Female Reproductive Organs – Follicle Maturation, Mucous Membranes and Mammary Gland Tissue
In Lecturio _ A number of hormone-mediated processes take place in the female genitals. The follicle maturation in the uterus, formation of the mammary gland tissue and lactation are processes that are basic knowledge to medical students. In the following, the most important facts are listed. Afterwards you can use the three exam questions to control your knowledge.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your physiology course now for free!
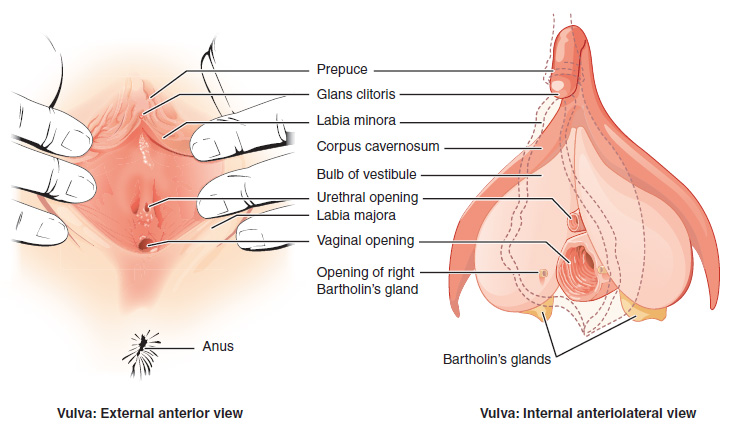
Introduction to Female Genitalia
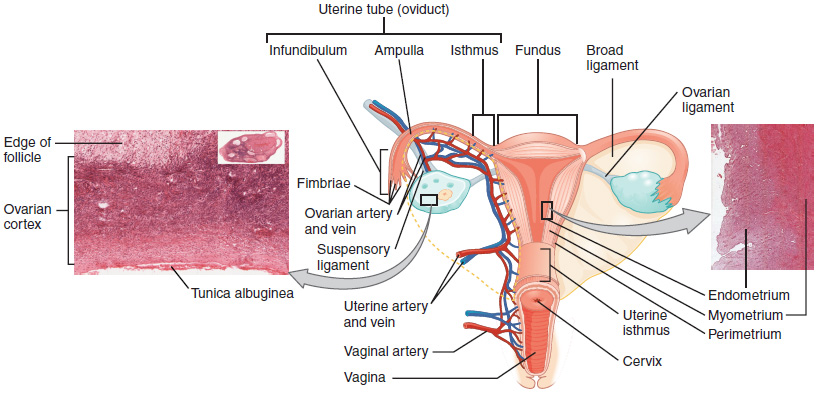
Female reproductive organs are divided into internal and external genital organs. The internal female reproductive organs are composed of the ovary, the fallopian tube, the womb (uterus) and the vagina. The external female genitals are referred to as the vulva. The external genitalia consist of the clitoris, the vulvar vestibule, the vulvar vestibule glands, the labia minora and the labia majora. The uterus is also classified as a part of the genitals, even if it is not visible from the outside. The female breasts, however, are classified as a secondary genital.Follicles and Follicle Maturation Influenced by Hormones
The follicle formation takes place in the ovaries – the female gonads. The ovary is reminiscent of the shape and size of a plum and contains already at birth the full amount of lifelong available oocytes. That is about 200,000 immature oocytes per ovary.During the reproductive period throughout the lifetime of any female, about 400 to 500 oocytes mature influenced by hormones. After ovulation the oocytes can be fertilized. In their mature state the fallopian tubes are each about 4 cm long, 2 cm wide and 1 cm thick. During menopause the size is constantly changing until it reaches its final size which is comparable to an almond. The ovaries are located in the inner pelvis walls on the right and left side of the lesser pelvis.
