Laboratory Evaluation in Rheumatic Diseases: Acute-phase Protein and Autoantibodies
Table of Contents
Overview
There more than 100 rheumatic diseases that are characterized by
inflammation against supportive and connective tissues of the body such
as joints, bones and muscles. They arise from the body mounting an
immune response against harmless antigens that are located in the body
due to cross reactivity of these antigens with harmful antigens.
Autoantibodies, when detected, can confirm the preliminary diagnosis of
autoimmune diseases, and identify disease activity. Unfortunately, the
detection of these autoantibodies in a healthy individual is common, and
their absence in a patient with a suspected rheumatic disease does not
exclude the diagnosis.
Thus, there is no specific diagnostic test for most of the rheumatic diseases and correlation of various findings is applied.
Acute Phase Proteins
Rheumatic diseases are characterized by chronic inflammation.
Inflammation is associated with an increase in the levels of:
- Ceruloplasmin
- Erythrocyte sedimentation rate
- C-reactive protein
- Ferritin
- Haptoglobin
- Fibrinogen
- Alpha-1 antitrypsin and amyloid A.
Ceruloplasmin, C-reactive protein, ferritin, haptoglobin, fibrinogen,
and amyloid A are known as acute phase proteins, and an elevation in
any of them is indicative of inflammation. Acute phase reactants might
be also elevated in infections and malignancy. The most commonly used
acute phase proteins/reactants are the erythrocyte sedimentation rate
and the C-reactive protein.
An elevated erythrocyte sedimentation rate equals and elevation of
fibrinogen because red blood cell aggregation is mainly affected by
fibrinogen. Therefore, the erythrocyte sedimentation rate can be
considered as an indirect assessment of the acute phase protein,
fibrinogen.
ESR
ESR represents the rate at which red blood cells settle. It is
directly proportional to age and thus normal levels vary as follows :
The normal erythrocyte sedimentation rate (ESR) can be estimated using the following formulas in males and females:
- ESR in males = age / 2
- ESR in females = (age + 10) / 2
The C-reactive protein is another acute phase protein that is
elevated in case of inflammation. The serum levels of C-reactive protein
might be elevated up to 1000 times when the patient develops an
inflammatory condition. The C-reactive protein is synthesized in the
liver. The C-reactive protein levels are not dependent on the age or sex
of the patient making them a more robust assessment of inflammatory
conditions.
False positives are seen with malignancy, anemia and infective
processes. The test is used to monitor patients with fibromyalgia and
polymyalgia rheumatica.
C-reactive protein (CRP)
The normal C-reactive protein (CRP) levels can be summarized in the following:
- Normal < 0.2 mg/dL
- Indeterminate 0.2 to 1.0 mg/dL
- Inflammation > 1.0 mg/dL
- Infectious etiology > 10 mg/dL
Acute Phase Reactants in Rheumatic Diseases
Rheumatoid Arthritis
In patients with rheumatoid arthritis, the CRP levels are elevated. This is useful in distinguishing patients with rheumatoid arthritis
from those with osteoarthritis. A highly elevated CRP level early in
the disease is indicative of severe progressive erosive rheumatoid
arthritis. CRP levels can be used to monitor disease activity in
rheumatoid arthritis. ESR levels are also elevated in rheumatoid
arthritis, however, the sensitivity of ESR in rheumatoid arthritis is
low compared to CRP.
Ankylosing spondylitis and Psoriatic Arthritis
CRP levels are elevated only in half of the patients with ankylosing
spondylitis. Patients with ankylosing spondylitis and peripheral
arthritis or uveitis have markedly elevated CRP levels. ESR levels are
also elevated in half of the cases, however, the ESR levels in this
group of patients is not correlated with disease severity.
Systemic Lupus Erythematosus
ESR levels are usually elevated in systemic lupus erythematosus,
however, CRP levels are frequently normal. In fact, asymptomatic
elevation in ESR might be the first manifestation of systemic lupus
erythematosus in some patients. An elevated CRP in a patient with
systemic lupus erythematosus is suggestive of early atherosclerosis.
Autoantibodies
Rheumatoid Factor
The rheumatoid factor (RF) is a specific antibody against the Fc section of immunoglobulins.The most common structure of RF is the IgM structure.
A positive RF does not mean that one has rheumatoid arthritis.
However, up to 70% of rheumatoid arthritis patients, have a positive RF
test.The role of RF in the pathogenesis of rheumatoid arthritis is still
poorly understood, however, it is likely to be related to impaired
antigen presentation and an amplified humoral response.
