Abnormal Looking Cervix: Cervical Fibroids and Cancer and Ectropion
Table of Contents
Image: “This is a picture of a cervix of a lactating woman with no STDs and who has given birth vaginally twice” by Ep11904. License: Public Domain
Normal Looking Cervix
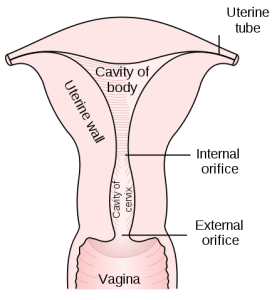
Image: “Posterior half of uterus and upper part of vagina” by Henry Gray. License: Public Domain
The cervix is normally fusiform in shape, with narrow external and internal oses. The portio vaginalis is the visible portion of the cervix that protrudes into the vagina. The outer portion of the ectocervix is covered by smooth, pink, nonkeratinized squamous epitheliumthat embryologically originates from the vaginal plate. The central portion of the ectocervix is lined by simple columnar epithelium, the same lining of the endocervix, which originates from Mullerian tissue. A Line of demarcation can be identified between the pale pink squamous epithelium and the bright red columnar epithelium. It bears the name squamocolumnar junction.
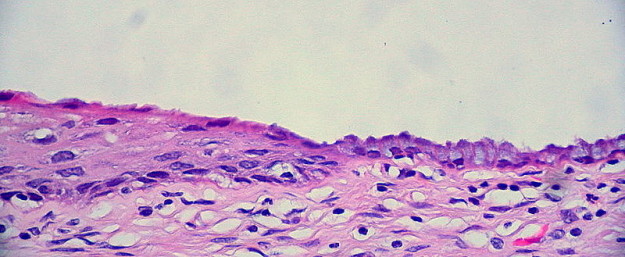
Image: “An unusually “clean” squamocolumnar junction of the uterine cervix, representing the boundary between the exocervix on the left, and the endocervix on the right. This is the “hot spot” where the tiny seedlings of dysplasia grow into the mighty oaks of cervical cancer. Accordingly, it’s important to sample this area while collecting a Pap smear specimen.” by Ed Uthman. License: CC BY 2.0
The original squamocolumnar junction represents the embryologically designated junction between the squamous and columnar epithelium. It’s usually seen during adolescence and a woman’s first pregnancy as the uterus and vagina enlarge, resulting in evertion of the endocervix. In postmenopausal women, the squamocolumnar junction may be high in the canal and cannot be seen.
A new squamocolumnar junction can be derived from squamous metaplasia of the columnar epithelium that covers the central ectocervix, thus moving the junction progressively closer to the external os and then up the endocervical canal.
The transformation zone is an area of cuboidal subcolumnar epithelium that can develop into either columnar or squamous epithelium. It is located between the original and the new squamocolumnar junction.
Approach to an Abnormal Looking Cervix
An abnormal looking cervix should be examined carefully using colposcopy under stereoscopic binocular magnification to identify the possible etiologies and exclude the cancerous lesions which may require further clinical evaluation. The possible causes of the suspicious cervix can be classified according to the etiological mechanisms into physiological, infectious, abnormal growth and iatrogenic.
Physiological
The gynecologist should first exclude the physiological conditions that can result in an abnormal looking cervix.

Image: “A nulliparous, post-menarchal woman’s cervix viewed on speculum exam with asymptomatic ectropion.” by GynaeImages. License: CC BY-SA 4.0
Ectropion
Ectropion occurs when endocervical evertion exposes a significant proportion of columnar epithelium that has a reddish appearance, similar to granulation tissue, giving the appearance of an erosion. This is seen as a central area of velvety redness surrounding the external os. Suspicious lesions should be biopsied to exclude malignancy.
Atrophic cervicitis
Physiological depletion of the ovarian follicles after menopause results in a significant decrease in the levels of estrogen hormone. The lack of estrogen causes atrophy and thinning of the cervical epithelium. Speculum examination reveals a pale epithelium with patches of erythema that may bleed easily on contact. The pH of vaginal discharge is less acidic (pH of 4.7 or higher). The possibility of a coexistent neoplasm should be excluded. Topical estrogen therapy for two to three months can reverse these changes.
Nabothian cysts

Image: “Nabothian cysts in a specimen of the uterus” by Ed Uthman. License: CC BY-SA 2.0
They are cystic structures that form when a portion of columnar epithelium becomes covered with squamous cells. The underlying islands of active columnar tissue continue to secrete mucoid material,which becomes entrapped forming retention cysts. These cysts vary in number and size from microscopic to large clusters of cysts, distorting the appearance of the cervix. They can be translucent, or opaque yellowish/whitish cysts, with branching blood vesselsrunning over their surfaces. They are usually asymptomatic but may cause pain during intercourse (dyspareunia).