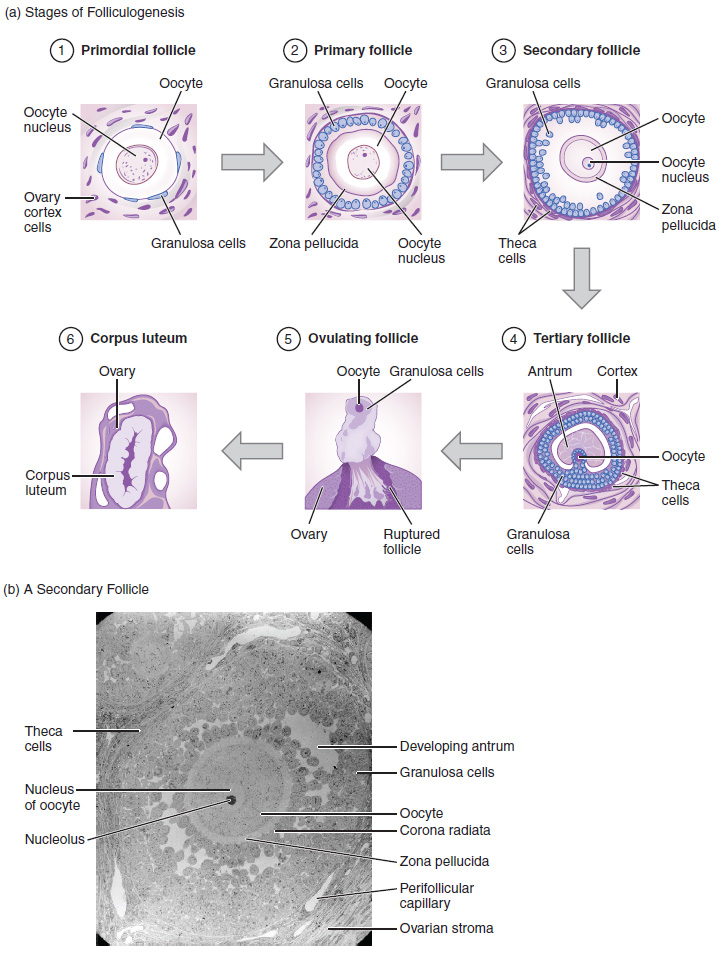
The follicle maturation
The first day of the menstrual bleeding is always classified as the beginning of a new cycle. Nevertheless, it is an ongoing process with flowing transitions. Follicles (vesicles) encase each oocyte. This first phase of follicle maturation is described as the previous cycle. In the second half of the cycle, more follicles develop as well, that e.g., can be visualized by ultrasound. They are called antral follicles.Normally, only one follicle reaches fully maturity. The remaining follicles gradually form back. The fully matured follicle has a size of about 2 cm. It reaches this size at about the 14th day of the cycle. The growing follicle exerts pressure on the environment causing the case to rupture and the oocyte to be released. In this phase, the fallopian tube meets the oocyte and can accommodate the released egg. From there, it is transported through the Fallopian tube to the uterus, where this process is supported by fine hair like projections and muscles.
