Inflammatory Bowel Disease (IBD) — Types, Causes and Treatment
Inflammatory bowel disease (IBD) is a group of conditions that affect the gastrointestinal system. IBD consists of autoimmune diseases that attack the GI mucosa, resulting in inflammation of the gut wall. For this discussion, we will be focusing on ulcerative colitis (UC) and Crohn’s disease (CD). The main differences between the two are that ulcerative colitis mainly involves the large intestine and rectum while Crohn’s disease can affect the GI system anywhere from the mouth to the anus and usually skips the rectum. Other conditions such as microscopic colitis and Behçet's disease are also types of IBD. IBD is different from irritable bowel syndrome (IBS) which is a functional disorder that is defined as abdominal pain and bowel movement changes.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your gastrointestinal pathology course now for free!
Definition of IBD
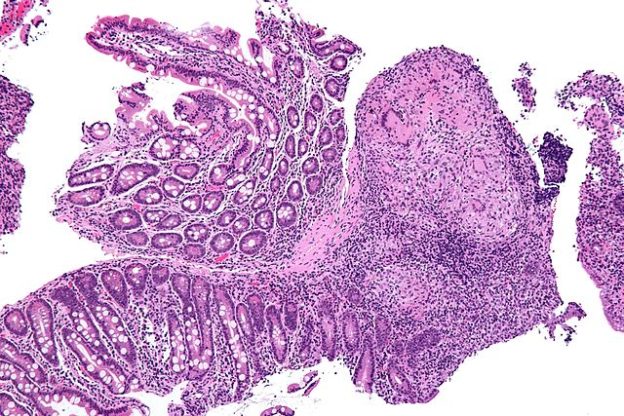
Image: “Micrograph showing inflammation of the large bowel in a case of inflammatory bowel disease. Colonic biopsy. H&E stain.” by Nephron. License: CC BY-SA 3.0
Inflammatory bowel disease (IBD) describes several autoimmune diseases involving inflammation of the bowel wall. Ulcerative colitis is usually isolated to the large intestine and rectum while Crohn’s disease may involve any portion of the gut tube, from mouth to anus. There are extraintestinal symptoms as well that range from connective tissue pathology to biliary disease.
Epidemiology of IBD
Spread of inflammatory bowel disease
The incidence of IBD is about equal in all races and both sexes. The age distribution is bimodal with one peak between 15–40 years old and one smaller peak between 55–65 years. There are higher incidents of the disease in developed countries and in countries further from the equator.
Etiology of IBD
Causes of inflammatory bowel disease
As with all autoimmune diseases both genetic and environmental triggers work together to sensitize the immune system. There is about a 10 fold increased risk in developing IBD if a first degree relative has the condition. Also, animal protein and recent antibiotic use increase risk of developing the condition.
While the genetic trigger has not been identified several hundred genes are currently under investigation. These genes regulate cytokines and lymphocyte activation. Genetic influence may protect individuals from one form of IBD and increase risk to another. Additionally, nicotine appears to provide some protection to ulcerative colitis and increase risk for developing Crohn’s disease.
Pathology and Pathophysiology of IBD
The pathophysiology of IBD is currently under investigation. The most prominent theory involves a disruption in the intestinal response to luminal bacteria. Under normal circumstances intestinal mucosa is covered by a protective layer of mucin that inhibits bacterial colonization. Additionally, a large portion of the innate and adaptive immune system is involved in monitoring the GI tract and its contents through gut-associated lymphoid tissue (GALT) and microfold cells (M cells). These systems react to luminal pathogens and stimulate the adaptive immune system to secrete IgA antibodies.
Patients with IBD may have a deficiency in one of these protective mechanisms. The immune system of the large and small intestines abnormally react to gut bacteria resulting in inflammation. A reduced IL-10 response may also play a role. A dysregulation in Th-1 cell (helper T cell type 1) activation is associated with Crohn’s disease while a dysregulation in Th-2 cells is associated with ulcerative colitis.
Note:
- Crohn’s Disease can affect the gastrointestinal tract anywhere from the mouth to the anus. Inflammation is transluminal which may spur the formation of fistulas and strictures. Rectal sparing is common but involvement of the anus is also common.
- The inflammation of ulcerative colitis starts at the rectum and moves proximally in an uninterrupted fashion. It rarely involves the terminal ileum.
