Anatomy of the Lower Extremity: Knee Joint
Table of Contents
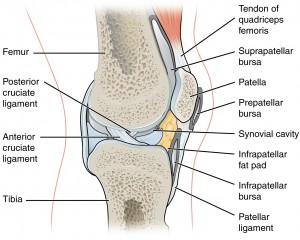
Knee Joint
The knee is a complex joint made up of 3 articulations: the medial and lateral femorotibial joints and the patellofemoral joint. It is not a simple hinge joint because it has 6 degrees of motion: flexion/extension, internal/external rotation, varus/valgus, compression/distraction, and anterior/posterior and medial/lateral translation. The normal range of flexion/extension is 10 degrees extension to 130 degrees flexion.
Image: “Head of the femur” by Henry Vandyke Carter and Henry Gray: “Gray’s Anatomy” (1918), License: Public Domain
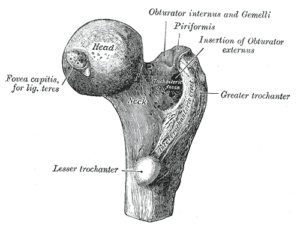
Femur
Medial and lateral condyles form the distal femur. Anteriorly, they are separated by the intercondylar notch. Posteriorly, they are separated by the intercondylar fossa. On the medial epicondyle, the adductor tubercle is the insertion point of the adductor magnus muscle. Both condyles are covered with hyaline articular cartilage. The trochlea is the surface that articulates with the patella.
Tibia
The proximal tibia is made up of the medial and lateral condyle. Gerdy’s tubercle (iliotibial band insertion) is located on the lateral epicondyle. The tibial tuberosity/tubercle is located anteriorly and is the point of insertion for the patellar tendon.
The tibial plateau is the tibial portion of the femorotibial joint. The articular surface is divided into a medial and a lateral facet. The facets have an oval shape. The medial facet is concave in both sagittal and coronal planes. The lateral facet is concave in the coronal plane and convex in the sagittal plane. This is because as the knee flexes, the lateral femoral condyle slides posteriorly on the tibia meaning the tibia externally rotates with knee flexion.
The intercondylar eminence separates the medial and lateral tibial facets. This area is not covered with articular cartilage. And within the eminence are the medial and lateral tibial intercondylar tubercles.
Patella
The patella is the largest sesamoid bone in the body. The proximal base is wider than the distal apex. It serves as a pulley for knee extension by reducing the movement arm – decreasing the force needed for knee extension.
The retro-patellar joint surface articulates with the femur. It is divided into a wide lateral and narrow medial facet. The lateral facet is concave and the medial facet can be both concave and convex.
Joint Capsule of the Knee
The joint capsule of the knee joint is wide and covers all involved osseous structures. It consists of the following layers: synovial membrane and fibrous membrane.
Synovial membrane
The synovial membrane forms many recesses and inserts close to the bone-cartilage border of the femur and forms the suprapatellar recess. Tibial insertion points are located on bone-cartilage-border medially, laterally, and ventrally of the tibial plateau. From the medial and lateral facets, it runs ventrally and revolves the intercondylar area. The cruciate ligaments are located in this region and are covered by the synovial membrane and lie outside the synovium.
Fibrous membrane
In contrast to the very complex course of the synovial membrane, the fibrous membrane inserts in almost all areas of the knee joint. The few exceptions are the tibial plateau, the intercondylar area, and the lateral condyles.
At the tibial plateau, the membrane inserts distally at the edge of the plateau, and the intercondylar area is bridged from the dorsal direction instead of from the ventral. From the insertion line at the lateral condyles, the membrane runs at the outer and superior edges of the bases of the meniscus, and, from the caudal direction, it runs to the outer and lower edges so that the menisci are directly inside of the fibrous membrane.
Parapatellar recess
This recess is very small and is not always present. It is formed between the lateral femoral bone-cartilage border and the lateral surfaces of the patella.
Subpopliteal recess
The subpopliteal bursa communicates with the articular cavity and is, thus, referred to as the subpopliteal recess.
Recessus subtendinea gastrocnemii
The capsular bulging between the heads of the gastrocnemius muscle and the femoral condyles is referred to as recessus subtendinea gastrocnemii or the pole caps.
