Infant of a Diabetic Mother — Pathophysiology and Management
Table of Contents
Epidemiology
A significant proportion of pregnant ladies have some form of abnormal glucose homeostasis.
Recent estimates show that up to 10 % of pregnant women have:
- Glucose intolerance
- Gestational diabetes mellitus
- Preexisting diabetes
Approximately 88 % of pregnant women with impaired glucose homeostasis have gestational diabetes mellitus. The remainder of the cases can be attributed to preexisting diabetes. Two-thirds of mothers with preexisting diabetes have type 2 diabetes mellitus, whereas one-third of the cases are due to type 1 diabetes mellitus.
In addition to the increased risk of different specific complications in infants of diabetic mothers, the risk of caesarean delivery is also increased. This can be explained by the increased risk of macrosomia and shoulder dystocia which are more common in infants of diabetic mothers.
Specific Complications to Infants of Diabetic Mothers
The extent and type of complications that an infant of a diabetic mother might develop depend on whether maternal glucose levels were elevated during the first trimester or not. Early maternal hyperglycemia is commonly associated with congenital malformations of the fetus, whereas late maternal hyperglycemia might be associated with fetal macrosomia, polycythemia and cardiomegaly.
Fetal macrosomia
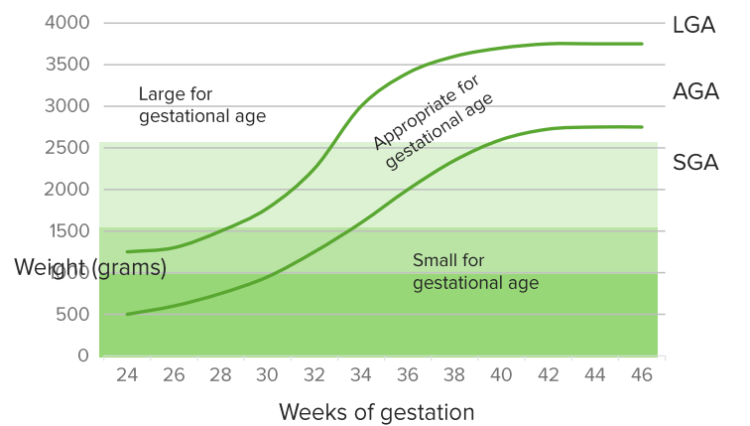
Infants of diabetic mothers are commonly large for gestational age at time of birth, i.e., they have fetal macrosomia. Fetal macrosomia can be accurately defined as a fetal size > 90th percentile for gestational diabetes or > 4000 grams in full-term newborns.
Fetal macrosomia is associated with hypotonia and perhaps an increased risk of shoulder dystocia. They are puffy, fat and ruddy babies. Additionally, fetuses with macrosomia are more likely to be delivered by a caesarean section. Infants who are classified as large for gestational age should be screened for hypoglycemia during the postnatal period.
Respiratory distress and pulmonary disease
Respiratory distress syndrome is more common in infants of diabetic mothers and can be
present within the first hours after birth. Hypoxia can be severe in these infants. Due to the increased risk of polycythemia, infants of diabetic mothers might develop persistent pulmonary hypertension of the newborn. Pneumonia is also more common in this group of infants. They present a few hours after birth with tachypnea, nasal flaring and intercostal recession.
Hypoglycemia and metabolic disturbances
Infants of diabetic mothers who show the following symptoms should be screened for hypoglycemia:
- Irritability
- Poor feeding
- Apathy
- High-pitched or weak cry
Hypoglycemia is due to hyperinsulinemia which is caused by persistent and uncontrolled maternal hyperglycemia. Prolonged maternal hyperglycemia is associated with fetal pancreatic beta cells hyperplasia which can cause hyperinsulinemia in the infant.
Hypoglycemia is due to hyperinsulinemia with low glucose levels. During intrauterine life, maternal glucose passes the blood-placenta barrier while insulin does not cross the blood-placenta barrier; thus the fetus has to produce insulin to control the glucose levels. Prolonged maternal hyperglycemia leads to fetal pancreatic beta cells hyperplasia which can cause hyperinsulinemia in the infant. After birth, maternal glucose is cut off, but the high insulin secretion remains in the newborn which triggers hypoglycemic episodes. The most important risk factors for hypoglycemia in infants of diabetic mothers are preterm labor and for the infant to be classified as large for gestational age.
Electrolyte disturbances
In addition to the metabolic disturbances, infants of diabetic mothers can also develop electrolyte abnormalities such as hypocalcemia and hypomagnesemia. Infants who develop seizures with normal blood glucose have low parathyroid hormone levels after birth.
Additionally, two thirds of infants of diabetic mothers have abnormal iron levels and metabolism at birth. This finding has been associated with impaired neuronal and brain development and can be associated with developmental delay.
Hematologic abnormalities
Infants of diabetic mothers are at an increased risk of fetal hypoxia. Fetal hypoxia can be associated with increased erythropoiesis and polycythemia. Polycythemia puts the infant at an increased risk of stroke, necrotizing enterocolitis, renal vein thrombosis and seizures. Respiratory distress is also more common in infants with polycythemia.