Symptoms of IBD
Signs of inflammatory bowel disease
Both Crohn’s disease and ulcerative colitis present with abdominal pain and chronic diarrhea. Weight loss, malaise, and low-grade fever are also frequently seen. Bloody stools and tenesmus are more common in ulcerative colitis because of the involvement of the colon and rectum. Weight loss is more common in Crohn’s disease.
Many signs and symptoms of ulcerative colitis and Crohn’s disease follow recognizable patterns.
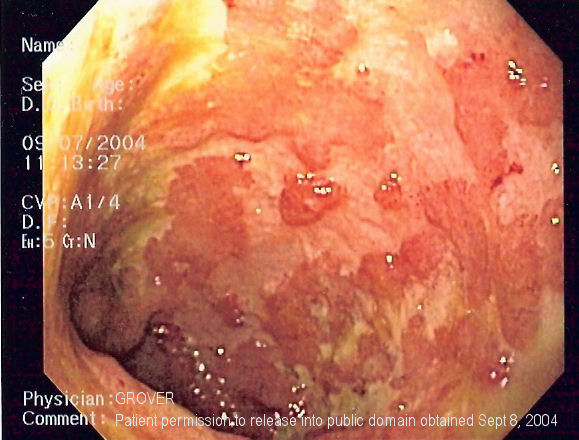
Image: “Endoscopic image of ulcerative colitis affecting the left side of colon. Note that the classic features of ulcerative colitis are not seen here, and that the image resembles Crohn’s colitis as it shows serpigious ulcers. The purpose of this image is to show the difficulty in differentiating between the two disorders on endoscopy.” by Samir. License: CC BY-SA 3.0
| Ulcerative colitis (UC) | Crohn’s disease (CD) | |
| Anus involvement | Rare | Common (perianal fistulas) |
| Rectum involvement | Always | Rare |
| Colon involvement | Always | Common |
| Small intestine involvement | Rare | Terminal ileum is commonly affected |
| Distribution | Continuous | Patchy (skip lesion) |
| Mural thickness | Shallow involvement | Transmural involvement |
| Granulomas on biopsy | None | Present |
| Extra-intestinal Complications | Primary sclerosing cholangitis Pyoderma gangrenosum | Erythema nodosum Apthous stomatitis Arthritis |
Diagnosis of IBD
A battery of tests are recommended when IBD is suspected. A diagnosis is made after the evaluation of several testing methods. Endoscopy is the most definitive tool in this process.
Laboratory
A great deal of information can be gathered from blood test. A CBC is useful to evaluate anemia, a major concern in IBD. Additionally, a thorough nutritional evaluation should be completed, especially iron studies, folate, and B12, and fat soluble vitamins. ESR and CRP markers become elevated in the presence of an inflammatory event. Though they are not specific for IBD both can be used to monitor the condition. Every patient should also have a thorough stool analysis for infection by pathogenic bacteria such as Clostridium difficile or parasites.
Radiography
An abnormal abdominal x-ray may show a variety of intestinal issues. Signs of inflammation include thickened, edematous colonic wall with “thumbprinting” (an x-ray finding of thickened haustra projecting into the lumen of the colon) or air in the colonic wall, AKA pneumatosis coli. Colon enlargement greater than 6 cm is a sign of megacolon. This is seen in ulcerative colitis and is a surgical emergency.
The utility of an abdominal x-ray is greatly enhanced with contrast, especially the double contrast enema (air is a negative contrast while the barium is the positive contrast). A lead-pipe sign implies a loss of haustra and is an indication of chronic ulcerative colitis. A normal rectum in the presence of inflammatory bowel disease implies Crohn’s disease. String sign, a heavily scarred and stenosed portion in the terminal ileum and cobblestoning suggests Crohn’s disease.
Endoscopy
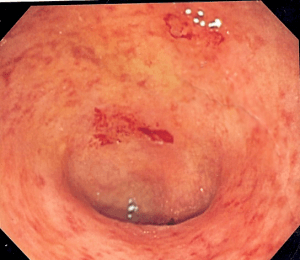
Image: “Endoscopic image of ulcerative colitis showing loss of vascular pattern of the sigmoid colon, granularity and some friability of the mucosa.” by Samir. License: CC BY-SA 3.0
Colonoscopy is useful to evaluate the mucosa directly for inflammation and strictures. The rectum is almost always spared and will appear grossly normal in Crohn’s disease. Biopsies can also be gathered via colonoscopy.
