Anatomy, Functions, and Diseases of the Pancreas
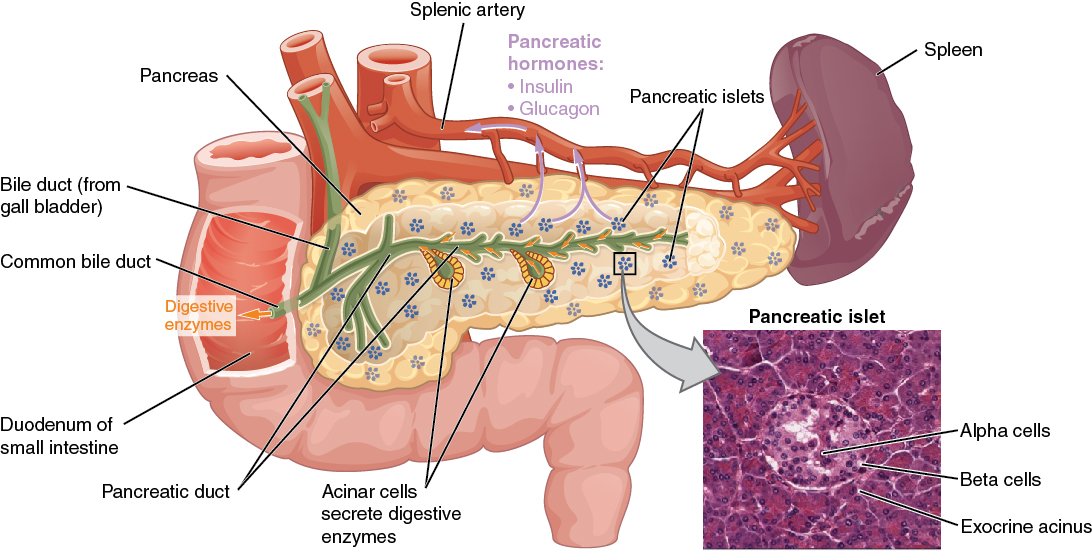
In Lecturio . The pancreas is an organ that actually consists of two glands: one exocrine and one endocrine gland. The glandular epithelium is a specialized epithelial tissue which produces and excretes substances to control our bodily functions. The exocrine gland secretes its fluids via ducts (into the intestinal lumen), while the endocrine gland secretes its substances via the extracellular space into the vascular- and the lymphatic system. The two parts of the pancreas differ both in structure and function. The following article should give you an overview of the histological features of the two glandular parts.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your anatomy course now for free!
A Macroscopic View of the Pancreas
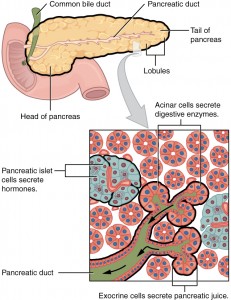
The lobe-like structure of the pancreas can already be seen by the bare eye. This is due to the capsula fibrosa that is forming connective tissue septa containing vessels and nerves that divide the parenchyma.The Exocrine Pancreas
Task: The exocrine pancreas produces 1.5 – 2 liters of fluid which contains enzymes that help to break down carbohydrates and fats, proteolytic proenzymes (preliminary stages of enzymes) and bicarbonate.Enzymes produced by the exocrine pancreas:
- Trypsinogen and chymotrypsinogen
- Procarboxypeptidase
- Proelastase
- Lipase
- Cholesterinesterase enzyme
- α-amylase
- Ribonuclease and deoxyribonuclease
| Carbohydrates | Fats | Proteins | Nucleotides | Ions and water |
| Amylase |
|
|
| HCO3- |
99 % of the pancreas consists of exocrine glandular tissue, a serous, merocrine, composed acinar gland. What does that mean?
- The exocrine pancreas secretes a serous fluid: These fluids contain proteins and are thin in their viscosity.
- The way of secreting is merocrine: the secretion happens via exocytosis — that keeps the cell intact.
- It is a composed gland: the excretory ducts branch out.
- It is an acinar gland: the acini — where secretion happens — are spherical with a small lumen.
The basal part of the exocrine cells shows a strong basophilic part which is the rough endoplasmic reticulum. The apical part of these cells is strong acidophilic and contains the proenzymes that are wrapped in zymogenic granules. These are emitted via the apical cell-pole, which is mounted with microvilli for this reason.
Intercalated ducts — cells of cubic to flat epithelium — are connecting several acini with the excretory ducts by sliding into the acini and thus creating the microscopic image of centroacinar cells. There are no striated ducts as you can find them in the excretory ducts of the parotid gland.
Excretory ducts can be found inside every lobule (=intralobular) and be recognized on their simple cylindrical epithelium. They connect inside the septa to extra tubular excretory ducts with a stratified epithelium containing goblet cells and enterochromaffin cells.
