Chest Pain in Family Medicine
Chest pain is a common and challenging presentation to the outpatient family medicine clinic. When a patient with chest pain is encountered, the main goal of your evaluation is to exclude life-threatening causes. Once life-threatening causes of chest pain are dismissed, the categorization of the patient into cardiac and non-cardiac chest pain is helpful.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your family medicine course now for free!

Overview of Chest Pain
Approximately 2% of outpatient visits are a result of chest pain. Fortunately, most cases of chest pain are found to be non-cardiac in etiology. Because heart disease is the leading cause of death in the United States, the family physician, who is usually the first one to see the patient, should be able to differentiate between cardiac and non-cardiac causes of chest pain.Epidemiology of Chest Pain in the Primary Health Care Versus the Emergency Department
Patients with chest pain often have the common sense to decide whether they are going to their primary health care provider or to the emergency department in a hospital setting. Additionally, the first responders to a patient with chest pain usually know if the patient is unstable. Therefore, they can transfer the patient to an emergency department, if necessary. Accordingly, the epidemiology of the many different causes of chest pain in each healthcare provider setting is expected to be different.Chest pain is a common complaint in the outpatient set up representing up to 1-2 % of outpatient visits. Non-cardiac causes of chest pain are more common but always avoid overlooking the life-threatening causes of chest pain which include myocardial infarction, thrombo-embolism, and pneumonia. The most common cause of chest pain that presents to the primary care is musculoskeletal in origin (up to 36% of the cases). Gastrointestinal diseases, including gastroesophageal reflux disease, are responsible for 19% of the chest pain complaints presenting to the family physician.
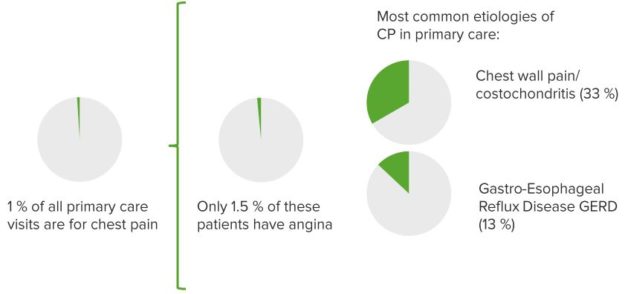
“Etiology Chest Pain” Image created by Lecturio
On the other hand, half of the cases of chest pain presenting to the emergency department are found to be caused by a life-threatening condition that is cardiac in origin. Stable and unstable angina are responsible for 13% each, while chest pain with gastrointestinal origin is rare in patients presenting to the emergency department.
Because of the differences in the etiology of chest pain and the seriousness of the condition, the following recommendations were put by the American Family Physician Society:
| Recommendation | Level of Evidence |
| Determine if the chest pain is anginal or not. | Expert opinion (C) |
| Use the Rouan decision rule to predict patients at high risk of myocardial infarction. | Expert opinion (C) |
| Patients with Wells’ score less than 2 and a normal D-dimer assay do NOT have pulmonary embolism. | Meta-analysis (A) |
| Patients with an abnormal D-dimer test and a Wells’ score of 2 or more should have a helical CT scan plus ultrasound examination of the lower limbs to rule out pulmonary embolism and/or deep venous thrombosis. | Meta-analysis (A) |
| The Diehr diagnostic rules should be used to predict the likelihood of pneumonia. | Meta-analysis (A) |
| Panic disorder should be excluded as a cause of chest pain. | Expert opinion (C) |
| Patients with chest pain should receive an ECG. | Expert opinion (C) |
| Serum troponin-level testing is helpful in excluding myocardial infarction as a cause of atypical chest pain. | Expert opinion (C) |
| Patients with chest pain who have an initial negative ECG should have a repeat stress ECG, a perfusion scan or an angiography based on their risk. | Expert opinion (C) |
| If stress ECG is performed, the Duke treadmill score should be used to predict long-term prognosis. | Meta-analysis (A) |
Clinical Presentation of the Different Causes of Chest Pain
Patients with chest pain due to myocardial infarction might also experience radiation to both arms, hypotension, S3 gallop or diaphoresis. They are unlikely to have pleuritic chest pain or tenderness over the precordium. Patients with pneumonia usually have egophony, dullness to percussion and fever. Bronchial breathing and crackles might be also heard. Patients with heart failure commonly have exertional dyspnea.Because of cardiac enlargement, the heart apical impulse is displaced in most patients. Tenderness to palpation is suggestive of chest pain of musculoskeletal origin or chest wall pain.
