Nitrates in the Treatment of Angina and Heart Failure
Table of Contents
- Heart Failure and Angina
- Nitrates in the Treatment of Angina and Heart Failure
- Different Preparation and their Usefulness in the Treatment of Angina and Heart Failure
- Adverse and Side Effects Related to Nitrates
- Contraindication of Nitroglycerin
- Nitrate Tolerance
- Newer Drug for Angina and Heart Failure
- References
Heart Failure and Angina
The ventricle is the chamber of the heart which is responsible for pumping the blood throughout the body. When the ability of the ventricles to fill the blood and pump the bloodoutside the heart is impaired, the condition is known as heart failure. The reason might be the change in the structural and functional feature of the ventricle.
Based on the left ventricular ejection fraction, the heart failure is classified into reduced or preserved ejection fraction heart failure. The other available classification includes chronic or acute heart failure, decompensated or non-decompensated heart failure. In most cases, both of those terminologies are combined. The knowledge about these classifications is very essential, as the treatment is greatly dependent upon this.
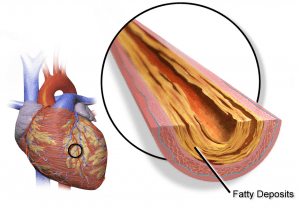
Angina is a state in which blood supply to the parts of the heart is compromised. Angina, when progressed, leads to the development of myocardial infarction (irreversible death of the heart). The nitrates form a group of drugs which are helpful and essential in both angina and heart failure.
Nitrates in the Treatment of Angina and Heart Failure
Functional mechanism of action – anti-anginal effect
The nitrates work by means of causing systemic vasodilation, but predominantly venodilation. The venodilation reduces the preload to the heart.
In addition to this, it also causes coronary vasodilation, which increases the blood supply to the parts of the heart experiencing an ischemic attack. It especially dilates the large coronary arteries, so the ischemic zone gets benefited the most.
The nitrates have an effect on the afterload of the heart, especially at higher doses. There is a decrease in the afterload, thereby decreasing the stress for the heart to pump against resistance. Thus, the three important stresses to the ischemic heart, namely preload, afterload and the decrease in the blood supply to the area per se are targeted by the nitrates.
The collaterals are normally formed, in case of compromised blood supply to any region. The nitrates cause enhancement of the blood flow in the collaterals. The nitrates also have antiplatelet and antithrombotic properties (by means of stimulating the guanylyl cyclase in the platelets, thereby inhibiting the binding of the fibrinogen to the platelet IIb and IIIa receptor).
Functional mechanism of action – treatment of heart failure
The venous and the arterial dilation is the main mechanism for nitrates in the treatment of heart failure. This decreases the preload and afterload to the heart, as discussed earlier.
Biochemical mechanism of action
The nitrates, after entering the cell, get converted into nitric oxide. This conversion occurs in two possible ways. In high potency nitrates (nitroglycerin and nitroprusside), the conversion is caused by the mitochondrial ALDH2 enzyme and, in low potency nitrates (isosorbide dinitrate and isosorbide mononitrate), the conversion occurs with the help of endoplasmic reticulum P450. This nitric oxide, in turn, gets attached to the sulfhydryl group, thereby forming the S-nitrosothiols. The S-nitrosothiols stimulates the Guanylyl cyclase enzyme.
The Guanylyl cyclase is responsible for the conversion of the Guanosine Triphosphate (GTP) to Cyclic Guanosine Monophosphate (CGMP). This CGMP is responsible for the dilation of the smooth muscle of the blood vessel. As the smooth muscle is present in both the arteries, as well as the veins, the nitrates are successful in dilating both.
Pros & cons and the main indication of nitrates
Angina
The sublingual nitroglycerin is the drug of choice for acute anginal episodes. The dosing consists of 0.4 mg every five minutes, and a maximum of three doses can be given to the patient. In case of heart pain, the self-administration of the nitroglycerin is recommended, but an EMS needs to be called if the pain does not subside after a single dose. The drug is also used as a prophylactic therapy for patients before they undertake a manoeuvre which may precipitate angina (though the evidence for this is varying). The patients who are not cured after the three doses are the potential candidates for the intravenous nitroglycerin.
The intravenous nitroglycerin is given at a starting infusion rate of 5-10 µg/min. The main aim is to make the patient relieved of the symptoms of angina pain. Caution needs to be exercised that the systolic blood pressure does not fall more than 90 mmHg. After 48 hours of treatment, the nitroglycerin can be switched to the oral and topical form of therapy.
Acute coronary syndrome (unstable angina)
Similar to that described in angina, the sublingual nitroglycerin, followed by intravenous nitroglycerin (in a patient not cured initially), is given. The cornerstone lies in giving the regimen of beta blocker, nitrates and anti-thrombotic and antiplatelet regimen (after assessing the cause). The nitrate also helps in reducing the coronary vasospasm.
Chronic stable angina
The difference between the nitroglycerin and isosorbide dinitrate in the pharmacokinetic parameter is that the nitroglycerin has a shorter onset of action (2-3 min), compared to the isosorbide dinitrate, with an onset of action of 15-30 min. The duration of action also varies between both the drugs (15-30 min for nitroglycerin and 3-6 hours in the case of isosorbide dinitrate). As a result of this difference, the isosorbide dinitrate is mainly used for the treatment of chronic stable angina.
