis of brachial plexopathy
Prognosis depends on the site of injury. Prognosis is good if there is isolated injury to upper trunk. Hornor’s syndrome may occasionally have good prognosis.Following types have poor prognosis:
- Injury to complete plexus
- Isolated injuries to upper roots, cords, and lower trunks
- Persistence of pain more than six months regardless of the site of injury
- pseudomeningocele
Lumbosacral Plexopathy
Anatomy of the lumbosacral plexus
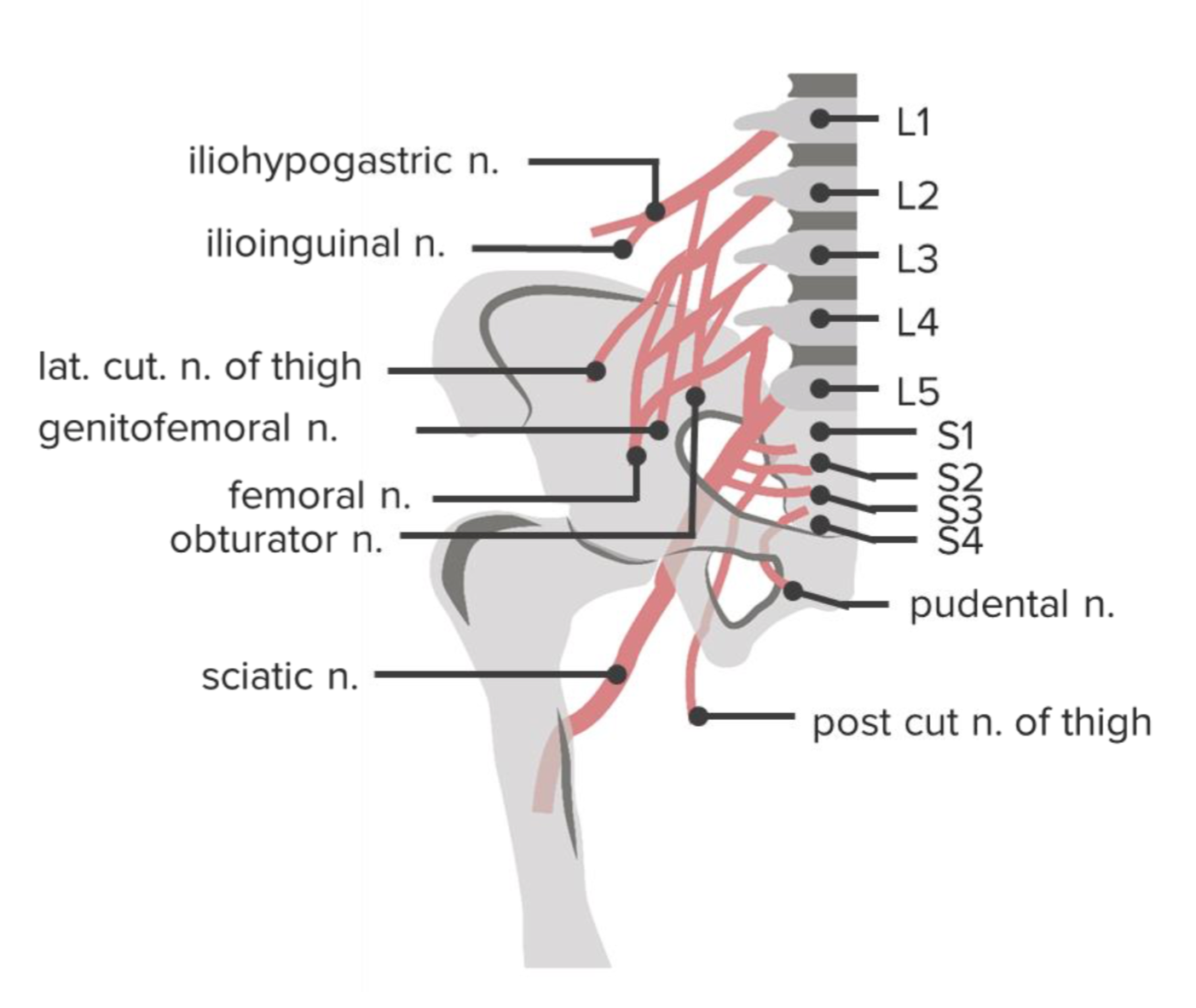
The lumbar plexus is formed by the anterior rami of the nerve roots from L1 to L4 lumbar spine. They divide within the psoas major muscle into anterior and posterior branches.
