Respiratory Failure: Hypoxemia, Hypercapnia and Hypoxia
Table of Contents
Image: “Cyanosis of the hand in someone with low oxygen saturations.” by James Heilman. License: CC BY-SA 3.0
Partial Pressure of Gases
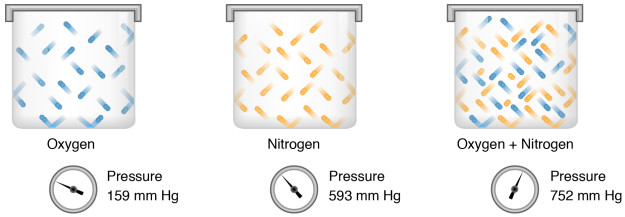
Atmospheric dry air is a mixture of many gases. At sea level, this air has a pressure of 760 mm Hg. The partial pressure that each gas contributes to this atmospheric pressure is based on the percentage of gas in the air.
Pgas = Fgas x Patm
Pgas = Partial pressure of gas
Fgas = Fraction of gas in air
Patm = Atmospheric pressure
Taking the above formula, the PO2 will be:
PO2 = 0.21 x 760 mm Hg
PO2= 160 mm Hg
PCO2 is very low in the atmospheric dry air, and hence, is considered to have a partial pressure of 0 mm Hg. As the air is inspired, it is warmed to 37°C and completely humidified. The gases in the air have a slightly lower partial pressure, owing to the addition of water vapors. This air has not yet participated in gas exchange. In the alveoli, where gas exchange occurs, PO2 decreases and PCO2 increases considerably.
In a normal healthy system, PO2 and PCO2 of the alveolar and pulmonary capillary compartments are the same. As some of the blood shunts through the lungs, the PO2 of the systemic arterial blood is slightly lower than that of the pulmonary capillaries.
Alveolar-Arterial Gradient
The difference between PO2 of alveoli and PO2 of arterial blood is referred to as alveolar-arterial gradient (A-a gradient).
A-a gradient = PAO2 – PaO2
PAO2 = Alveolar PO2 (calculated from the alveolar gas equation)
PaO2 = Arterial PO2 (measured in arterial blood)
In a normal healthy non-smoker’s system, A-a gradient is 5–10 mm Hg.
Alveolar Gas Equation
Arterial PO2 (PaO2) is measured from an arterial blood sample. Unlike PaO2, alveolar PO2(PAO2) cannot be measured directly by taking an air sample from alveoli. Instead, an equation is used to estimate PAO2.
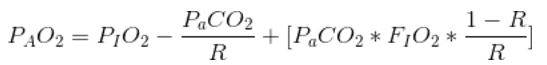
PAO2 = Alveolar partial pressure of oxygen
PIO2 = Partial pressure of inspired oxygen
PaCO2 = Arterial partial pressure of carbon dioxide
FIO2 = Fraction of inspired gas that is oxygen
R = Respiratory exchange ratio
The above equation can be simplified when FIO2 < 1
Alveolar PCO2
Alveolar PCO2 depends on two factors:
- Alveolar ventilation
- Metabolic rate
Alveolar ventilation has an inverse relationship with PACO2.
- Hyperventilation decreases PACO2 as deoxygenated air clears away faster. If ventilation is doubled, PACO2 halves.
- Hypoventilation increases PACO2 as deoxygenated air remains in alveoli for a longer time. If ventilation is halved, PACO2 doubles.
Metabolic rate has a direct relationship with PACO2.
- Increased metabolic rate increases PACO2.
- Decreased metabolic rate decreases PACO2.
The body compensates for these changes in PACO2 by altering alveolar ventilation. In other words, to keep PACO2 constant, the body matches metabolic rate with equivalent changes in alveolar ventilation. For example, during exercise (increased metabolism), the respiratory rate also increases to expel the increased PACO2.
Alveolar PO2
Alveolar PO2 (PAO2) depends on PACO2, and therefore, on alveolar ventilation.
- Hyperventilation decreases PACO2, leaving more space for oxygen (increased PAO2).
- Hypoventilation increases PACO2, decreasing space for oxygen (increased PAO2).
Arterial-Venous Gradient
The difference between PO2 of arterial blood and PO2 of venous blood is referred to as arterial-venous gradient (a-v gradient). The arterial-venous gradient is highly dependent on the rate of metabolism. At higher metabolic rates, more O22 is produced. Hence, the a-v gradient is high during exercise and in trained athletes.
“Overview Arterial-venous and Alveolar-arterial Oxygen Gradients” Image created by Lecturio
Tissue Hypoxia — Deprivation of Oxygen Supply
Hypoxia is a state of body or a region of the body when it is deprived of adequate oxygen supply. It results from the failure of oxygen delivery to cells.
Etiology of Hypoxia
Tissue hypoxia has many diverse reasons. The mechanisms behind these causes can be summarized as follows:
- General ischemia
- Localized ischemia
- Anemia
- Carbon monoxide poisoning
- Hypoxemia
Generalized ischemia results from a low cardiac output. Many heart diseases could contribute towards it. Localized ischemia, on the other hand, is caused by vascular dysfunction, as in cases of peripheral vascular disease and gangrenes.
Image: “Cyanosis of the hand in someone with low oxygen saturations.” by James Heilman. License: CC BY-SA 3.0
Anemia decreases the capacity of blood to carry oxygen as lesser hemoglobin is available to bind to oxygen. This leads to a decreased supply of oxygen throughout the body.
Carbon monoxide binds to hemoglobin and keeps it from carrying oxygen. The binding of carbon monoxide to hemoglobin is 100 times stronger than that of oxygen to hemoglobin. Additionally, it keeps the already bound oxygen from releasing at tissues.
