Erectile Dysfunction (ED; Impotence) — Symptoms and Diagnosis
Table of Contents
- Definition of Erectile Dysfunction and Peyronie’s Disease
- Epidemiology of Erectile Dysfunction and Peyronie’s Disease
- Etiology and Pathophysiology of Erectile Dysfunction and Peyronie’s Disease
- Clinical Presentation of Erectile Dysfunction and Peyronie’s Disease
- Diagnostic Work-up for Erectile Dysfunction and Peyronie’s Disease
- Treatment of Erectile Dysfunction and Peyronie’s Disease
- References
Image: “Viagra in pack.” by user:SElefant. License: CC BY-SA 3.0
Definition of Erectile Dysfunction and Peyronie’s Disease
Erectile dysfunction can be defined as the inability to get a penile erection or to maintain erection that would adversely affect vaginal sexual intercourse. Erectile dysfunction is one of the problems encountered in men with Peyronie’s disease.
Peyronie’s disease is a penile condition that presents with a palpable plaque and an abnormally increased curvature of the penis when erect. This is associated with painful erections and/or erectile dysfunction.
Epidemiology of Erectile Dysfunction and Peyronie’s Disease
The prevalence of erectile dysfunction is age dependent. Prevalence is estimated to be less than 10% in men younger than 4 years of age, approximately 10% in men aged 40 to 49 years, up to 40% in men aged 60 to 69 years and virtually all men aged older than 70 years complain of some form of erectile dysfunction.
The incidence of erectile dysfunction is high and ranges between 26 to 46 per 1,000 men. Coronary artery disease, stroke, smoking, obesity, sleep disorders, diabetes and cardiovascular disease are all linked to an increased risk of erectile dysfunction.
On the other hand, Peyronie’s disease seems to be less common than nonspecific erectile dysfunction and is estimated to have a prevalence of 0.4%. The average age of patients with Peyronie’s disease is approximately 53 years. Approximately, 30% of men with Peyronie’s disease have erectile dysfunction.
Etiology and Pathophysiology of Erectile Dysfunction and Peyronie’s Disease
Etiologies of erectile dysfunction are diverse and first we need to understand the most common causes of Peyronie’s disease before talking about other etiologies of erectile dysfunction in general.
Peyronie’s disease’s most common and well established etiology is sexual trauma to the erect penis. A dorsal or ventral sheer stress can be elicited in the past medical history of most patients with Peyronie’s disease. It is believed that impaired healing along with fibrosis are the main causes of the formation of the penile plaque which is responsible for the increased curvature of the penis and the painful erections in Peyronie’s disease.
Other less common etiologies of Peyronie’s disease include family history of the disease, history of Paget’s disease of the bone and Dupuytren’s contracture.
On the other hand, erectile dysfunction without Peyronie’s disease can be a complication of a diverse myriad of conditions. Central nervous system injury, multiple sclerosis, diabetes polyneuropathy and autonomic neuropathy of any cause can result in erectile dysfunction.
Male hypogonadism regardless of the etiology and hyperprolactinemia have also been linked to an increased risk of erectile dysfunction. Additionally, men with cardiovascular atherosclerotic disease can develop erectile dysfunction.
Beta-blockers, antidepressants, antiandrogens, tobacco smoking and alcoholism are also linked to erectile dysfunction. Patients with systemic diseases such as liver, renal or respiratory failure can have erectile dysfunction.
While the mechanism of erectile dysfunction in atherosclerosis and peripheral neuropathy is understood, the pathogenesis of other etiologies and how they cause erectile dysfunction still needs to be elicited.
Clinical Presentation of Erectile Dysfunction and Peyronie’s Disease
Patients with erectile dysfunction usually present to the clinic with indirect questions about weak erections and whether they are normal in their age or not. Once the subject is opened, it is important to understand whether the patient has erectile dysfunction or premature ejaculation which can be mixed up by most patients.
Additionally, it is important to ask about the normal and physiological morning erections, and whether the patient can have an erection due to sexual thoughts. If the patient can attain an erection in these circumstances but not with his partner, the possibility of psychogenic erectile dysfunction is high.