Suprapatellar recess
The largest recess of the knee joint is formed by the joint capsule that lies ventro-cranially of the patella and contains a superficial and a deep sheet. The deep sheet inserts at the proximal area of the facies patellae and runs cranially to turn back caudally above the base of the patella. Then it is fixed at the base of the patella as the superficial sheet. This recess is located underneath the tendon of the rectus femoris muscle. This means that the two sheets of the recess glide against each other at contraction and stretching of the muscle.
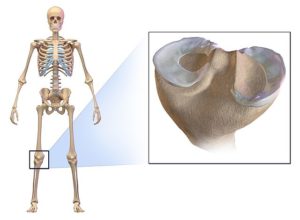
Meniscus
Image: “Meniscus of the knee” by Andrewmeyerson – Own work, License: CC BY-SA 4.0
Histology and vascular supply
Menisci are c-shaped fibrocartilage wedges that are thick on the outside and thin on the inside. Their main purpose is shock absorption. They are made of type I collagenous fibers and some elastic fibers. They consist of three layers where each layer has its own specific structure:
Both the lateral and the medial menisci have their respective anterior and posterior horns, an inner section in the cavum articulare, and a base.
The anterior horns of the menisci are anchored by the patellomeniscal ligaments and are connected to each other by the transversum genu ligament. The inner 2/3 of the menisci are supplied via diffusion of the synovial fluid.
The base of each meniscus is supplied by blood vessels that originate from the fibrous membrane. A special feature of the medial meniscus is that additional vessels radiate into it via the posterior medial collateral ligament. Anterior and posterior horns are vascularized via the meniscotibial ligament.
Ligamentous fixation of the medial meniscus
The medial meniscus is c-shaped and is fixed to the bone by several ligaments. Via the anterior meniscotibial ligament, the anterior horn is connected to the anterior intercondylar area, while the posterior horn is connected to the posterior intercondylar area by the posterior meniscotibial ligament. The posterior medial collateral ligament communicates with the dorsomedial area of the meniscus and the semimembranosus muscle is fixed at the posterior horn of the meniscus.
Ligamentous fixation of the lateral meniscus
The ring-shaped lateral meniscus is fixed at the tibial plateau by the anterior and posterior meniscotibial ligaments. The posterior meniscofemoral ligament runs from the posterior horn of the meniscus to the inside of the medial condyle, parallel to the posterior cruciate ligament. Also, the popliteus muscle is connected to the posterior horn.
Functional anatomy: movement behavior of the menisci
During knee flexion, the menisci are pulled dorsally by the femoral condyles. The semimembranosus muscle (medial) and the popliteus muscle (lateral) synergize this gliding motion with their direct connection.
During extension, the femoral condyles push the menisci ventrally on the tibial plateau. The extent of the movement of the lateral meniscus is significantly greater than that of its medial counterpart.
During rotation, the menisci follow the movement of the femoral condyles. During internal rotation, the medial meniscus moves anteriorly and the lateral meniscus moves posteriorly on the tibia.
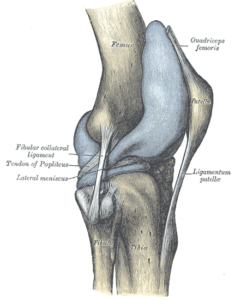
Ligaments of the Knee Joint
Image: “
More details
Capsule of right knee-joint (distended). Lateral aspect.” by Henry Vandyke Carter and Henry Gray: “Gray’s Anatomy” (1918), License: Public Domain
Anterior cruciate ligament
The anterior cruciate ligament (ACL) originates from the dorsal, inner lateral femoral condyle and inserts at the roof of the intercondylar fossa. It has two fiber bundles: the anteromedial and the posterolateral bundle.
The ACL stabilizes the knee joint preventing excess anterior translation of the tibia on the femur. It also limits the extension and rotation of the joint.
Posterior cruciate ligament
The posterior cruciate ligament (PCL) originates from the inner surface of the medial femoral condyle and inserts at the posterior intercondylar area of the tibia. The PCL also has two fiber bundles: the anterolateral and the posteromedial bundle.
The PCL prevents excess posterior translation of the tibia. It also limits the extension and internal rotation of the knee joint.
Lateral/fibular collateral ligament
The lateral/fibular collateral ligament originates from the lateral femoral epicondyle and inserts at the head of the fibula. This ligament stabilizes the knee joint against varus stress.
Medial collateral ligament
The medial/tibial collateral ligament originates from the medial femoral epicondyle and inserts at the medial condyle of the tibia. It stabilizes the knee joint against valgus stress.