Esophagogastroduodenoscopy is only useful in evaluation lesions and aphthous ulceration in Crohn’s disease. Capsule enteroscopy is reserved for cases where standard colonoscopy and endoscopy do not provide results. Crohn’s disease may demonstrate longitudinal deep ulcers and skip ulcers, inflamed mucosa separated by normal mucosa. In advanced stages of the disease, these ulcers may appear as cobblestones.
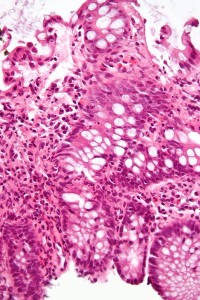
Histology
The mucosa and submucosa of the colon and rectum are both involved in ulcerative colitis. Neutrophil infiltration and crypt distortion is common. Granulomas are not found in ulcerative colitis. About 50 % of Crohn’s disease biopsies will demonstrate granulomas. Inflammation extends throughout the entire wall and proliferation of the muscularis mucosa is frequently observed.
Many diseases besides Crohn’s disease produce non-caseating granulomas including sarcoidosis and leprosy; therefore, this histological finding is insufficient to diagnose Crohn’s disease. These hard tubercles contain giant cells epithelioid histiocytes without necrosis. Caseating (“turning into cheese”) appear with necrotic tissue at their center.
Differential Diagnoses of IBD
Clinical pictures similar to inflammatory bowel disease
- Irritable bowel syndrome: Do not confuse inflammatory bowel syndrome with irritable bowel syndrome (IBS). IBS usually meets three criteria: abdominal pain, changes in bowel habit (diarrhea to constipation and back), without an underlying cause. At this time IBS is considered a functional GI disorder with a strong psychological component.
- Giardiasis: Symptoms include abdominal pain and non-bloody diarrhea
- Intestinal radiation injury
Therapy of IBD
Treatment of inflammatory bowel disease
Maintaining proper nutrition is an important part of IBD treatment, and they may provide some therapeutic effect. Deficiencies in fat soluble vitamins (A, D, E, K), B12, essential fatty acids, and minerals are common. Low residue diets (low fiber) may provide therapeutic benefit.
There are two goals of therapy: remission and maintenance. It is a stepwise process.
Step 1: Amiosalicylates: These drugs provide topical relief to the mucosa and are primarily used in ulcerative colitis. They are affective for inducing remission and maintenance.
Step 2: Corticosteroids: Steroids are ideal for flare-up treatment. They are not intended for prolonged use.
Step 3: Immunomodulators: These drugs act as immunosuppressants by lowering the WBC or bind TNF-α. They take several months to achieve full effect and are reserved for maintenance therapy.
Surgery is also an option in ulcerative colitis only. Proctocolectomy, removal of the colon and rectum can surgically cure the disease; however, ulcerative colitis can also affect the distal ileum. It is usually reserved for complicated cases or malignancy.
Crohn’s disease can affect any part of the gastrointestinal tract form mouth to anus and is not curative. Surgery in this condition is reserved for complications of fistula, stricture or obstruction. Inflammation often reappears at the site of anastomosis. Short gut syndrome is a complication of excess small bowel resections.
Progression and Prognosis of IBD
Patients with ulcerative colitis have the same mortality ratio compared to the general population while those with Crohn’s disease have a slightly higher mortality ratio. IBD increase the risk of developing malignancy of the gastrointestinal system, especially in ulcerative colitis.
Review Questions
The correct answers can be found below the references.
1. A 25 year old female with a history of IBD presents to the ED with severe abdominal pain and diarrhea. Colonoscopy reveals friable, inflamed colonic mucosa. What treatment will you provide in the ED?
- Aminosalicylates
- Steroid therapy
- Infliximab
- loperamine
2. Non-caseating granulomas can be found in Crohn’s disease and what other disease process?
- Fungal infection
- Tuberculosis
- Syphilis
- Sarcoidosis
3. A 35 year old female presents to your GI clinic with adnominal pain and chronic diarrhea. She describes the diarrhea as mucousy, non-bloody, and foul smelling. She recently went on a backpacking trip through Appalachian Mountains in the United States and her symptoms started on the last day on the trail. The likely diagnosis is:
- Giardia infection
- Irritable bowel syndrome
- Inflammatory bowel disease
- Lactose intolerance

Comentários
Enviar um comentário