Interstitial Nephritis (Tubolainterstitial Nephritis) — Pathophysiology and Laboratory Investigations
Table of Contents
- Definition of Interstitial Nephritis
- Epidemiology of Interstitial Nephritis
- Etiology of Interstitial Nephritis
- Pathophysiology of Interstitial Nephritis
- Clinical Presentation and Symptoms of Interstitial Nephritis
- Diagnosis & Laboratory Investigations of Interstitial Nephritis
- Treatment of Interstitial Nephritis
- Prognosis of Interstitial Nephritis
- Review Questions
- References
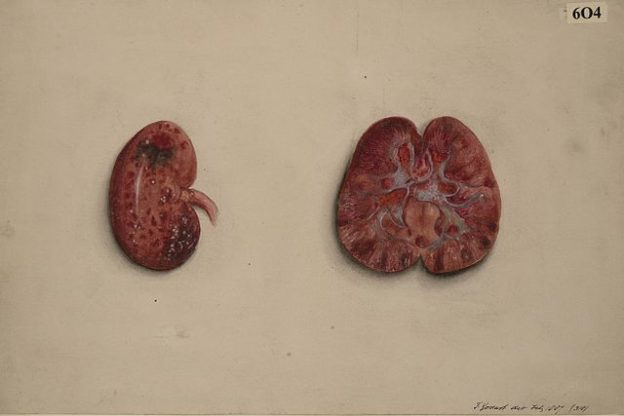
Image : “Kidney in a condition of acute interstitial nephritis” by Godart, Thomas. License: CC BY-SA 4.0
Definition of Interstitial Nephritis
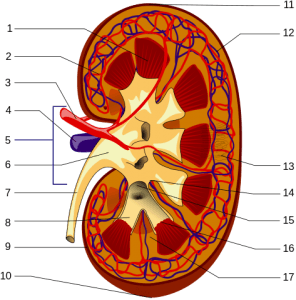
Image: “Structures of the kidney: 1.Renal pyramid 2.Interlobular artery 3.Renal artery 4.Renal vein 5.Renal hilum 6.Renal pelvis 7.Ureter 8.Minor calyx 9.Renal capsule 10.Inferior renal capsule 11.Superior renal capsule 12.Interlobar vein 13.Nephron 14.Minor calyx 15.Major calyx 16.Renal papilla and 17.Renal column” by Piotr Michał Jaworski. License: CC BY-SA 3.0
Interstitial Nephritis as Inflammation
Inflammation of the tubules and interstitium, while sparing the glomerulus, is called as tubulointerstitial nephritis.
Epidemiology of Interstitial Nephritis
Spread of Interstitial Nephritis
Tubulointerstitial nephritis contributes to 10 to 15% of all the kidney diseases in the United States. Women are at greater risk for drug induced interstitial nephritis, when compared to men.
Etiology of Interstitial Nephritis
Acute Interstitial Nephritis
Drugs
- Antibiotics: Sulfonamides, vancomycin, rifampin, beta lactam antibiotics
- NSAIDs
- Diuretics (thiazide and loop diuretics)
- Anticonvulsants (phenytoin, valproic acid and carbamazepine)
Infections
- Bacterial (streptococcal, staphylococcal)
- Viral (EBV, CMV)
Autoimmune Disorders
- Systemic lupus erythematosus
- Sjogren’s Syndrome
Acute Obstructive Disorders
- Light chain nephropathy
- Acute urate nephropathy
Chronic Interstitial Nephritis
- Reflux nephropathy
- Sickle cell disease
- Drugs and toxins
- Phenacetin and NSAIDs
- Cyclosporine and tacrolimus
- Exposure to heavy metals (lead, lithium)
Pathophysiology of Interstitial NephritisType I and type IV hypersensitivity reactions are associated in the pathogenesis of drug induced interstitial nephritis. These drugs act as haptens and, during secretion, they covalently bind to the extracellular components of the tubule. When these haptens are immunogenic, they result in tubulointerstitial injury.Presence of eosinophilia, rash and increased Ig E levels indicate the presence of type I hypersensitivity reaction, while the presence of granulomatous infiltrate in some tissues indicates the presence of type IV hypersensitivity reaction. Dosage of the drugs administered is independent on the incidence of the disease. Discontinuation of the drug results in the reversal of some changes.Clinical Presentation and Symptoms of Interstitial NephritisAcute tubulointerstitial nephritis presents as acute renal failure following the exposure to the offending drug. Nephrotic range proteinuria is seen in patients with NSAIDs induced tubulointerstitial nephritis.Presence of rash, eosinophilia and eosinophiluria should be investigated for the presence of the offending antibiotic, especially in hospital admitted patients for other medical conditions.Clinical onset is more insidious in the chronic tubulointerstitial nephritis. Clinical history includes administration of offending agents for several years. They present with predominant symptoms of tubular dysfunction (polyuria). Proximal tubule defects can present as Fanconi syndrome.Interstitial Nephritis with Uveitis