Patellar tendon
The patellar tendon runs from the apex of the patella to the tuberosity of the tibia and is the continuation of the quadriceps tendon. Between the ligament, the tibia, and the infrapatellar fat pad is the superficial infrapatellar bursa.
Innervation of the knee joint
Clinical Knee
Cruciate ligament rupture
Cruciate ligament rupture describes the partial or complete rupture of the anterior, posterior, or both cruciate ligaments. Usually from direct trauma to the knee or pivoting/buckling injury to the knee during sports. Results in anterior/posterior translational instability. Surgical reconstruction is the treatment of choice.
Dislocation of the patella
The patellar dislocation can be traumatic or from ligament laxity, and it usually dislocates laterally. Recurrent dislocation can result in patellofemoral arthritis. Common surgical treatments include medial patellofemoral ligament reconstruction and/or tibial tubercle osteotomy.
Image: “A Baker’s cyst (popliteal cyst) is located behind the knee and is a swelling of the popliteal bursa. In this image, the Baker’s cyst is the yellowish tissue and was discovered during routine dissection.” by Dr. Frank Scali – Own work, License: CC BY-SA 3.0
Baker’s cyst
Common cysts which occur in the popliteal area. If the swelling is small, patients hardly have any symptoms. If the accumulation of fluid increases due to continuous incorrect loading, sensitive structures can be compressed and cause pain and/or impairment of movement. Baker’s cyst can be treated conservatively or with surgery. However, it has a high rate of recurrence.
Meniscal injuries
Three forms of meniscus injuries should be distinguished: degeneration, impingement, and tear, whereas all three forms can be caused by each other or may occur in combination
Degeneration
Degeneration of the meniscus or its fibril structure occurs due to incorrect loading and unloading causing pathological changes in vascularization. If the tissue is not sufficiently supplied with blood and nutrients, it decays and cannot regenerate. Degeneration of meniscus tissue due to loss of vascularization is irreversible.
Impingement
If the gliding behavior of the meniscus is impaired or absent, the meniscus is tucked between osseous structures during movements. Extension lock is the most frequent form of meniscus impingement and is most often caused by a rupture of a part of the meniscus.
Tear
There are different forms of tears, which differ in either their direction or in their localization.
Also, there is a special form of meniscus tear termed the bucket-handle tear. Hereby, a longitudinal tear develops, which can expand into the ventral direction. Thus, a hole in the meniscus results. The inner part, the so-called bucket-handle, can dislocate and can additionally be tucked between bones at flexion or extension. If this meniscus injury progresses, removal of the damaged structure is often the only useful procedure and involves surgery (meniscectomy).
Image: “Knee with Osgood-Schlatter, MRI lateral view”, The original uploader was MBq at German Wikipedia – Transferred from de.wikipedia to Commons. License: Copyrighted Free Use
Osgood-Schlatter disease
Osgood-Schlatter-disease or simply Schlatter’s syndrome is aseptic bone necrosis in the area of the tuberosity of the tibia, which often affects male teenagers and children between the ages of 10 and 16. Patients suffer from load-depending pain which is often severe pain, especially during climbing stair or quick and/or torsional movements, which are high functional loads for the knee joint.
Review Questions
The correct answers can be found below the references.
1. Which statement concerning the parapatellar recess is false?
- The parapatellar recess is very small.
- The parapatellar recess can be absent.
- The parapatellar recess can be present more than once.
- The parapatellar recess is formed between the lateral femoral bone-cartilage border and the lateral surfaces of the tibia.
- The parapatellar recess is formed between the lateral femoral bone-cartilage border and the lateral surfaces of the patella.
2. Which statement concerning the movement function of the knee joint is false?
- The knee joint can perform internal and external rotation during maximal extension.
- The knee joint can perform internal and external rotation during maximal flexion.
- The knee joint can perform flexion.
- The knee joint can perform extension.
- Physiologically, the knee joint cannot perform abduction and adduction.
3. Which statement concerning the menisci is correct?
- Menisci are c- or ring-shaped fibrocartilage wedges.
- The anterior horns of the menisci are connected with the tibia by the patellomeniscal ligament.
- The menisci are primarily supplied by blood vessels.
- Histologically, the menisci mainly consist of type II collagenous fibers.
- The semimembranosus muscle is connected to the posterior horn of the lateral meniscus.



Comentários
Enviar um comentário