Human Digestive System — Processes and Food Resorption in the Small Intestine
Table of Contents
- The Basic Processes of Digestion
- Swallowing as an Aspect of Digestion
- Food Processes in the Stomach
- The Processing of Food in the Duodenum, Plus Pancreas Secretion and Bile
- The Digestion of Food in the Small Intestine
- Phases of Digestion
- Food Resorption in the Small Intestine
- Splanchnic Circulation
- The Processes in the Colon
- Diseases of the Gastrointestinal Tract
- Review Questions
- References
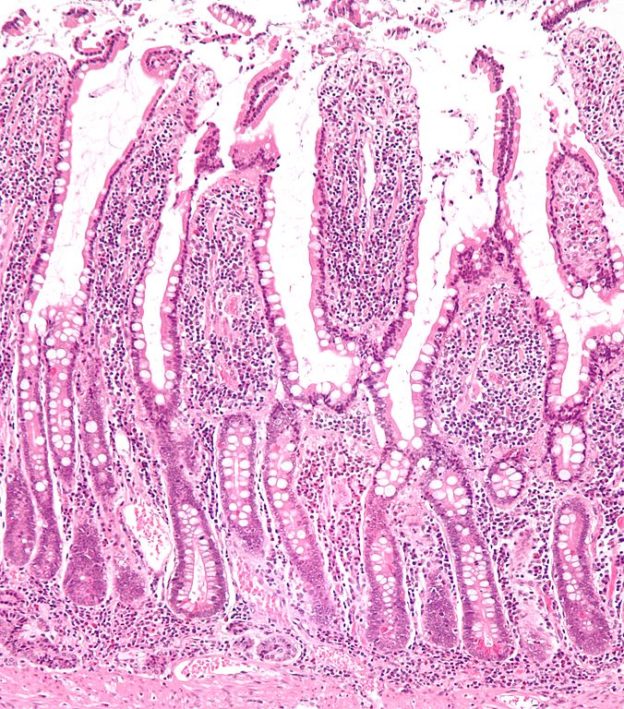
Image: “Low magnification micrograph of small intestinal mucosa. H&E stain.” by Nephron. License: CC BY-SA 3.0
The Basic Processes of Digestion
The digestive system is formed by two groups of organs:
- Gastrointestinal tract (GI tract)
- Accessory (supportive) digestive organs
The GI tract, also known as the alimentary canal, is about 9m long in a cadaver. It is defined as a continuous tube connecting the mouth to the anus.
The constituent elements of the GI tract are:
- Mouth
- Larger part of the pharynx
- Gullet (esophagus)
- Stomach
- Small intestine
- Colon
The accessory digestive organs:
- Teeth
- Tongue
- Salivary glands
- Liver
- Gall bladder
- Pancreas
Other than the teeth, whose purpose is to grind the food, and the tongue, which assists in chewing and swallowing, no other digestive organ ever comes into direct contact with the food. The purpose of the other digestive organs is to generate and store vital secretions that flow through the passages of the GI tract and assist the chemical breakdown of the food.
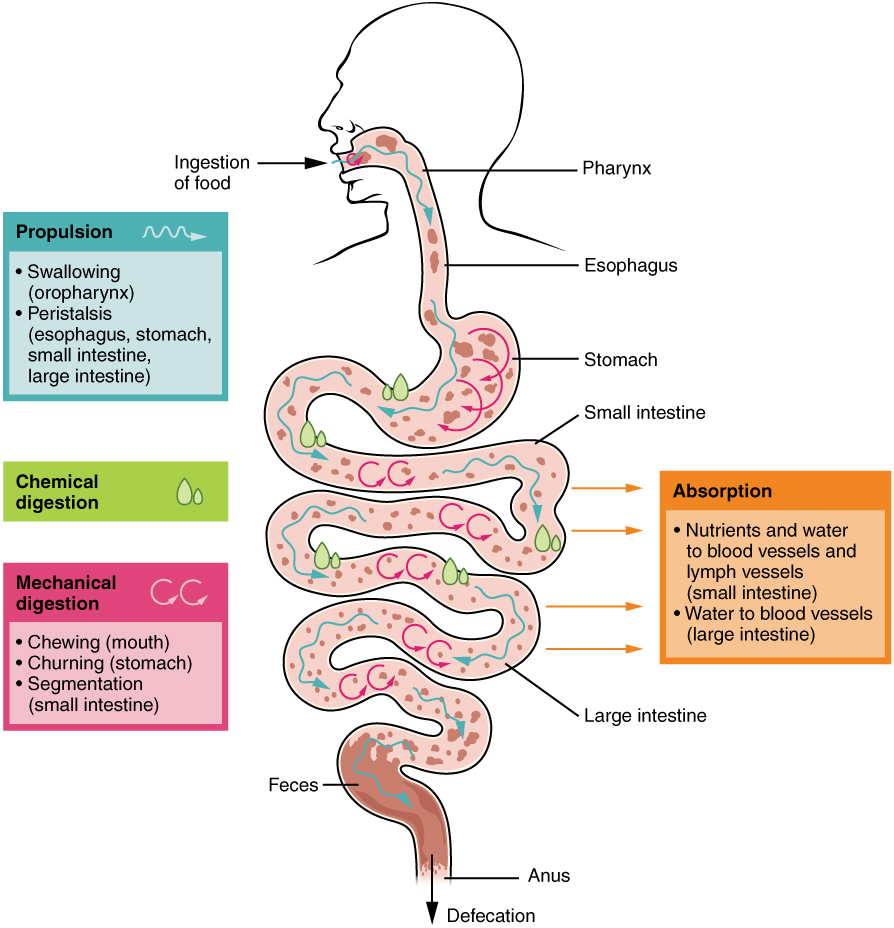
The digestive system performs six important fundamental processes:
Ingestion: Processing of food and the intake of fluid into the mouth. It includes the processes that take place while the food is in the mouth It includes the processes that take place while the food is in the mouth, such as chewing and grinding using the teeth, the lubrication and chemical effects of saliva released from the salivary glands, and swallowing of the food – which sends it on wards down the digestive tract.
Secretion: Seven liters of water, acid, buffers and enzymes are secreted into the lumen of the digestive tract every day.
Mixing and moving: The active movement (motility) of the GI tract, assisted by its alternating contraction and relaxation (peristalsis), enables the food, accompanied by additional secretions, to be propelled towards the anus.
Digestion: During the process of mechanical digestion, the food is ground before being swallowed and churned intensely by the smooth muscles of the stomach and the small intestine. This enables food molecules to be dissolved, and they are mixed with digestive enzymes in the process. During chemical digestion, carbohydrate, lipid, protein and nucleic acid molecules are cloven into smaller molecules by hydrolysis and are afterwards absorbed with the digestive enzymes. Only a few substances, such as vitamins and cholesterol, can be absorbed by the body without chemical digestion.