Hormonal control of follicular growth and maturation
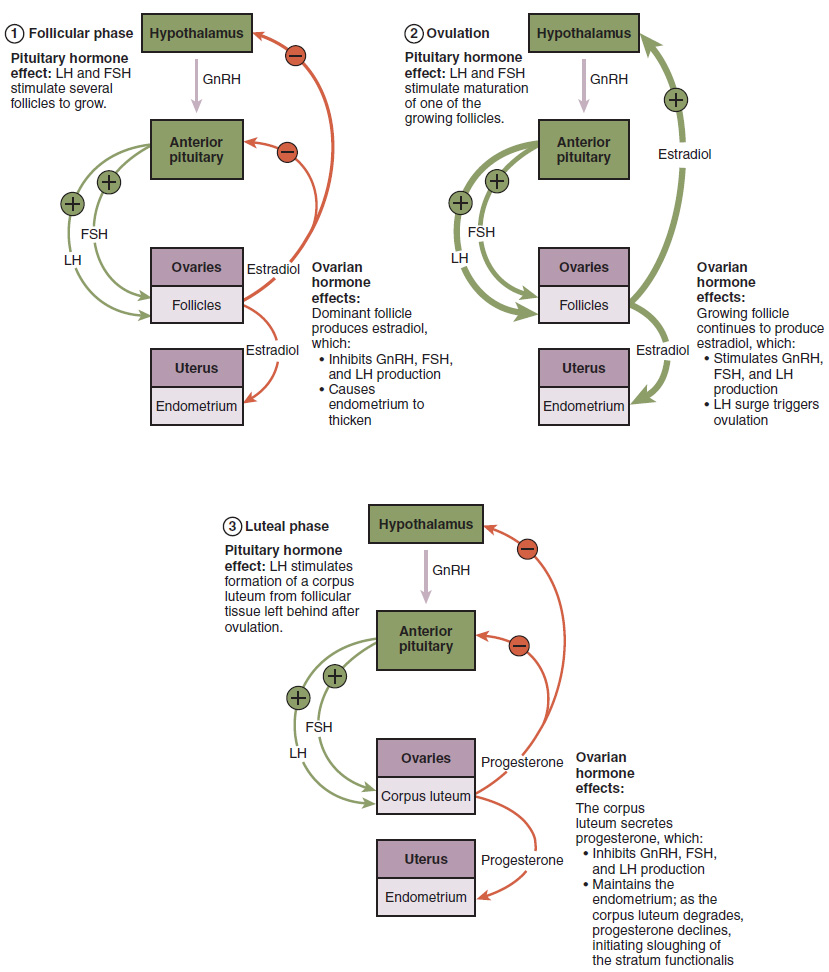
The menstrual cycle and its follicle formation are hormonally controlled. Hormones influence each other at the level of midbrain (hypothalamus), pituitary gland (hypophysis) and ovary.The gonadotropin-releasing hormone (GnRH)
The gonadotropin-releasing hormone (GnRH) is produced (synthesized) in the hypothalamus. GnRH is also known as neuro-secretion. Its function is to stimulate the release of further hormones. These hormones are called gonadotropins. GnRH is a peptide hormone, composed of 10 amino acids. It is transported to the anterior pituitary via the portal system. Approximately every three hours GnRH is cyclically released. However underproduction can contribute to diseases. One being, amenorrhea , in which the menstrual period doesn’t occur.
Follicle-stimulating hormone (FSH)
FSH is known as the follicle-stimulating hormone, also called follitropin. Together with LH, it controls the maturation of follicles and estrogen production.
Luteinizing hormone (LH)
LH is a luteinizing hormone that is also known as lutropin. It is synthesized in the hypophysis and controls, together with FSH, follicle maturation and ovulation. Furthermore, it is necessary for the production of estrogen and progesterone.
Estrogen
The hormone estrogen is of importance for the formation of secondary sexual characteristics. Additionally, it promotes the vagina’s healthy flora and aids in the formation of the uterine lining (endometrium). The follicle maturation is also influenced indirectly by this hormone. Estradiol 2 (E2) is another type of this hormone. It is produced in the ovaries and in the placenta as well during pregnancy.
Progesterone
Progesterone is also known as corpus luteum hormone. It belongs to the gestagen group and is synthesized in the ovaries’ corpus luteum. Progesterone is necessary for the oocytes’ implantation. Furthermore, it maintains pregnancy, stimulated by LH.