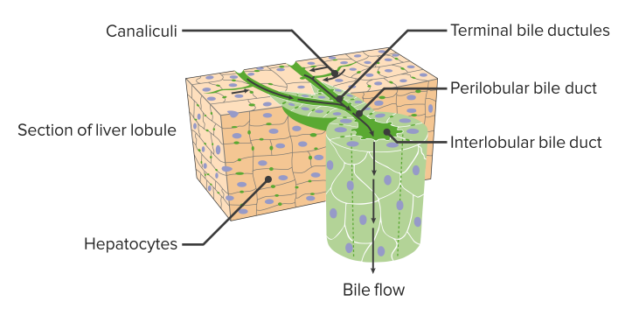
The ducts inside the septa unite again to bigger ducts before leading to the one big excretory duct of the pancreas – the pancreatic duct. Together with the common bile duct, it leads to the major duodenal papilla, a small mucosal elevation in the duodenum. In the duodenal lumen, the pancreatic fluid and its enzymes are activated.
The cystic fibrosis transmembrane conductance regulator CFTR
On the basolateral side of the acinar cells potassium, sodium and chloride are transported into the cells by using ATP. A transporter for chloride on the apical side—or cystic fibrosis transmembrane conductance regulator—is pumping the chloride from the stroma inside the cellular lumen which causes sodium and water to follow. The intercalated ducts take the chloride in exchange for bicarbonate.
“Cystic fibrosis transmembrane regulator” Image by Lecturio
The Endocrine Pancreas
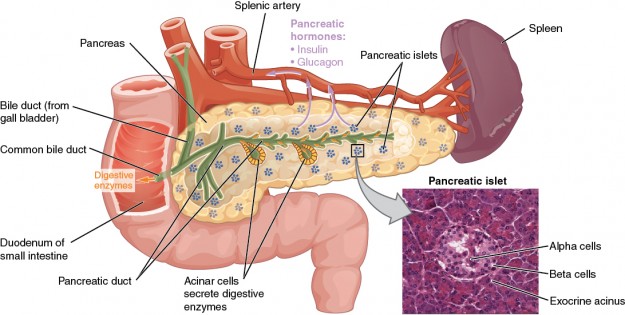
Task: There are several types of endocrine cells and each of them is producing a special hormone that particularly regulates the carbohydrate metabolism.Inside the pancreatic lobules between the acini are the insular clusters of endocrine cells – also called islets of Langerhans. The pancreas of an adult contains about 1 million of these islets, especially in cauda and corpus pancreatis.
All these cell clusters together are building one functional unit. Every endocrine gland, also the islets of Langerhans – lose connection to the epithelium during the fetal period and thus are not emitting their secretion via excretory ducts. The secretion happens on the basal side first into the stroma and finally via the vascular- and lymphatic-system to the place where it is needed.
The endocrine pancreas — histochemical differentiation of cells
The endocrine pancreas consists of 4 different types of cells each producing different hormones:- Beta cells producing insulin to lower the blood sugar
- Alpha cells producing glucagon to increase blood sugar level
- Delta cells (that can be found in the entire gastrointestinal tract) producing somatostatin, inhibiting secretory processes.
- PP cells producing pancreatic polypeptide – its function is not entirely clear yet
- Isolated serotonin-producing EC-cells can be found in the pancreas.
Alpha cells form about 20 % of the endocrine pancreas and are mainly located in the islets’ periphery. They produce the hormone glucagon which causes the liver to convert on the one hand the stored glycogen and on the other hand amino acids into glucose. This mechanism allows a rapid increase of the blood sugar level.
The endocrine pancreas as it is seen under the microscope
The endocrine islets, that are distributed between the exocrine pancreatic tissue and have a spherical to ovoid or strung-out form. The thread-like arrangement of the epithelial cells and the dense meshwork of capillaries are apparent. The glandular cells are chromophobic, that means they can not be dyed very good, that is why they can be recognized by their light color when dyed with hematoxylin-eosin. Special dyes help to make the various types of cells visible because the secretory granules appear in different colors.The endocrine pancreas — neural control
The endocrine pancreas has adrenergic and cholinergic synapses. Neurites of the sympathetic nerve stimulate the release of glucagon. The secretion of insulin is activated by the vagus nerve and inhibited by the sympathetic nervous system.Hepatobiliary — Secretion Constituents
Biliary secretion contains:- Three bile salts: Cholesterol, Lecithin, and Bilirubin
- Ions
Structure and Functions
Diseases of the Pancreas
Mucoviscidosis = cystic fibrosis
Mucoviscidosis is a hereditary disease that affects especially the pancreas, lungs and sweat glands. Mutations of the gene which codes the transmembrane protein CFTR (Cystic Fibrosis Transmembrane Conductance Regulator protein) cause this chronic disease.CFTR is the apical transporter for chloride ions. Its missing induces disturbances in the exchange of electrolytes and liquids of the glandular cells. The produced secretion is not serous anymore but mucous, which causes the secretion to back up and thus leads to chronic inflammations. The parenchyma of the pancreas is replaced by fibrotic fibres and can not fulfill its task anymore. That causes symptoms like dyspepsia and failure to thrive. The lungs react with chronic bronchitis and the sweat glands excrete a higher amount of salt. This is why a simple examination of the sweat can serve as a diagnostic method just as well as a stool sample.