Resorption/ Assimilation: Resorption (resorbere = absorb) is defined as the entry of digested and secreted fluid, ions and the products of digestion into the epithelial cells that fill the lumen of the GI tract. These substances reach the cells within the entire body via the blood and the lymph. Assimilation is the process by which components/chemicals from food are taken into the cells of the body – after the food/beverage has been digested and absorbed.
Defecation: Defecation is the process, in which waste products, bacteria, indigestible substances or digested materials which have not been absorbed, are excreted via the anus. Material that has been eliminated in the process is defined as feces (a stool).
“GI Overview. How to approach learning the GI System” Image created by Lecturio
The layers and innervation of the GI tract
The wall of the GI tract consists of four layers—each having the same basic layout—going from the lower esophagus to the anus.
Moving from the luminal surface to the outer surface, the following layers are distinguished:
- Mucosa
- Submucosa
- Muscularis
- Serosa
The mucosa, the innermost layer of the the GI tract, is a mucous membrane consisting of an epithelial layer, a layer of connective tissue and a thin layer of smooth muscles.
The epithelium, the most exposed part of the mucosa, has a protective function, and it contributes to secretion and resorption by means of a single-layered columnar epithelium. Exocrine cells are also located among the epithelial cells, and they secrete mucus and fluid into the lumen (lat. = the inside of a cavity) of the GI tract. The epithelium contains the goblet cells which are responsible for the secretion of mucus, which lubricate the passage of food along and protects the intestinal wall from digestive enzymes.
The connective tissue layer or lamina propria (lat. lamina = thin, flat layer; propria = intrinsically) contains many blood and lymph vessels. The lamina propria provides a way for nutrients that have been absorbed into the GI tract to reach other body tissues. In addition, this layer also includes the majority of mucosa-associated lymphoid tissue (MALT) cells, which contain immune system cells and provide protection against disease.
The muscularis mucosae, a thin layer of smooth muscle fibers, increases the surface area for digestion and resorption and ensures that all resorbing cells are exposed to the contents of the GI tract.
The villi, small folds of mucosa found in the small intestine aid the digestive system by increasing the surface area of the intestine. Additionally, the villi contains a lacteal, a vessel like tube connected to the lymph system that helps in the removal of lipids as well as tissue fluids.