Hypoxemia refers to a decreased oxygen level in the blood (specifically arterial blood), as opposed to hypoxia which refers to decreased oxygen level in tissues, organs and/or the body. Hypoxemia would eventually lead to hypoxia, but, as mentioned above, it is only one of the many causes of hypoxia.
Body’s Response to Hypoxia
The body has various compensatory mechanisms set in place to combat hypoxia. The immediate response includes:
- Shifting respiratory reactions from aerobic to anaerobic reactions, leading to lactic acid build-up
- Increasing ventilation in response to lower PO2
- Systemic vasodilation to improve tissue perfusion
- Pulmonary vasoconstriction to shunt blood towards better-ventilated regions
If hypoxia remains for a longer duration (over 2 weeks), interstitial cells in the peritubular capillary bed of the renal cortex secrete erythropoietin. Erythropoietin will primarily target erythrocyte progenitors to induce the production of red blood cells. This improves the oxygen supply. Therefore, erythrocytosis is considered to be an important clinical sign of chronic hypoxia.
Hypoxemia — Decreased Blood Oxygen
Air is inhaled into the alveoli where oxygen diffuses into the blood through the walls of the alveoli and capillaries. Hypoxemia, i.e. decreased oxygen in the blood, occurs due to a dysfunction at any stage in this process.
“Hypoxemia. Low Arterial Partial Pressure of O2” Image created by Lecturio
Hypoventilation or Low PIO2
The very first stage of respiration is inhaling an adequate amount of oxygen.
- In hypobaric conditions, the atmospheric pressure of air is lower, and hence, the constituent gases, including oxygen, have a lower partial pressure.
- In closed compartments, oxygen is limited. Over time, its consumption can lead to decreased FIO2.
- Hypoventilation causes decreased PAO2.
Diffusional Impairment
The exchange of gases (O2 & CO2) between the alveoli and blood occurs by simple diffusion.
- Thicker alveolar or capillary wall impairs diffusion of gases.
- Pulmonary fibrosis thickens the walls of the lungs. Fluid in the lungs can decrease the diffusion capacity.
- The measurement of the uptake of CO in mL/min/mm Hg is called the diffusing capacity of the lung (DLCO).
Right-to-left Shunt
Some pathological shunts can skip the pulmonary circulation.
- Cardiac defects allow the mixing of deoxygenated blood with oxygenated blood.
- Uncorrected left-to-right shunts can progress to the right-to-left shunt. This phenomenon is known as Eisenmenger syndrome.
V/Q Inequality
The gas exchange across the alveolar-capillary barrier could either be diffusion-limited or perfusion-limited. The diffusion-limited gas exchange occurs when net diffusion into pulmonary capillary depends on a magnitude of A-a gradient. If the gradient is high, more oxygen will diffuse. The perfusion-limited gas exchange occurs when the gas exchange is limited by blood flow through pulmonary capillaries. People with heart diseases (reduced cardiac output) experience a perfusion-limited gas exchange.
Ideally, the ventilation-perfusion ratio (V/Q) should be 1. Physiologically, the apex of a lung is poorly perfused (decreased blood flow) and highly ventilated. The V/Q ratio is high and signifies that oxygen does not get a chance to properly diffuse from alveoli to blood. In contrast, the base of a lung is highly perfused (increased blood flow) and normally ventilated. The V/Q ratio is low and signifies that enough oxygen is not available to properly oxygenate the blood.
Hypercapnia — Increased Carbon Dioxide in Blood
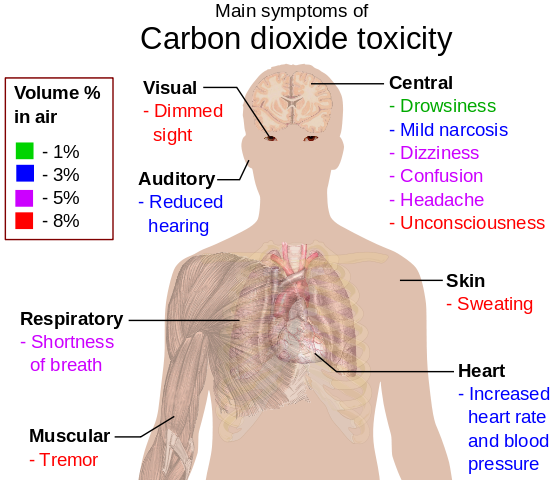
Image: “Main Symptoms of Carbon Dioxide Toxicity” by Mikael Häggström. License: Public Domain
Hypercapnia refers to an increased carbon dioxide level in the blood. Hypercapnia occurs when enough carbon dioxide is not being expelled from the body.
- PaCO2 directly depends on PACO2. Expulsion of CO2 in the alveoli is important to maintain a concentration gradient between alveoli and blood and facilitate the diffusion of CO2 across the alveolar-capillary barrier.
- Poor ventilation decreases the V/Q ratio, stopping the adequate off-loading of CO2 from erythrocytes.
- A higher metabolism produces more CO2. Without proper reflex, this can lead to hypercapnia.
Review Questions
Solutions can be found below the references.
1. Analysis of expiratory gases of a patient reveals the following information. What is the explanation of such findings in the patient?
- Normal alveolar ventilation and perfusion
- Poor alveolar ventilation
- Poor alveolar perfusion
- Right-to-left shunt
2. A patient has the following arterial blood findings. Which of the following is the most likely cause of these findings?
- Obesity
- Carbon monoxide poisoning
- High altitude
- Asthma
- Anemia


Comentários
Enviar um comentário