Image: “Hypopyon – leukocytic exudate in the anterior chamber of the eye.” by EyeMD (Rakesh Ahuja, M.D.). License: CC BY-SA 2.5It is an autoimmune disease seen in around 5% of those affected with tubulointerstitial nephritis. Clinical features include bilateral painful uveitiswith photophobia and blurred vision. Uveitis can either precede or accompany the renal symptoms. Histopathology shows a characteristic lymphocytic infiltrate. Clinical symptoms are usually relapsing in adults and show good response to glucocorticoids.Diagnosis & Laboratory Investigations of Interstitial NephritisBlood and Urine Examination
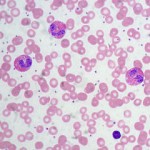
Eosinophiluria is the characteristic finding in acute tubulointerstitial nephritis. Urinanalysismay show proteinuria and microscopic hematuria. The complete blood picture shows the characteristic increase in the number of eosinophils, and further blood examination shows increased blood urea nitrogen and serum creatinine in the presence of renal insufficiency.Gross and Histopathology Findings
Renal biopsy is the definitive test for the diagnosis of acute interstitial nephritis. Findings include:- Cellular infiltration with eosinophils and monocytes
- Sparing of the glomeruli
- Interstitial fibrosis
Chronic tubulointerstitial nephritis shows interstitial fibrosis; tubular atrophy and arteriosclerosis to varying degrees are seen.Radiological Investigations
Papillary calcification with garland pattern appearance on a non-contrast CT scan is characteristically seen in analgesic nephropathy. Ultrasound and CT scan helps in the identifying the presence of chronic kidney disease, but does not help in the diagnosis of tubulointerstitial disorder.Treatment of Interstitial NephritisAcute Interstitial Nephritis
Withdrawal of the offending agent is the primary treatment for acute interstitial nephritis. Treatment with glucocorticoids is recommended in the absence of improvement after the withdrawal of the offending agent.Chronic Interstitial Nephritis
Treatment is usually supportive and is tailored based on the etiology. Offending drugs like analgesics are to be discontinued, immunosuppressive agents like tacrolimus and cyclosporine needs to be replaced. Heavy metal poisonings, like lead, needs to be promptly identified and treated.Prognosis of Interstitial NephritisImprovement is seen as long as the offending agent is removed from the circulation. The majority of the tubule interstitial disorders will progress to end stage renal disease (ESRD). The rate of progression to ESRD is slower when compared to other glomerular disorders.Review QuestionsThe solutions are located below the references.1. A 52-year-old male is presented with fever, flank pain, polyuria and dysuria. After blood and urine tests, tubulointerstitial nephritis is diagnosed by the urologist. The patient history reveals that the patient is taking NSAIDs since 11 months. What is the primary treatment in this case?- Removing the offending drug and glucocorticoid treatment
- Fluoroquinolone
- Ampicillin
- Cephalosporins
- Anti-histamines
2. Which of the following drug is not implicated in tubulointerstitial nephritis?- Diclofenac sodium
- Aspirin
- Ibuprofen
- Furosemide
- Tolterodine
3. Which of the following is the characteristic finding in acute tubulointerstitial nephritis?- Eosinophiluria
- Neutrepenia
- Uricemia
- Albuminuria
- Hyperuricemia

Comentários
Enviar um comentário