The submucosa consists of a network of loose elastic fibers that appear prominent due to the numerous fenestrations (areolar connective tissue). The submucosa links the mucosa to the muscularis. It consists of numerous blood and lymph vessels, which receive the food molecules that are absorbed. The submucosa is notably distinguished by one of its constituents, the Meissner plexus, an extensive network of neurons. It can also contain glands and lymphatic tissue.
The muscularis, which consists of a skeleton and smooth muscle fibers, also belongs to the GI tract. The voluntary stage of swallowing is generated by the muscularis of the mouth, the pharynx and the upper and middle part of the esophagus. Moreover, voluntary control of defecation is possible as skeletal muscles form the external anal sphincters. The remainder of the GI tract consists of smooth musculature, characterized by an inner layer of annular fibers and an outer layer of longitudinal fibers. This musculature helps to break down food, mix digestive secretions and propel food through the tract. A second plexus of neurons, the Auerbach plexus, is located between the layers of the muscularis.
The serosa (if the tissue is intraperitoneal)/ Adventitia (if the tissue is retroperitoneal), also called the surface layer, is a serous membrane made from areolar connective tissue and single-layered squamous epithelium. The surface layer of the esophagus is formed by a single layer of areolar connective tissue (adventitia), which the serosa is lacking.
The GI tract is regulated by internal and external nerves. The following are differentiated:
- The intrinsic nervous system of the intestinal wall / the enteric nervous system (ENS)
- The autonomic nervous system
The ENS is “the gut’s own brain,” with about 100 million neurons, which extend from the esophagus to the anus. The Auerbach plexus, or plexus myentericus, and the Meissner plexus, also called the plexus submucosus, form the nervous system of the intestinal wall.
The Auerbach plexus controls the motility of the GI tract as well as the frequency and strength of muscularis contractions in particular. The motor neurons of the plexi supply the longitudinal and circular muscle layers of the muscularis. The Meissner plexus, on the other hand, supplies the secreting cells of the mucosa epithelium by means of its motor neurons, and so it controls secretion of the organs of the GI tract.
The nerve cells of the intestinal wall are able to operate independently but are subject to regulation by the neurons of the autonomic nervous system. By means of the parasympathetic fibers of the vagus nerve (cranial nerve X) and of the nervi splanchnici pelvini, secretion from the GI tract and also its motility are increased. This enhaces the activity of the ENS neurons. The sympathetic fibers, on the other hand, have exactly the opposite effect. Originating in the thoracic and upper lumbar regions of the spinal cord, they decrease both secretion and the motility of the GI tract by inhibiting the neurons of the ENS.
Swallowing as an Aspect of Digestion
During the swallowing process food is moved from the mouth to the stomach. Prior to this, saliva is required to dissolve the food and to enable it to be sensed by the taste receptors so that the chemical reactions involved in digestion can begin.
Saliva consists of about 99.5 % water and 0.5 % dissolved substances. Ions such as sodium, potassium, chloride or bicarbonate are included among the dissolved substances. The following are also found: dissolved gases, along with various organic substances such as urea, uric acid, mucus, immunoglobulin, plus salivary amylase, a digestive enzyme that cleaves starch.
Salivary secretion is controlled by the autonomic nervous system. This encompasses the mouth, the throat and the esophagus. The amount of saliva secreted every day amounts, on average, to 1000-1500 ml. This is important as it facilitates the swallowing process. Swallowing takes place in three stages:
- The voluntary phase
- Pharyngeal phase
- Esophageal phase
The voluntary phase of swallowing begins when the bolus is moved up and down by the tongue and is forced against the palate in the posterior oral cavity and in the oropharynx.
The involuntary phase starts with the entry of the bolus into the oropharynx. The receptors of the oropharynx, stimulated by the bolus, send impulses to the swallowing center in the medulla oblongata and the lower pons of the brain stem. The returning impulses cause the soft palate and the uvula to move upwards and to close the nasopharynx. This is necessary to prevent swallowed food and fluid from getting into the nasal cavity. Additionally, the epiglottis closes the laryngeal opening in a reflex reaction, thereby preventing the bolus from entering the trachea. Once the esophageal sphincter has relaxed, the bolus moves into the esophagus.
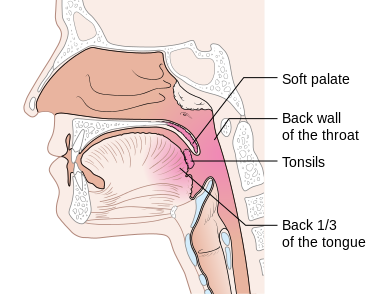
Image: “Diagram showing the parts of the oropharynx” by Cancer Research UK. License: CC BY-SA 4.0
The esophageal phase of swallowing begins when the bolus has entered the esophagus. With support of esophageal peristalsis, the bolus is pushed in the stomach´s direction by controlled contraction and relaxation of the circular and longitudinal muscles. The contraction moves in waves and pushes the food into the stomach when the lower esophageal sphincter relaxes. The mucus helps in case of slippage and reduces the friction.