Posterior braches from L2 to L4 form the femoral nerve, which runs from the lateral border of the psoas muscle to the anterior compartment of the thigh below the inguinal ligament. The obturator nerve is formed by the anterior branches and exits the medial side of the psoas to the obturator foramen and finally to the medial aspect of the thigh.
Small branches of the lumbar plexus include the ilioinguinal nerve, genitofemoral nerve, iliohypogastric nerve and lateral femoral cutaneous nerve of the thigh.
The sacral plexus is formed by the anterior rami of the S1-S4 nerve roots. The lumbar plexus is connected to the sacral plexus with the lumbosacral trunk, which is formed by the L4 and L5 nerve roots.
S1 & S2, with the posterior division of the lumbosacral trunk, form the peroneal division of the sciatic nerve, while the tibial division of the sciatic nerve is formed by the anterior branches. Small nerves from the sacral plexus include the pudendal nerve, the posterior cutaneous nerve of the thigh and gluteal nerves.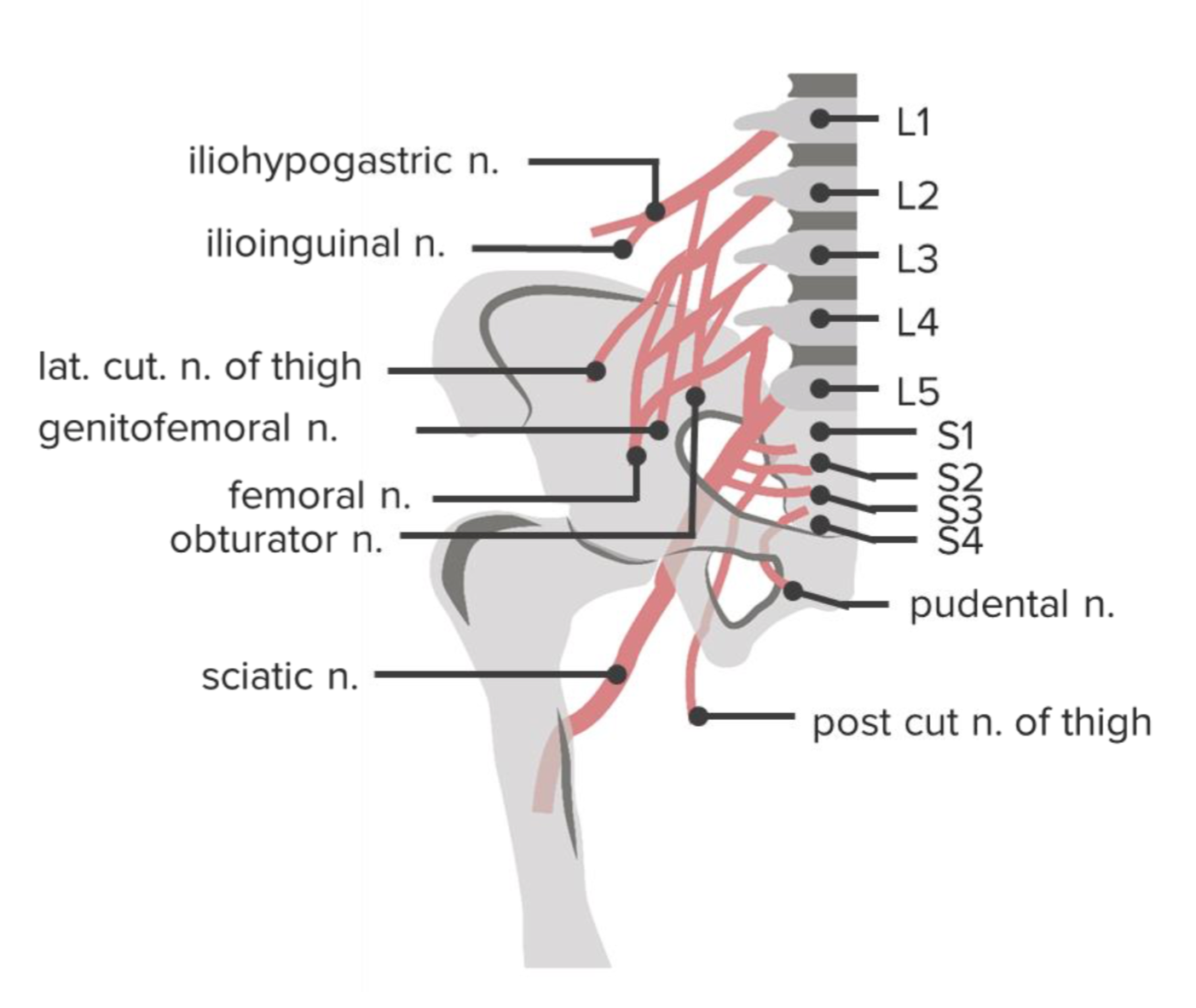
Clinical picture of lumbosacral plexopathy
Upper lesions involving the lumbar plexus are most likely to present with paresis in hip flexion and adduction and knee extension, as well as parethesia in the anteromedial thigh and medial leg, while lesions involving the lumbosacral trunk or the sacral plexus present with paresis of knee flexion, foot drop and hip abduction with paraethesia of the leg, dorsum of the foot, posterior thigh and perineum.Etiology of lumbosacral plexopathy
Retroperitoneal hematoma
This is common in the psoas muscle due to anticoagulation therapy with iatrogenic femoral vein dialysis or catheterization. The hematoma causes compression of the upper lumbosacral plexus, leading to weakness in the knee flexion, hip adduction and flexion. Paresthesia in the anteromedial thigh will be due to sensory involvement.
Imaging for retroperitoneal hematoma is better with CT or MRI. Treatment is mainly conservative with good prognosis. Few patients will need surgical evacuation or will continue with mild neurological sequelae.
Diabetic amyotrophy