Available Scoring Systems for the Family Physician to Rule in or Rule out Certain Diagnoses
To be more objective while examining your patient, it is helpful to have a scoring system that has been research-validated and is evidence-based.Rouan Decision Rule for Myocardial Infarction
This scoring system is based on the clinical presentation of the patient and can be used to predict the risk of myocardial infarction. Patients with a score of 0 have a 0.6% risk of myocardial infarction, those with a score of 1 have a 3.4% risk, those with a score of 2 have a 4.8% risk, those with 3 points have a 12% risk and finally, patients who score 4 points have a 26% risk of myocardial infarction.The following summarizes the Rouan decision rule for myocardial infarction:
- Age > 60 years
- Male gender
- Previous history of myocardial infarction or angina
- Diaphoresis
- Pressure-like chest pain
- Pain radiating to the arm, neck or jaw
Wells’ Scoring System for Pulmonary Embolism
Another life-threatening condition that should be excluded by the family physician is a pulmonary embolism. Wells’-score, combined with laboratory or imaging studies when needed, is usually sufficient to exclude pulmonary embolism.The following table summarizes Wells’ model for clinical diagnosis of pulmonary embolism:
| Clinical Feature | Points | |
| Pain with palpation over the deep leg veins, leg swelling or the presence of other signs and symptoms suggestive of deep venous thrombosis. | 3 | |
| The diagnosis of pulmonary embolism is more likely than any other alternative. | 3 | |
| Heart rate is more than 100 beats per minute. | 1.5 | |
| History of immobilization for three consecutive days or more, or surgery in the past four weeks. | 1.5 | |
| Previous diagnosis of deep venous thrombosis or pulmonary embolism. | 1.5 | |
| Hemoptysis. | 1 | |
| History of malignancy or treatment for malignant disease within the last six months. | 1 | |
| Total Points | Risk of Pulmonary Embolism | Probability of Pulmonary Embolism |
| < 2 | Low | 1 to 28% |
| 2 to 6 | Moderate | 28 to 40% |
| > 6 | High | 38 to 91% |
Diehr Rule for Diagnosing Pneumonia in Adults with Acute Cough
Patients with pneumonia can present with a cough, fever and chest pain. The following scoring system can be used to predict the probability of pneumonia.| Clinical Feature | Points |
| Rhinorrhea | -2 |
| Sore throat | -1 |
| Myalgia | 1 |
| Night sweats | 1 |
| Sputum production | 1 |
| Respiratory rate more than 25 per minute | 2 |
| Temperature more than 100 F or 37.8 C | 2 |
| Total Points | Probability of Pneumonia |
| -3 | 0 |
| -2 | 0.7% |
| -1 | 1.6% |
| 0 | 2.2% |
| 1 | 8.8% |
| 2 | 10.3% |
| 3 | 25% |
| >4 | 29.4% |
Exclusion of Panic Attacks as a Possible Cause of Chest Pain
The patient should be asked the following two questions to exclude panic attacks as a cause of his or her chest pain:1. In the past six months, did you have a spell or an attack where you suddenly felt frightened or anxious?
2. In the past six months, did you have a spell or attack when you suddenly felt like your heart is racing, you fainted or you could not catch your breath?
If the patient answers no to both questions, then he or she is unlikely to have panic attacks as the cause of the current chest pain.
Duke Treadmill Score and Chest Pain
During testing on the treadmill, the following parameters should be considered: duration of exercise, degree of ST deviation in mm and the patient’s angina index. The patient’s angina index can be 0 = no angina during testing, 1 = typical angina during test or 2 = test stopped because of angina. The Duke treadmill score is then calculated with the following equation:
Duke’s Treadmill Score = Exercise time in minutes – (5 x ST deviation in mm) – (4 x angina index)
After the score is calculated, the following table can be used to interpret the results.| Score | Risk of an adverse cardiac event in the future | Seven-year survival rate% | |
| Normal resting ECG | ST or T wave abnormalities on resting ECG. | ||
| > 5 | Low | 95 | 91 |
| -10 to 4 | Moderate | 91 | 80 |
| < -11 | High | 78 | 78 |
Great post.
ResponderEliminarhttps://stocktwits.com/DouglasHunter