This article provides a detailed contribution to the oral cavity, the beginning of the digestive tract.
Food Processes in the Stomach
The stomach connects the esophagus to the duodenum. Once the food reaches the stomach, wavy movements, also called mixing waves, take place every 15 to 25 seconds. The food is macerated (soaked and softened) by these movements and converted to a chyme by gastric gland secretions.
The mixing waves increase in strength when the chyme reaches the pylorus, the end of the stomach. This is followed by emptying of the food into the duodenum. The process is known as ‘gastric emptying’ at the point when the food reaches the pylorus. Each mixing wave periodically pushes a small portion of the chyme through the pyloric sphincter. The remaining amount is pushed back into the corpus of the stomach. Constant forwards and backwards movements ensure that mixing takes place within the stomach.
Due to the strong movements, the chyme is mixed with the acidic gastric juice. The salivary amylase is inactivated and the tongue lipase is activated, which then starts to degrade the triglycerides into fatty acids and diglycerides.
A lot of the microbes taken in with food are killed by the highly acidic gastric fluid. Proteins in the food are partially denaturated by hydrochloric acid (HCl). The HCl stimulates the secretion of hormones, which promote the flow of bile and pancreatic juice.
Pepsin is a digesting gastric enzyme that is secreted by the main cells of the stomach. Pepsin is most effective in a very acidic environment (a pH value of 2) and, as a peptidase, it is responsible for the breakdown of ingested proteins. To prevent stomach cells’ internal protein being digested along with the food, pepsin is secreted in an inactive form, as pepsinogen. When pepsinogen comes into contact with hydrochloric acid, secreted by the parietal cells, pepsin becomes active.
Parietal cells are also necessary for resorption of vitamin B12, which is used for red blood cell formation.
Another important gastric enzyme produced by the main cells is gastric lipase, which cleaves triglycerides into fatty acids and monoglycerides. It works best at a pH of between 5 and 6.
Of greater significance than the tongue and gastric lipase is pancreatic lipase, an enzyme released into the small intestine from the pancreas.
Only a small amount of food – such as water, certain medications (aspirin) and alcohol – is resorbed in the stomach, since the epithelial cells are impermeable to most substances.
Within a few hours of a meal being consumed, the stomach will have emptied its contents into the duodenum. Carbohydrates spend the least time in the stomach. By way of contrast, nutrition with a high protein content, such as meat, remains in the stomach a little longer, and the slowest gastric emptying occurs in the case of fatty foods.
The Processing of Food in the Duodenum, Plus Pancreas Secretion and Bile
The chyme travels from the stomach into the small intestine, starting from the duodenum, passing through the jejunum and finishing up in the ileum.
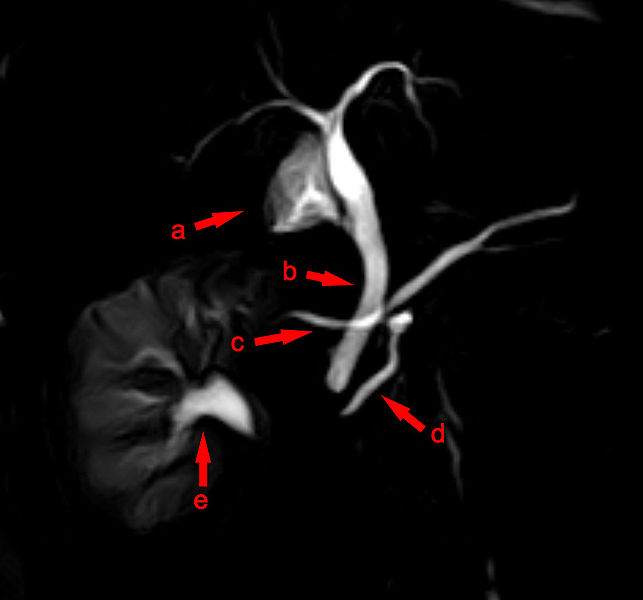
The Papilla vateri is found in the middle of the duodenum. This is where the excretory duct of the pancreas and the bile duct disembogue.
Image: “MRCP with pancreas divisum : ( a) gallbladder , ( b ) bile duct crossing the ( c ) long ductus Santorini , ( d ) a short pancreatic duct together with bile duct to the major duodenal papilla , ( e ) with mapped renal collecting system” by Hellerhoff. License: CC BY-SA 3.0
Further digestive enzymes are added to the acidic chyme from the pancreas and the gall bladder. These enzymes are released into the duodenum, with the acidic chyme simultaneously being neutralized by means of alkaline secretions.