Diabetic amyotrophy affects lumbosacral plexus and peripheral nerves in diabetic patients. They present with acute progressive pain, weakness and autonomic loss in the proximal legs asymmetrically with weight loss. The disease is self-limited and recovery is the rule.
Peripartum plexopathy
Lumbosacral plexopathy associated with gestation and delivery. Antepartum plexopathy occurs from pressure of the gravid uterus on the upper part of the plexus, leading to weakness of adduction and flexion of the hip and numbness or the anteromedial thigh.
During fetal delivery, the involvement of the lumbosacral trunk is more common due to its compression against the bony pelvis. The patient presents with foot drop and numbness of the dorsum of the foot and lateral foreleg. The prognosis is excellent with complete recovery within a few months.
Neoplastic
Direct and distant spread of benign and malignant tumors from colon, lung, breast, spine, sarcoma, prostate, hematological and gynecological tumors to the lumbosacral plexus is a common cause of plexopathy.
Patients present with severe pain that is aggravated by positional changes, straining and weight bearing. Parethesia and weakness along the nerve distribution follow. Treatment and response to therapy differ according to the neoplasm involved.
Lumbosacral plexopathy is common with pelvic and sacral fractures, as well as inflammatory conditions involving with cytomegalovirus, HIV and tuberculosis. Chronic inflammation associated with rheumatic diseases can also lead to lumbosacral neuropathy with varying clinical presentation.
Post-surgical Lumbosacral Plexopathy
Lumbosacral plexus can get injured as a sequel of surgeries like hysterectomy, hip joint surgeries and surgical removal of tumors in corresponding regions. Neuropathies occur as a result of compression, stretching, cutting and scraping as result of surgery.
Post-surgical Lumbosacral Plexopathy
Lumbosacral plexus can get injured as a sequel of surgeries like hysterectomy, hip joint surgeries and surgical removal of tumors in corresponding regions. Neuropathies occur as a result of compression, stretching, cutting and scraping as result of surgery.
Comentários
Enviar um comentário