Abnormal growth
If non-cystic cervical mass was observed during the examination, gynecologists should first exclude the possibility of cervical neoplasms. Other cervical growths include polyps and cervical fibroids.
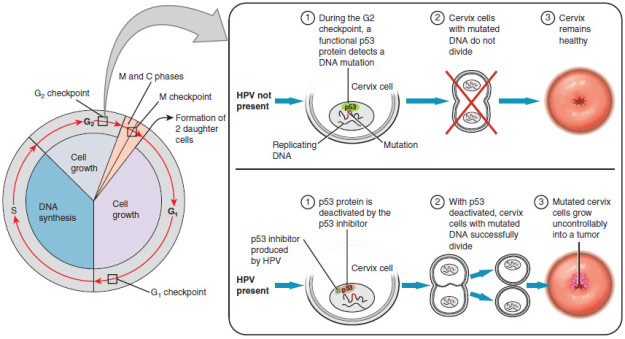
Cervical cancer
Invasive cervical carcinoma first appears as focally ulcerated and indurated lesions with a friable necrotic mass that bleeds easily on touch. Advanced lesions can be exophytic, endophytic or infiltrative. Suspected lesions should be examined carefully, especially in high-risk patients. Cervical Intraepithelial Neoplasia (CIN) is a spectrum of pre-malignant lesions that can be detected only by pap smears.
Cervical polyps
These are single or multiple reddish, soft pedunculated polyps, resulting from hyperplasia of the endocervical columnar epithelium due to chronic inflammation of the cervical canal. The pedicle is usually long and thin but may also be short and broad-based. Symptomatic polyps should be removed and sent to the laboratory for histological study.
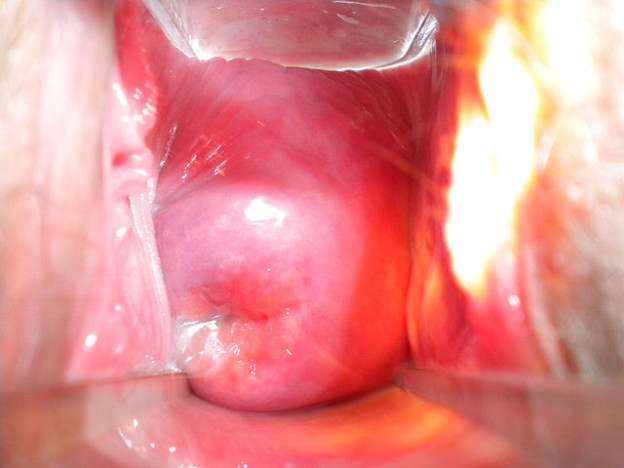
Cervical fibroids
Fibroids (Leiomyomas) are well-circumscribed benign tumors of the uterine smooth muscles that usually run a very slow progressive course. Cervical fibroids may arise from the cervix itself or from the uterine submucosal fibroids that may elongate and project downward into the vagina through the cervical os. The fibroids are firm, smooth and non-tender on palpation. Menorrhagia and dysmenorrhea are the commonest presentation and occur most commonly with submucosal type.
Infectious
Bacterial vaginosis
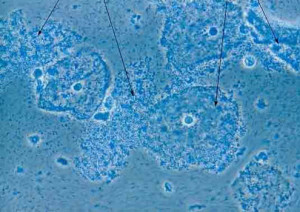
Image: “Bacterial vaginosis” by Per Grinsted / Medicinsk Webdesign. License: CC BY-SA 3.0
Bacterial vaginosis is a common bacterial vaginal infection, which represents a state of unexplained alteration of the normal vaginal flora, resulting from overgrowth of the normal inhabitants (anaerobic bacteria) of the vagina, such as Gardnerella Vaginalis (GV). It commonly presents with non-irritant, malodorous vaginal discharge, which is a characteristically thin, homogeneous, fishy-smelling, gray vaginal discharge, especially noticeable around the time of menses or following sexual intercourse. The diagnosis is based on the presence of clue cells on saline wet mount smears, vaginal pH > 4.5 and fishy odor with the addition of 10 % KOH. It responds well to metronidazole.
Trichomoniasis
Trichomoniasis is a common cause of vulvovaginitis, which is caused by Trichomonas Vaginalis (TV), an ovoid, motile and flagellated protozoon. It is a common sexually transmitted infection that characteristically presents with profuse, frothy, yellow malodorous vaginal discharge with vulvar irritation. Speculum examination may reveal subepithelial redness of the cervix (strawberry cervix), in which certain red areas can be identified colposcopically.