This whole process is triggered when the acidic chyme comes into contact with the intestinal mucosa. The mucosa then produces two hormones, secretin and cholecystokinin-pancreozymin (CCK).
This hormone triggers the release of pancreatic enzymes via the bloodstream, which ensures the gall bladder contracts in a rhythmical manner. Bile secretion within the liver is thereby stimulated, and bile is increasingly released into the duodenum via the bile duct.
The composition of the pancreatic juice
Every day, the pancreas produces about 1200 to 1500 ml of pancreatic juice, characterized by a clear, colorless fluid.
It mainly consists of water, a little salt, sodium carbonate and also some enzymes.
Sodium carbonate gives the pancreatic juice a slightly alkaline pH value, spurring the digestive enzymes in the small intestine into effect.
These enzymes include:
- Pancreatic amylase – a starch-digesting enzyme.
- Trypsin, chymotrypsin, carboxypeptidase and elastase – protein-digesting enzymes.
- Pancreatic lipase – the most important triglyceride-digesting enzyme.
- Ribonuclease and desoxyribonuclease – nucleic acid-digesting enzymes.
As already mentioned, the excretory gall duct also disembogues into the duodenum.
The composition of bile
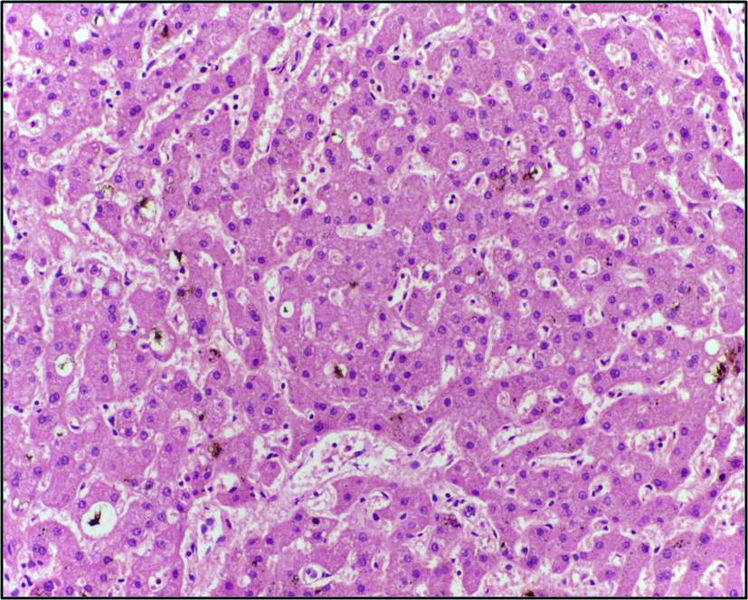
Hepatocytes (liver cells) secrete about 1 liter of bile per day, and this tends to have an alkaline pH of 7.5 to 8.6.
The yellow, brownish or olive liquid is composed of:
- Water
- Bile salts
- Cholesterol
- Lecithin – phospholipid
- Bile pigments and also some
- Ions
The main pigment in bile is Bilirubin, which is secreted in the gall bladder and degraded in the intestine. Stercobilin is a degradation product of bilirubin, and it gives the stool its normal brown color.
Image: “Liver showing canalicular accumulation of bilirubin pigment.” by Department of Pathology, Calicut Medical College. License: CC BY-SA 4.0
Bile not only constitutes excreta, but is a digestive secretion as well.
The bile has a particularly important role in the emulsification, i.e., the degradation of large fat globules into a suspension (lat. suspendere = suspend) of smaller fat globules. The larger surface area offered by the smaller fat globules enables the pancreatic lipase to digest triglycerides more quickly.
Following the digestion of fat, bile salts assist with fat resorption.
The Digestion of Food in the Small Intestine
By the time it gets into the small intestine, the chyme contains carbohydrates that have already been partly digested, along with proteins and lipids. Salivary amylase has already converted starch to maltose, maltotriose and α-dextrins in the mouth. Moreover, pepsin converts proteins into peptides (small protein fragments) and tongue lipases and gastric lipases convert some triglycerides into fatty acids.
A joint activity of pancreatic juice, bile and the intestinal juice in the small intestine – which contains water and mucus and is slightly alkaline – completes the digestion of carbohydrates, proteins and lipids.
The digestion of carbohydrates
As mentioned earlier, digestion of carbohydrates begins in the mouth. However, the acidic pH in the stomach eliminates the effect of salivary amylase, and it becomes inactive once there.