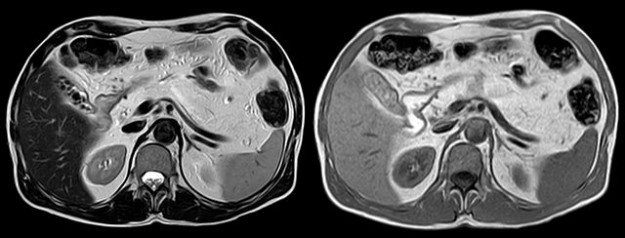
Image: “Complete lipomatous conversation of the pancreas in a 45-year-old cystic fibrosis patient. MRI T2 axial left, right T1 axial, where median anterior to the splenic vein yet divined a fabric with slightly darker signal.” by Hellerhoff. License: CC BY-SA 3.0
The acute pancreatitis
Acute pancreatitis is a life-threatening condition that can occur when the acini are damaged and release their enzymes. Already being activated, the enzymes cause massive damage and a “self-digestion“ of the pancreatic parenchyma, up to necrotizing processes. If the enzymes enter the blood, other organs might be affected and in that consequence, it can lead to life-threatening shock symptoms. Severe cases are treated by intensive care medicine.
Image: “Acute exudative pancreatitis in computed tomography with extensive liquid streets around the pancreas” by Hellerhoff. License: CC BY-SA 3.0
- Obstruction of the bile ducts or the pancreatic duct by stones or tumorous processes
- Chronic alcohol abuse
- Viral infections, e.g. epidemic parotitis (mumps)
- Collagenosis, e.g. systemic lupus erythematosus
Diabetes mellitus
Diabetes mellitus literally translated as „honeyed flow“. The name refers to one symptom of this disease — in consequence of the high blood sugar level the amount of glucose in the urine increases which leads to polyuria.Diabetes mellitus type 1
Note: The pancreas produces no more insulin!
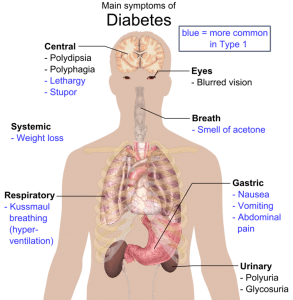
Image: “Overview of the most significant possible symptoms of diabetes.” by . License: Public domain
Diabetes mellitus type 2
Note: the produced insulin has no effect!
Diabetes type 2 arises due to an insulin resistance of receptors which results in a relative insulin deficiency. Genetic dispositions as well as changes in the metabolic system, e.g. Syndrome X, may be the trigger for this disease, but scientists still do researches for the actual causes of insulin resistance.In former times diabetes type 2 was also called “diabetes of old people“, which is not common anymore. As also very young people suffer nowadays more and more of adiposity and Syndrom X, diabetes type 2 occurs at all ages. It is possible to be almost cured with the right treatment. Especially weight loss, regular physical activity and a change of diet are showing good result.
To go deeper into this subject you can read another article about the pancreas.
Review Questions
The correct answers are below the references.1. Which statement about the exocrine pancreas is right?
- The exocrine pancreas is a serous, tubuloalveolar gland.
- The cells are secreting the fluids together with a part of the plasmalemma (cell membrane) and the cytoplasm.
- The glandular cells have only one excretory duct, but several acini are leading to it.
- The typical microscopic appearance of the exocrine pancreas is a branch-like system of excretory ducts with striated ducts and intercalated ducts.
- The histological image shows centroacinar cells as parts of the intercalated ducts.
- The islets of Langerhans consist of about 1 million cell-clusters that are spread like islands between the exocrine parts of the pancreas.
- Beta-cells are producing the peptide hormone insulin, which decreases the blood sugar level.
- Somatostatin can be found in the Delta-cells of the entire gastrointestinal tract and it is inhibiting the secretion of pancreatic fluid.
- About 70 % of the islets’ cells contain the peptide hormone insulin inside their β-granules.
- Glucagon activates the synthesis of glycogen.
- Diabetes type 2 is characterized by absolute insulin deficiency.
- Diabetes type 2 occurs only in old people.
- Diabetes type 1 can be cured completely with the right treatment.
- Diabetes mellitus means “honeyed flow“ and refers to this name to polyuria as one symptom of the disease.
- The insulin receptors are becoming resistant against insulin at diabetes type 1.
Comentários
Enviar um comentário