The diagnosis is based on the presence of motile trichomonads and WBCs on saline wet mount smears, vaginal pH > 4.5 and amine odor with 10 % KOH. Application of Schiller’s Iodine gives Leopard skin appearance. It responds well to metronidazole.
Candidiasis
Candidiasis is a fungal infection of the vulva and vagina. In 90 % of the cases, it is caused by the normal inhabitants of candida albicans, especially when host immunity is reduced. Patients typically present with intense pruritus, a vaginal burning sensation that may cause discomfort, and scanty thick white vaginal discharge. Although candidal infection can be identified clinically, diagnosis is based mainly on the presence of pseudo-hyphae, with budding yeast on KOH wet mount smears.
Herpes simplex infection
Herpes simplex virus (HSV) type II primarily infects the anogenital tract. It is considered the most common cause of ulcerative genital lesions. HSV typically presents with multiple, superficial, painful ulcerations of the vagina and cervix, making the cervix extremely abnormal; may be misdiagnosed with invasive cervical cancer. In contrast to cervical cancer, HSV infections are painful, recurrent and resolve spontaneously within 2—4 weeks.
Genital warts or condylomata accuminate
Genital warts are the most common sexually transmitted viral infection, and in 90 % of the cases, it is caused by human papillomavirus (HPV) type 6 and 11. They present as either flat or large exophytic (cauliflower-like) papules or nodules on the moist surfaces of the vulvovaginal and cervix, causing itching and burning pain. Suspicious clinical diagnosis can be confirmed with a colposcopy-directed cervical biopsy.
Iatrogenic
Iatrogenic scarring of the cervix can be caused by previous cervical surgery or other procedures. The gross appearance is based on the extent of cervical scarring. Minimal scarringmay present as circumferentially raised pale tissue around the os, while more extensive scarring may result in distortion of the cervix. Cervical stenosis is a common complication which occurs in 1—2 % of patients. Due to contraction of the scar tissue, it may result in secondary amenorrhea and hematometra in severe stenosis.
My name is Angelo Alex I was tested HIV/Herpes positive and I was so worried am I going to die soon. I made my search on herbal remedy for Std, then I found lots of testimonies on how Dr James Herbal Medicine Cured HIV/Aids, and other diseases like,Yeast infection, Rectum effects, intestine damage, bowel obstruction, Ovarian disease, Cancer, hypothyroidism, Herpes, COPD, HIV, Arthritis, Lyme disease,Hpv, Infections,Liver Disease, Autoimmune Diseases, Parkinson's disease,Lupus,Nephrology and Hypertension, Neurology, Obstetrics, Gynecology, and Women's Health, Oncology, Pediatrics, Pulmonary, ACUTE MYELOFIBROSIS, ALZHEIMER's symptoms, BREAST CANCER, DIABETES, HAIR LOSS AND HAIR TREATMENT, KIDNEY DISEASES, LEUKEMIA, MYELOID LEUKEMIA, STEM CELL TREATMENT On websites sharing their testimonies, which made much more sense to me. All the authors pronounce Dr James As a man with Good Heart, I picked interest in their testimonies and I contact him about my situation then he gave me procedure how it works, I proceed after one week he courier his Herbal Medicine to me and instructed me on how to drink it for two weeks to cure. I received His Herbal Medicine so I drank it for two weeks as I was told then after 2 weeks of drinking his medicine, I went for a test I found out I was cured from HIV/Aids & Herpes Virus, I pay homage to him 2 months ago to his country to celebrate with him on his African festival which he told me it usually happens every year. I know there are lots of (HIV)/Aids Herpes Virus denials of Herbal Remedy movement the same few doctors and they represent a very small fraction of the community. I could have died because I refused Natural Herbs Cures for so long, but luckily, by the grace of God I am alive to tell my story. Contact Info...Whatsapp Number...+2348152855846,Email...drjamesherbalmix@gmail.com
ResponderEliminarjust to make the story short, few weeks ago i founded a herbalist Dr. online who has cured thousand of Herpes virus patients with 100% excellent result and i inquire the treatment for me and my husband taking it for two weeks and we got cured i just want to use this medium to thanks Dr Ogedegbe for his wonderful treatment he so-much saved us from this virus his information has been attached to my post you can reach out to him via: dr.ogedegbe6@gmail.com, whatsapp number +2348109374702 . Thanks to you Dr Ogedegbe for curing me and my husband from this deadly virus.he also cure the following ......HPV....ALS...COPD...CANCER......DIABETES.......
ResponderEliminar