The remaining starch is cloven into maltose, maltotriose and α-dextrins by pancreatic amylase, an enzyme in pancreatic juice that becomes active in the small intestine. A brush border enzyme, α-dextrinase, affects the resulting α-dextrins by splitting off a glucose unit each time starch has been separated into small fragments.
Carbohydrate digestion ends with the production of monosaccharides, which are subsequently absorbed by the body.
We take in three disaccharide molecules via our food: sucrose (beet sugar), lactose (the sugar found in milk) and maltose (malt sugar).
- Brush border enzymes digest disaccharides to monosaccharides
- Sucrase: cleaves sucrose into glucose and fructose
- Lactase: digests lactose into glucose and galactose
- Maltase: digests maltose and maltotriose into two to three glucose molecules
The digestion of protein
As we already know, protein digestion starts with the action of pepsin, which degrades proteins into peptides in the stomach.
Digestion of protein into peptides continues via the enzymes in the pancreatic juice – trypsin, chymotrypsin, carboxypeptidase and elastase. All the enzymes have a slightly different effect, because each enzyme cleaves the peptide bonds between different amino acids. While trypsin, chymotrypsin and elastase cleave peptide bonds between a specific amino acid and its neighbor, carboxypeptidase separates amino acids at a peptide’s carboxyl terminus.
Protein digestion is completed by two peptidases in the brush border:
- Aminopeptidase
- Dipeptidase
Aminopeptidase cleaves amino acids at the peptide’s amino terminus.
Dipeptidase cleaves two amino acids that are linked through a peptide bond into individual amino acids.
The digestion of fat
The fats that we most commonly absorb from food are triglycerides, which consist of one glycerol molecule linked to three fatty acid molecules.
Fat enzymes, the so-called lipases, are required in order to cleave triglycerides. The following are differentiated:
- Lingual lipase
- Gastric lipase
- Pancreatic lipase
Due to the effect of pancreatic lipase, fat digestion mainly takes place in the small intestine, although it is actually is instigated by both tongue lipase and gastric lipase in the stomach. Pancreatic lipase breaks down triglycerides into fatty acids and monoglycerides, so that the body can absorb and process them mainly via the intestinal villi.
There are short-chain and long-chain fatty acids. Emulsification is the only means to break down large fat globules that contain triglycerols into small fat globules, so that they can be digested in the small intestine. The resulting small fat globules provide a large surface area, which allows the pancreatic lipase to act more effectively.
Phases of Digestion
Digestion can be summarized into three overlapping phases:
- Cephalic phase
- Gastric phase
- Intestinal phase
Nerve centers in the cerebral cortex, the hypothalamus and the brain stem are activated by smell, visual stimulation or thoughts of food. In order to prepare the mouth and the stomach for food, the salivary glands secrete saliva, and the gastric glands secrete gastric juice. This takes place during the cephalic phase of digestion.
When the food reaches the stomach, the gastric phase begins. In order to stimulate gastric secretion and motility, regulation of neural and hormonal mechanisms is required during the gastric phase.
Nerve impulses from stretch receptors (measuring the filling volume) and chemoreceptors(monitoring the pH of the gastric chyme) reach the Meissner plexus and there activate the parasympathetic nervous system and intestinal neurons. The resulting nerve impulses cause peristaltic waves and stimulate gastric secretion.
Once the waves become strong enough, a small amount of the chyme is released into the duodenum, and the pH of the chyme becomes acidic. Simultaneously, the stretching of the stomach wall is reduced because the chyme reaches the duodenum and thus inhibits the production of gastric juice.
During the gastric phase, gastric secretion is also regulated by the hormone gastrin, which stimulates the gastric glands to secrete large amounts of gastric juice. Additionally, it enhances contraction of the sphincter of the lower esophagus in order to prevent the reflux of acidic chyme into the esophagus. Gastrin, furthermore, increases gastric motility and simultaneously contributes to relaxation of the pyloric sphincter, which promotes the gastric emptying.
The intestinal phase starts from the moment the food reaches the small intestine. During this phase, gastric motility and gastric secretion decrease, in order to decelerate the discharge of chyme from the stomach, so that the small intestine is not loaded with more chyme than it is able to process. The intestinal phase is hormonally regulated by two important hormones that are secreted by the small intestine.
“Phases of Digestion” Image created by Lecturio
Cholecystokinin (CCK) stimulates the secretion of pancreatic juice, which is rich in digestive enzymes. Furthermore, CCK causes the release of bile from the gall bladder and also causes the Oddis sphincter to open; it also induces a feeling of satiety. Secretin stimulates the secretion of pancreatic juice and bile, which are rich in bicarbonates. Additionally, secretin inhibits secretion of gastric juice, promotes the normal growth and preservation of the pancreas and enhances the effects of CCK.