The Stages of Follicle Formation
The follicles process through different stages in which the follicle designations change as well.The primordial follicle
Primordial follicle derives from primary oocytes. Its epithelium is flat and consists of one layer.The primary follicle
The primary follicle forms a gap between the oocyte and the follicle cells. In this interspace extracellular material is deposited. Primary follicles absorb proteins and accumulate fat. Therefore, their volume increases with formation decreasing at the age of 35.The secondary follicles
In case of the secondary follicle the epithelium consists of five layers. These layers are composed of interconnected high prismatic cells. Gaps between the cells are possible. The gap between the oocyte and follicle cells persists as well. Here, the zona pelludica originates, which consists of basement membrane material. In addition, the theca folliculi (also called theca organ) forms in this stage. It derives from stromal cells that in turn enclose the follicle cells.The tertiary follicle
The tertiary follicle measures about 1 cm and is surrounded by 6-12 layers. The gaps are further grown (follicle antrum) and are filled with follicular fluid (liquor folliculi). This is produced by granulosa cells and contains hyaluronic acid. The theca folliculi consists of two layers. One, the theca interna which produces steroidal hormones that affect the endometrium. Two, the theca externa consisting of cells similar to muscles. It also contains blood vessels and reticular fibers.The graafian follicle
The graafian follicle measures about 1 centimeter. With the graafian follicle the follicle maturation ends. The gaps form the follicle antrum, also called antrum folliculi. Further, it is filled with the follicular fluid. Now, the oocyte is in a hill-shaped protrusion that is described as cumulus oophorus. Once the oocyte removes from that hill, it is freely floating in liquid, with theca interna and externa still present. Finally, the case raptures and the oocyte releases. The ovulation occurs, while the theca interna and externa, as well as the granulosa cells, form the corpus luteum. In the ovary, maturity levels are detectable as long as the woman is still fertile.Uterus With Endometrium, Myometrium and Perimetrium
The uterus holds and feeds the embryo, provides enough space and supports the process of birth. It is a hollow organ having strong muscles and a shape of a pear. It is composed of three layers, the inner endometrium, the myometrium and the perimetrium. The endometrium is the uterine lining consisting of mucous membrane. It consists of a single-layer covering epithelium and connective tissue stroma. The endometrium is interlocked with the myometrium.The endometrium (tunica mucosa)
The endometrium is a mucosal membrane, where the fertilized oocyte implants. It assembles and disassembles cyclically under influence of gestagen and estrogen. This rebuild occurs in phases, namely the proliferation phase, the secretion phase, the premenstrual period and menstruation. In addition, the endometrium is the place of placental development. The endometrium contains the uterine glands. The lamina propria mucosae including the functional stratum, is subjected to cyclic changes too. The basal layer (stratum basale), which is the myometrium´s barrier, is also part of the endometrium.The myometrium (tunica muscularis)
The myometrium is the uterus wall’s middle layer. It mainly consists of smooth muscles, which are spirally arranged, but also of supporting connective tissue and vessels. Muscles are able to provide strong contractions as it is necessary during birth. The myometrium contracts after birth as well, to expel the placenta. The aim is to keep the blood loss at a minimum. The myometrium is composed of the outer muscle layer, the stratum vasculosum, including vessel-rich connective tissue, and the inner muscle layer. The myometrium is susceptible to benign growth, so-called myomas.The perimetrium (tunica serosa)
The perimetrium is the uterus wall’s outer layer. Outwards, it encloses the uterus towards the abdominal cavity. Together with the tela subserosa it serves as a sliding layer.The Female Breast
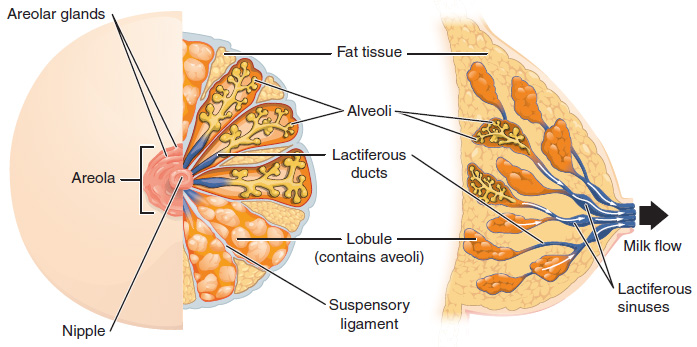