Infants of diabetic mothers are also at an increased risk of bleeding due to thrombocytopenia. Thrombocytopenia is caused by impaired thrombopoiesis, a condition that is commonly seen in infants of diabetic mothers.
Cardiovascular anomalies
Hypertrophic cardiomyopathy is more common in infants of diabetic mothers and can be diagnosed in up to one-third of the infants. Congestive heart failure is also more common in this group of infants and is correlated with the degree of outflow tract obstruction.
Cardiomegaly is also more commonly seen in infants of diabetic mothers. Ventricular septal
defects are way more common in this cohort of infants compared to infants of non-diabetic mothers. Transposition of the great arteries is also more common in infants of diabetic mothers.
Other congenital malformations
Anencephaly is 13 times more common in infants of diabetic mothers compared to infants of non-diabetic mothers. Additionally, the risk of spina bifida and caudal dysplasia is significantly increased in infants of diabetic mothers, 20 times and 600 times, respectively.
The high rate of congenital anomalies is associated with hyperglycemia and rapid growth of the body and other organs. This leads to misalignment of structures leading to development of anomalies, more so congenital heart abnormalities.
The use of insulin by the mother can be associated with neurologic immaturity which can manifest as immature sucking patterns.
Infants of diabetic mothers are also at an increased risk of:
- Hydronephrosis
- Renal agenesis
- Ureteral duplication
- Duodenal atresia
and a myriad of congenital heart defects.
Diagnostic Workup for Infants of Diabetic Mothers
A complete blood count should be performed to diagnose polycythemia. Glucose concentrations should be determined in any infant who develops seizures, and hypoglycemia should be excluded.
Serum levels of magnesium, calcium and iron should be checked in infants of diabetic mothers. Hyperbilirubinemia is commonly seen in infants with polycythemia, and serum total and unconjugated bilirubin levels should be determined in these infants.
Hypoxia should be identified as early as possible by the utilization of peripheral oximeters. Arterial blood gases should be examined to exclude respiratory or metabolic acidosis.
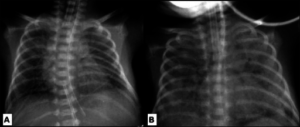
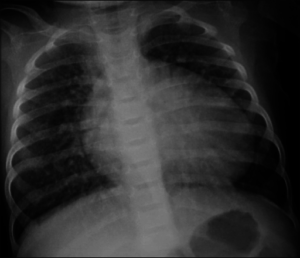
Infants with respiratory distress should undergo a chest x-ray to exclude focal atelectasis, pulmonary edema and free air in the pleural spaces which are findings of respiratory distress syndrome. Cardiomegaly can be also excluded by a chest x-ray.
Infants with caudal dysplasia should undergo pelvic and lower extremity radiographic examination to exclude other musculoskeletal malformations. Infants with hypotension and signs and symptoms suggestive of congestive heart failure should undergo a cardiac echocardiography to exclude hypertrophic cardiomyopathy.
Management of Hypoglycemia and Electrolyte Disturbances in Infants of Diabetic Mothers
Hypoglycemia can be very hazardous to the infant and should be corrected as early as possible. Plasma glucose levels that are below 36 mg/dL but above 25 mg/dL require active intervention only if they remain below this level for a prolonged period, they do not improve with feeding and if the infant is symptomatic. When plasma glucose levels drop below 25 mg, intravenous administration of glucose should be initiated.
The best protocol to correct hypoglycemia is to administer a bolus dose of dextrose solution followed by continuous infusion of dextrose.
Infants with hypocalcemia should be evaluated for the co-presence of hypomagnesemia. The correction of hypocalcemia alone, without correcting hypomagnesemia, usually fails. Therefore, hypocalcemia should be corrected only after the administration of magnesium and after hypomagnesemia is completely corrected.
Infants diagnosed with respiratory distress syndrome might require oxygen supplementation, or intubation and assisted ventilation. Infants who develop apnea should be put on assisted ventilation to avoid prolonged periods of hypoxia which can be associated with permanent neurologic sequalae.
Infants who are diagnosed with hypertrophic cardiomyopathy with severe outflow tract obstruction should receive propranolol. If medical treatment is not sufficient, surgical intervention to relieve outflow tract obstruction might be required.
Finally, infants of diabetic mothers should be always referred to a specialist in neonatal caredue to the increased risk of the various complications we described in this article.
References
European Padiatric Association
http://www.epa-unepsa.org/
International Pediatric Association
https://www.ipa-world.org/
Canadian Pediatric Association
https://www.cps.ca/
American Pregnancy Association
https://americanpregnancy.org/breastfeeding/breastfeeding-while-pregnant/
Academy of Neonatal Nursing
https://www.academyonline.org/default.aspx
American Association of Diabetics Educators
https://www.diabeteseducator.org/
References
WHO recommendation on the diagnosis of gestational diabetes in pregnancy
http://www.epa-unepsa.org/
International Pediatric Association
https://www.ipa-world.org/
Canadian Pediatric Association
https://www.cps.ca/
American Pregnancy Association
https://americanpregnancy.org/breastfeeding/breastfeeding-while-pregnant/
Academy of Neonatal Nursing
https://www.academyonline.org/default.aspx
American Association of Diabetics Educators
https://www.diabeteseducator.org/

Comentários
Enviar um comentário