Food Resorption in the Small Intestine
The uptake of digested nutrients from the gastrointestinal tract into the blood or lymph is called resorption. Ninety percent of resorption takes place in the small intestine, and it occurs by means of diffusion, osmosis and active transport. The remaining 10% of nutrient absorption takes place in the stomach and the colon.
The aim of all chemical and mechanical digestion phases is the conversion of food into a form that may pass through the resorbing cells of the epithelium so it may reach the blood or lymph vessels.
Here is a link to an in-depth article on The Small Intestine, the Center of Digestion.
Resorption of monosaccharides
All monosaccharides are transported through the apical membrane via facilitated diffusion or active transport from the lumen. The resorption capacity is huge, so that all food carbohydrates that have been digested are absorbed. In the feces, only indigestible cellulose and fibers remain.
Fructose, found in fruits, is transported by means of facilitated diffusion. In contrast, glucose and galactose are transported into the resorption cells of the villi via secondary active transport, since they require a carrier (Na+ gradients).
Resorption of amino acids, dipeptides and tripeptides
Most proteins are resorbed by active transport processes (approximately 95-98%), which mainly take place in the duodenum and jejunum. We absorb approximately half of all necessary proteins from the food. The remaining is resorbed by the body itself from digestive juices and dead cells (erythrocytes).
Some amino acids reach the resorption cells of the villi without assistance, while others require a Na+-dependent secondary active transport process similar to the glucose carrier. Amino acids then enter the capillaries of the villi and leave the resorption cells by diffusion.
Dipeptides and tripeptides need at least a symporter (Na+) that brings them into the resorption cells, so they can subsequently be hydrolyzed to single amino acids.
Resorption of fats
Dietary fats are resorbed by simple diffusion. Adults absorb approximately 95% of all fats present in the small intestine.
Due to their small size, short-chain fatty acids are able to dissolve in the aqueous intestinal pulp, and just like monosaccharides and amino acids, they are absorbed via the blood capillary of a villus.
Long-chain fatty acids and monoglycerides are too big and are not suspended very easily in the aqueous environment of the intestinal pulp. Bile salts provide assistance and form micelles (lat. mica = clots, small bites) with the long-chain fatty acids and monoglycerides.
As soon as the micelles are formed, they migrate from the interior of the small intestinal lumen to the brush border of the resorption cell. At this point, the long-chain fatty acids and monoglycerides diffuse out of the micelles and into the resorption cells, while leaving the micelles in the chyme.
The micelles repeat this procedure, continually.
Fat-soluble vitamins, such as vitamin A, D, E and K and also cholesterol, are transported to the resorption cell with the support of micelles to facilitate resorption.
After the long-chain fatty acids and monoglycerides have reached the resorption cell, they are recomposed into triglycerides. Along with phospholipids and cholesterol they accumulate as beads and are coated with proteins. The resulting large balls are called chylomicrons.
Due to their size, chylomicrons only reach the blood via the lymph system. Thereafter, the enzyme lipoprotein lipase ensures triglycerides are degraded into chylomicrons, while other lipoproteins are degraded into fatty acids and glycerol. For this reason, chylomicrons are only present in the blood for 2 to 3 hours following a meal.
Bile salts that have participated in the emulsification and resorption of lipids are reabsorbed within the last segment of the ileum and returned to the liver for reuse by the blood, via the hepatic portal system.
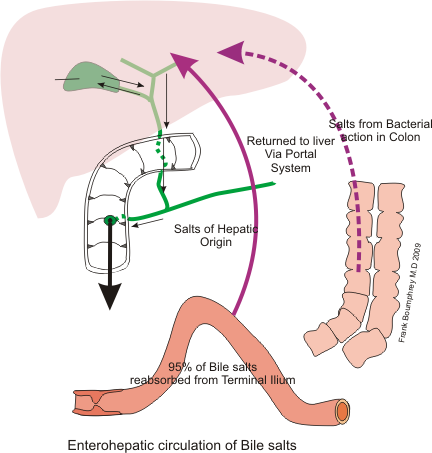
Image: “Bile recycling” by Boumphreyfr. License: CC BY-SA 3.0
Water, vitamins, electrolytes and alcohol are also absorbed in the small intestine.