The female breast serves the infant´s nutrition and is a secondary sexual organ. Shape and size depends on various factors and changes during the cycle and a woman’s whole life. Under the influence of estrogen and gestagen, the tissue is better supplied with blood. Additionally, water accumulates and, thus, causes volume increase.Structue of the mammary (breast)
The mammary is mainly composed of fatty tissue (about 80 % in case of non-breastfeeding woman) and connective tissue. It includes the milk-producing gland tissue (glandula mammaria), that consist of 15 to 20 lobules (lobuli). The lobuli are connected to the nipple (mammilla) by the milk ducts (ducti). At the end of the milk ducts are the lactiferous sinus (sinus lactiferi), which excretes milk while breastfeeding and serves as a milk reservoir. The areola allows an exclusion of air and, thus, helps the infant with suckling.Glands within the mammary
The mammary is the mammary gland. It is composed of 10 to 20 individual glands. Each has an own main efferent duct, the main is the lactiferous duct (ductus lactifer colligens). The glands are described as tree-branch vesicles that are separated by the stroma (fat- and connective tissue). The resulting sections are the lobes (lobi). The lobes are divided into lobules.At the end of the lobules (alveoli), milk is produced in the case of breastfeeding woman. This process is triggered by the hormones prolactin and oxytocin. Progesterone is the hormone that already prepares the body for lactation during pregnancy. The development occurs during adolescence which is influenced by hormones. The scent glands, by the release of pheromones, help the infant to find the breast.
Pheromones are attractants. Here the Montgomery glands become visible as elevations on the mammilla. The mammilla itself is interspersed by a network of muscle fibers. It contracts when touched, at which the nipple gets bigger. Therefore, the allowing the infant to suck with ease.
Common Disease of the Uterus
 The two inner layers of the uterus, the endometrium and the myometrium are susceptible to proliferation. In case of the endometrium we refer to this as endometriosis. This is a benign condition, but can develop to be painful and at worst, spreads to other organs.
The two inner layers of the uterus, the endometrium and the myometrium are susceptible to proliferation. In case of the endometrium we refer to this as endometriosis. This is a benign condition, but can develop to be painful and at worst, spreads to other organs.This mostly involves endometrial growths that originate simultaneously with the endometrium during the cycle. Endometriosis can result in permanent pain and is often associated with cyst formation. Its progress can also be asymptomatic and, thus, an identical finding. Endometriosis can cause infertility. If untreated it gets worse until menopause. It can be treated by means of hormones. In case of doubt, a surgical procedure is necessary.
Diseases of the Female Breast
Image: “Cytopathology of infiltrating duct carcinoma breast” by – Government Medical College, Kozhikode. License: CC BY-SA 4.0
The classification is divided into non-invasive, invasive and others. The risk of metastasis is high. Lung, bones, liver and adrenal glands as well as the brain are especially affected. The treatment depends on various factors, in case of a surgical therapy, the regional lymph nodes are also removed and the effort is to avoid a breast amputation (masectomy).
Review Questions
The solutions are below the references.1. Which statement is correct?
- GnRH is derived from the pituitary gland.
- Amenorrhea is the consequence of LH deficiency.
- The cycle begins on the first day without bleeding.
- GnRH is a peptide hormone.
- GnRH acts directly on the follicular maturation.
- Graafian follicle is another word for tertiary follicle.
- Theca interna and externa are cellular waste.
- FSH is also known as follitropin.
- Theca interna produces no hormones.
- Tertiary follicle has a size of about 0.5 cm.
- The endometrium is gland tissue.
- The endometrium contains the uterine glands.
- The endometrium consists of connective tissue.
- The endometrium’s structure is always the same.
- The endometrium contains spiral muscles.
Comentários
Enviar um comentário