In A positive RF might be indicative of worse prognosis in patients with rheumatoid arthritis.
Positive and elevated RF levels are associated with:
- Aggressive joint disease
- Rheumatoid nodules
- Extra-articular involvement.
In up to 15% of healthy individuals, RF level is positive. Therefore,
the sole presence of RF is not sufficient to make the diagnosis of
rheumatoid arthritis. RF levels are also elevated in patients with
systemic lupus erythematosus, cryoglobulinemia, pulmonary interstitial
fibrosis and silicosis, and in Sjogren’s syndrome. Up to one-third of
the patients with rheumatoid arthritis are seronegative (do not have
RF).
Anti-citrullinated peptide antibodies
The most type of anti-citrullinated peptide antibodies (ACPAs) is the anti-perinuclear factor.
Other common ACPAs include an anti-keratin antibody, anti-fliaggrin,
anti-Sa, and anti-cyclic citrullinated peptide (anti-CCP). Anti-CCP is
highly specific for rheumatoid arthritis compared to other
autoantibodies including RF.
Anti-CCP antibodies are detected years before the development of any
rheumatoid arthritis symptoms. Patients with positive anti-CCP
antibodies early in the disease are more likely to have erosive disease
compared to those who do not. Anti-CCP titrations are not used in
clinical practice because anti-CCP levels are not correlated with
disease activity and are useless in monitoring the disease.
Antibodies Against Nuclear Antigens
Anti-nuclear antibodies
(ANA) include antibodies that act against the DNA, RNA, histones,
centromeres, nucleolus, and other nucleoproteins. The most commonly used
ANAs in clinical practice are those against DNA or RNA.
ANAs include two types of antibodies: antibodies against DNA and
histones, and antibodies against extractable nuclear antigens.
Antibodies against DNA and histones are elevated in systemic lupus
erythematosus and drug-induced lupus erythematosus.
ANA tests are quite specific and sensitive for systemic lupus
erythematosus and scleroderma. In patients with drug induce systemic
lupus erythematosus and mixed connective tissue disease, a positive ANA
is diagnostic.
The other specific ANAs in rheumatic diseases can be summarized in the following:
| Anti-dsDNA | Diagnostic of SLE with a specificity of 97.4% and sensitivity of 57.3% | |
| Anti-Sm | Diagnostic of SLE with a specificity of almost 100% but low sensitivity of 25% | |
| Anti-RNP | Their presence is diagnostic of mixed connective tissue disease | |
| Anti-histone antibodies | They are present in up to 95% of those with drug-induced lupus erythematosus | |
| Anti-chromatin | They are present in 50 to 90% of systemic lupus erythematosus patients | |
| Anti-Ro/SSA and anti-La/SSB | They are found in systemic scleroderma and are diagnostic of the condition. They are also detected in patients with systemic lupus erythematosus | |
| Anti-centromere | Antibodies against the centromere protein B (CENP-B) are found in patients with limited cutaneous systemic sclerosis and in patients with CREST syndrome | |
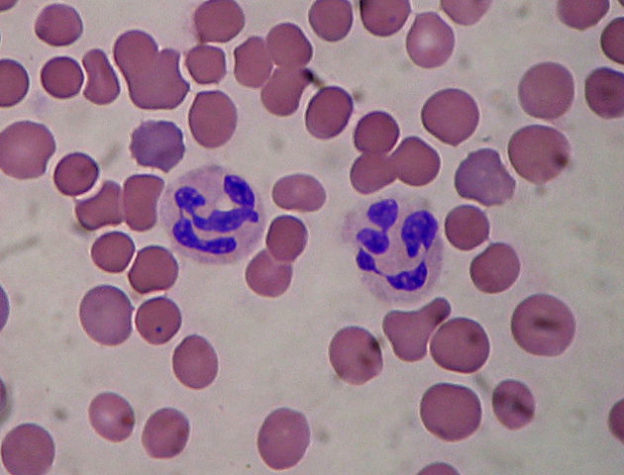
| Anti-neutrophil cytoplasmic antibodies (ANCAS) | Detected in patients with Wegener’s granulomatosis, pauci-immune glomerulonephritis, microscopic polyangiitis, and Churg-Strauss syndrome | |
| Anti-Mi2 antibodies | Detected in patients with dermatomyositis. Anti-SRP antibodies are detected in autoimmune heart disease and myositis. Anti-MAS antibodies are found in rhabdomyolysis |

Comentários
Enviar um comentário