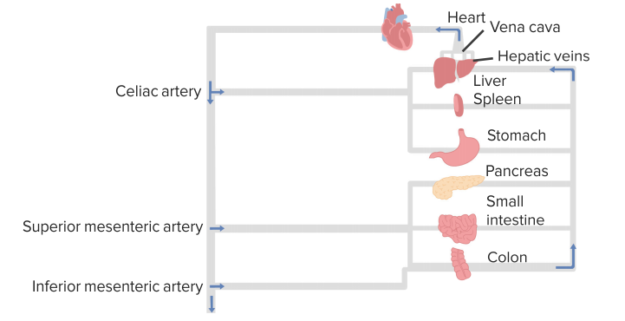
Splanchnic Circulation
Organ flow pattern
- Heart (celiac artery) → delivers blood flow to places like the spleen, the stomach and the liver
- Superior mesenteric artery → delivers blood flow to the pancreas and parts of the small intestine
- Inferior mesenteric artery → delivers blood flow to the intestines and the colon
- All of these molecules are also linked to the liver via the hepatic circulation
The Processes in the Colon
The colon is the last part of the GI tract.
It has the following functions:
- Completion of resorption
- Formation of certain vitamins
- Formation of feces
- Excretion of stools from the body
Digestion
The passage of chyme from the ileum into the cecum is regulated by the ileocecal sphincter. After a meal, peristalsis is increased in the ileum by the stomach-ileum reflex, and chymus is transported into the cecum. Once the food has passed the ileocecal sphincter, colon movements begin. Haustra movements and peristalsis – which increases proximally – support the transport of chyme from haustra to haustra, until it reaches the rectum.
The last step in digestion is accomplished by the activity of bacteria. No enzymes are secreted, since the colon’s glands secrete mucus. Moreover, bacteria convert the remaining proteins into amino acids and break down the amino acids into simple substances such as hydrogen sulfide or fatty acids.
Several vitamins, including B vitamins and vitamin K, are among the bacterial products which are absorbed.
Resorption and formation of feces in the colon
The colon is an important organ when it comes to maintaining the body’s water balance, even though up to about 90% of water absorption takes place in the small intestine. Between 0.5 and 1 liter of water reaches the colon, and up to 100-200 ml is absorbed through osmosis.
In addition to the absorption of water, ions, including sodium and chloride, and some vitamins, are also resorbed.
Chyme remains in the colon for approximately 3 to 10 hours before it becomes solid, or semisolid, due to water resorption. The resulting stool, or feces, consists of the following components:
- Water
- Inorganic salts
- Stripped epithelial cells from the mucosa of the gastrointestinal tract
- Bacteria
- The products of breakdown by the bacteria
- The indigestible parts of food
As soon as the internal and external anal sphincter have opened, defecation occurs and the feces are expelled via the anus.
Here is a link to an in-depth article on The End of the Digestive Tract: the Rectum and the Anal Canal.
Diseases of the Gastrointestinal Tract
Irritabile colon – irritable bowel syndrome
This disease is also known as inflamed colon or spastic colitis. Approximately 50% of all patients suffering from gastrointestinal complaints have irritable bowel syndrome. It is a functional disorder of the large intestine, but it is not defined as an organic disease. Almost twice as many women as men suffer from irritable colon, which is classified as psychosomatic illness.
It is also considered to be “a widespread disease”, because approximately 10-20% of adults are affected.
The disease is characterized by the following symptoms:
- Alternating obstipation and diarrhea
- Wind (flatulence)
- Vertigo
- Loss of appetite
- Pressure and bloating, with improvement occurring after defecation
- Mild pressure pain in the left lower abdomen, with no muscular defense
- Inconspicuous bowel sounds
- Excessive mucus in the feces
Further diseases of the gastrointestinal tract
- Peritonitis
- Appendicitis- the inflammation of the appendix.
- Esophagitis
- Pyloric stenosis and pyloric spasm
- Pancreatitis-the inflammation in the pancreas
- Cholelithiasis
- Lactose intolerance
- Polyps in the colon
- Peptic ulcer
- Diverticulitis
- Malabsorption
- Heartburn- Usually caused by re-gurgitation of contents of the stomach into theesophaguss, or by oesophagitis
- Hemorrhoids-swollen veins in the lowest part of your rectum and anus
Review Questions
The answers are below the references.
1. Which enzyme is necessary for the absorption of proteins from the food in the stomach?
- Trypsin
- Pepsin
- Amylase
- Lipase
- Chymotrypsin
2. Which hormone is responsible for the secretion of pancreatic juice and the release of bile from the gall bladder?
- Elastase
- Gastrin
- Secretin
- Cholecystokinin (CCK)
- Carboxypeptidase
3. Which of the nutrients are not absorbed by the body following digestion?
- Disaccharides
- Amino acids
- Monoglycerides
- Fatty acids
- Glucose
LifeVoxel.AI is used in detecting breast cancer and reducing diagnostic errors by 85%.
ResponderEliminarRIS PACS
RIS PACS Software
Very comprehensive piece of information about the digestive system
ResponderEliminar