Acute myocardial infarction
The nitrates do not have any survival benefit in the case of myocardial infarction. The nitrates are almost contraindicated in those cases where the hypotension is present. Also, the beta blocker which has the survival advantage is given preference than nitrates and never the administration of nitrates should preclude the use of the beta blocker. The reperfusion therapyis the main treatment in the case of acute myocardial infarction (this includes direct percutaneous intervention and thrombolytic therapy).
Variant (Prinzmetal angina)
The coronary vasoconstriction is responsible for the ischemic pain in this condition.
The calcium channel blocker has shown to be better efficacious for this condition when compared to the nitrate. The nitrate, when given, is given along with the calcium channel blocker.
Heart failure
The nitrates are not recommended for the treatment of heart failure with preserved ejection fraction.
In fact, in a recent trial consisting of 110 patients, where the effect of isosorbide mononitrate was compared to that of a placebo, it was found that the use of isosorbide mononitrate decreases the daily activity level of the patient with preserved ejection fraction heart failure.
The main indication for the use of nitrate is for the treatment of acute decompensated heart failure, especially with an increase in blood pressure.
Acute decompensated heart failure (ADHF)
The initial therapy for an acute decompensated heart failure consists of ventilation (for respiratory distress) and loop diuretic (for fluid overload). The nitrates are especially indicated in patients with heart failure and elevated pressure. The dose of the intravenous nitroglycerin in ADHF includes a starting dose of 5 to 10 µg/min, with increment in the dose made every 5 minutes, at a rate of 5 µg/min.
The nitroprusside needs continuous haemodynamic monitoring in the form of an intra-arterial catheter, as it is more potent. The isosorbide dinitrate though can also be used for the treatment of this condition, but it is not preferred as it has a long half-life (it will be difficult to correct when hypotension occurs in the treatment).
Different Preparation and their Usefulness in the Treatment of Angina and Heart Failure
The transdermal patch of nitroglycerin gained popularity mainly because of the ease of the administration. They consist of a semipermeable membrane separating the reservoir of drug and the skin.
Adverse and Side Effects Related to Nitrates
As the nitrates cause systemic vasodilation, one of the expected side effects is hypotension. This can be corrected by volume infusion.
In addition, the patient experiences a headache and tachycardia (an increase in the heart rate, which occurs as a compensatory mechanism when the decrease in the blood pressure occurs) and flushing.
The nitrates, when infused for a longer period, can cause methemoglobinemia. In this condition, the methemoglobin form of hemoglobin occurs in the red blood cells.
The methemoglobin contains the ferric ion in the core and has decreased affinity to attach to the oxygen. The nitrate causes oxidation of the ferrous ion to ferric ions. At the same time, it hinders the release of the oxygen from other ferrous ions. Thus, the ability to attach, as well as release, is impaired, causing the oxygen-hemoglobin dissociation curve shifts to the left.
The tissue undergoes hypoxia and the blood colour changes to a blush colour. The treatment for this condition is intravenous methylene blue. It hastens the conversion of the methemoglobin to hemoglobin.
Contraindication of Nitroglycerin
The patient is already in hypotension, characterized by the systolic blood pressure less than 90 mmHg. The administration of nitrates might further aggravate the hypotension. The patient has an increased risk of decompensation, as noted by the occurrence of the bradycardia or tachycardia.
The patient has taken drugs for erectile dysfunction like Sildenafil, Tadalafil, and Vardenafil. These are phosphodiesterase 5 inhibitor and its mechanism of action also consists of increasing the concentration of CGMP by preventing the breakdown of CGMP, thereby causing the dilation of the blood vessel. So, a cumulative hypotension, which can be life-threatening, can occur.
There is already compromised output from the heart, in a disease like hypertrophic cardiomyopathy and severe aortic stenosis. The administration of nitrates in these patients leads to a compromised ejection fraction of the heart. In those patients, who have a massive right ventricular infarction, the risk of hypertension increases with nitrates.
The nitroprusside has the risk of causing cyanide toxicity. The nitroprusside normally gets metabolized into cyanide and the cyanide is detoxified by the conversion into thiocyanate, which occurs in the liver and kidney. In patients who are on long-term treatment with nitroprusside, run the risk of accumulation of cyanide in the blood.
Nitrate Tolerance
The tolerance of the nitrate is the loss of the therapeutic benefit of a decrease in blood pressure after the drug administration. This occurs in many patients after 24 hours of therapy.
The mechanism behind the nitrate tolerance can be divided into early and late causes. The compensatory neuro-hormonal activation of the body is the initial mechanism for the loss of effect seen with nitrates. In the long term, the decrease in the biotransformation of the nitrates by the inhibition of the ALDH-2 is a proposed reason.
The inhibition of this enzyme is caused by the stimulation of the vascular superoxide and the peroxynitrite formation by the nitrates. One of the other reasons proposed is the nitrate-induced endothelial dysfunction, which occurs in the treatment.
As intravenous nitroglycerin forms a part of initial emergency therapy in angina and is not given in the long term, the tolerance can be overlooked in many cases. But, in the case of isosorbide dinitrate and isosorbide mononitrate, which is given long-term for the treatment of chronic stable angina, the tolerance is an important concern. The nitrate-free interval in between the treatment with nitrates is one of the proposed solutions to the problem. However, it increases the risk of rebound angina.
Newer Drug for Angina and Heart Failure
Pentaerythrityl tetranitrate is a drug which is mainly investigated for its proposed absence of the development of nitrate tolerance. But the recent randomized, multicentre trial, which compared the Pentaerythrityl tetranitrate against a placebo in patients with chronic stable angina, the drug was no more effective when compared to a placebo.
References

Comentários
Enviar um comentário