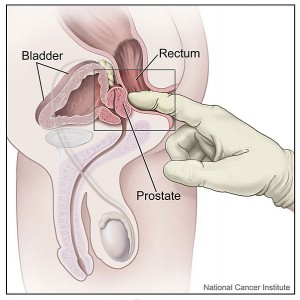
Image: “Digital rectal exam of the prostate.” by Unknown – This image was released by the National Cancer Institute, an agency part of the National Institutes of Health, with the ID 7136. License: Public Domain
Risk factors for erectile dysfunction such as a relevant drug history, alcohol intake and tobacco smoking should be excluded. It is also important to ask about painful erections, increased curvature of the erect penis and history of previous sexual trauma to the penis which can point towards Peyronie’s disease.
Systemic conditions known to be associated with erectile dysfunction such as diabetes, hypertension, multiple sclerosis and polyneuropathy should be excluded. Physical examination should include genital examination to exclude any penile structural abnormalities such as plaques, to assess the prostate via rectal examination, and to exclude male hypogonadism.
Diagnostic Work-up for Erectile Dysfunction and Peyronie’s Disease
Laboratory investigations for erectile dysfunction
It is important to exclude diabetes or hyperglycemia as many patients with type 2 diabetes can present with symptoms and signs of peripheral vascular disease or neuropathy before the establishment of the diagnosis of diabetes. A fasting blood glucose level is therefore indicated.
Testosterone levels should also be checked to exclude male hypogonadism as the cause of erectile dysfunction. Other tests to exclude systemic diseases include liver function tests, kidney function tests and BNP levels to exclude heart failure/cardiovascular disease.
Imaging and more advanced evaluation for erectile dysfunction
Erectile dysfunction is a very subjective symptom and specific sexual questionnaires should be used to objectively evaluate sexual performance and to confirm the diagnosis of erectile dysfunction. These questionnaires exist to confirm the diagnosis of erectile dysfunction but cannot identify the cause of the problem.
The next step would be to exclude vascular causes by performing either an intracavernosal injection of vasodilators that cause tumescence within 10-15 minutes or a color Doppler ultrasound scan. Achieving an erection with injections is indicative of the severity of the erectile dysfunction. Color Doppler ultrasound scans help to diagnose arteriogenic erectile dysfunction.
Patients who are at risk of neurogenic erectile dysfunction due to central nervous system disease or peripheral neuropathy should undergo specific neurologic testing which might include a brain magnetic resonance image, spinal magnetic resonance imaging and/or electromyography studies.
Treatment of Erectile Dysfunction and Peyronie’s Disease
Treatment of erectile dysfunction depends on whether a cause can be identified or not. When the cause is hypogonadism, testosterone can be used. Patients with psychogenic erectile dysfunction benefit from psychotherapy and oral sildenafil therapy, a phosphodiesterase type 5 inhibitor (PDE5 inhibitor), that blocks the degradative action of cGMP-specific phosphodiesterase type 5 (PDE5) on cyclic GMP in the smooth muscle cells lining the blood vessels supplying the corpus cavernosum of the penis.
Obese patients and those who have sleep disturbances benefit from weight reduction and physical exercise. Smokers and alcoholics should be advised to quit or abstain respectively.
If these treatments fail, sildenafil therapy should be tried for most patients who complain of erectile dysfunction. Additionally, adequate glycemic control should be achieved in patients with diabetes.
If sildenafil therapy or other phosphodiesterase type 5 inhibitors fail, intracavernosal injections, intraurethral injections and vacuum constrictive devices should be tried. These treatments of erectile dysfunction carry certain risks such as painful and prolonged erections, hence should be used only as second line therapies.
When all of the above fail, a penile prosthesis can be implanted to achieve adequate penile erections.
Several medical options exist for Peyronie’s disease that can be tried before going for surgical correction. Systemic treatment with vitamin E supplementation, colchicine, tamoxifen and Acetyl-L-carnitine have been all used with variable success in improving sexual performance in men with Peyronie’s disease.
Additionally, intralesional treatments where an injection of a calcium channel blocker such as verapamil, collagenases or interferons can be used in this group of patients. Intralesional treatments are known to decrease and/or reverse fibrosis in the penile plaques and can perhaps alleviate the symptoms of the disease.
When local and systemic therapies fail, surgical treatment is usually indicated in patients with Peyronie’s disease. The goal of surgery in Peyronie’s disease is to achieve a symmetric penis. The penis is usually curved to one side or the other and the procedure involves lengthening the shorter side of the penis or shortening the longer side.
Another option would be a penile prosthesis especially in men with erectile dysfunction due to Peyronie’s disease.

h4che.com
ResponderEliminarfildena-espana
cenforce-espana
vidalista-espana
cenforce-100
tadalista
vidalista
cenforce
nizagara
malegra