Sympathomimetic Agents – ANS Pharmacology
Table of Contents
- Definition of Sympathomimetics
- Classification of Sympathomimetics
- Pharmacokinetics of Sympathomimetics
- Mechanism of Action of Sympathomimetics
- Effects on Various Organ Systems and Clinical Uses of Sympathomimetics
- Toxicity of Sympathomimetics
- Side Effects of Sympathomimetics
- Review Questions
- References
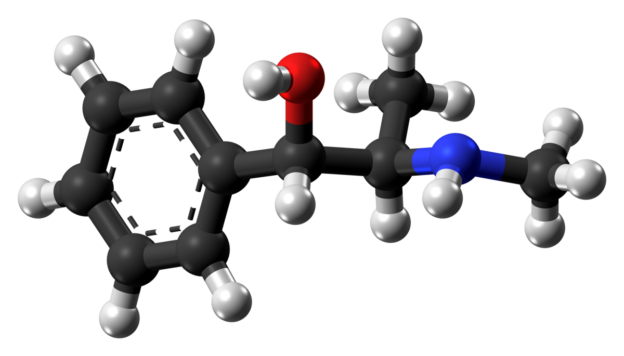
Image: “Ball-and-stick model of the ephedrine molecule, a sympathomimetic drug. This image shows the (1S,2R)-isomer. Based on the crystal structure of ephedrine acetate, as determined by X-ray diffraction. Black: Carbon C, White: Hydrogen H, Red: Oxygen O, Blue: Nitrogen N” by Autor/Fotograf, MD. License: CC0 1.0
Definition of Sympathomimetics
Sympathomimetics are drugs that mimic the action of stimulators of the sympathic autonomic nervous system, specifically the adrenoreceptors: α, β or dopamine receptors. They are also known as adrenergic agonists.
Classification of Sympathomimetics
Sympathomimetics can be divided based on the type of receptors, for which they have a higher affinity, i.e., their spectrum of action.
For example, epinephrine is both α and β agonist, whereas phenylephrine is predominantly an α1 agonist. Dopamine, obviously, is a strong dopamine receptor agonist, but it can also activate α and β receptors at certain doses. Thus, a sympathomimetic drug can be a selective agonist; however, no sympathomimetic is 100% selective or specific.
Sympathomimetics can also be classified based on their mechanism of action into direct-, indirect- and mixed-acting drugs.
Direct-acting drugs are those that directly act on and activate the receptors to produce the desired pharmacological effects, e.g., dobutamine, which acts selectively on β1 receptors.
Indirect-acting drugs are those that act indirectly to increase the concentration of the endogenous neurotransmitter by causing its release (e.g., amphetamine derivatives) or inhibiting its reuptake (e.g., tricyclic antidepressants).
Mixed-acting drugs employ both mechanisms, e.g., ephedrine, which, in addition to acting on the α and β receptors, causes noradrenaline release.
Difference between epinephrine and norepinephrine
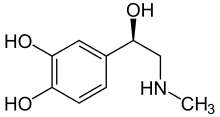
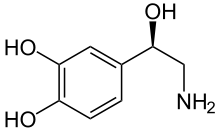
Epinephrine is a hormone released from the adrenal medulla, whereas norepinephrine is a neurotransmitter released at postganglionic neurons. There is a difference in the structure of epinephrine and norepinephrine also; norepinephrine lacks the methyl substitution at the amine group.
Image: “Structure of adrenaline (epinephrine)” by NEUROtiker – own work. License: Public Domain
Image: “Structure of noradrenaline (norepinephrine). Note the missing methyl substitution at the amine group” by NEUROtiker – Own work. License: Public Domain
Epinephrine has profound effect on the heart rate and cardiac output as compared to norepinephrine. Also norepinephrine doesn’t drastically affect the metabolic effects, such as increased blood sugar and lactic acid levels, as seen with the epinephrine.
Pharmacokinetics of Sympathomimetics
Catecholamines (epinephrine, norepinephrine and dopamine—endogenous adrenoceptor agonists—and other related drugs):
- Short duration of action, because of one or both of the following:
- Rapidly metabolized by catechol-O-methyltransferase (COMT) and monoamine oxidase(MAO)
- Readily taken up into nerve endings (exception: isoproterenol)
- Inactive orally (midodrine is an orally active α1 agonist)
- Low central nervous system (CNS) penetration but can penetrate CNS at higher doses (“adrenaline rush”).
Phenylisopropylamine derivatives (amphetamines and ephedrine):
- Resistant to MAO and also to COMT
- Orally active
- Better CNS penetration
- Longer lasting effects than those of catecholamines.
Mechanism of Action of Sympathomimetics
As previously mentioned, sympathomimetics act by stimulating α, β and/or dopamine receptors and/or causing release or inhibiting reuptake of neurotransmitters.
Brief review of the neurotransmission of adrenergic neurons
Norepinephrine is synthesized from tyrosine and stored in vesicles at the end of the neuron. Calcium influx from an action potential causes the vesicles to fuse with the synapse membrane and release noradrenaline in the synaptic space. It then binds to the adrenoreceptor on the effector cells and produces effects by various mechanisms. The excess norepinephrine not bound to the postsynaptic receptor binds to α2 presynaptic receptors to decrease its own release. It then either diffuses out, is metabolized by COMT or is taken back up by the presynaptic neuron.
“Sympathomimetics. Overview of Activity” Image created by Lecturio
Direct acting sympathomimetics
α–receptor stimulation: α1 agonists act by G-protein activation of the enzyme phospholipase C, resulting eventually in the release of calcium, thereby increasing the intracellular calciumconcentration. Alpha2 (α2) agonists act by inhibiting adenylyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cyclic adenosine monophosphate (cAMP). This leads to decreased intracellular cAMP levels.
Alpha receptors are further subdivided into α1A, α1B, α1C and α1D as well as α2A, α2B and α2C. This differentiation is important as the search for more selective newer drugs continues, and selectivity at the sub-type level helps narrow down the effects of a drug.
β-receptor stimulation: β agonists – selective to a subtype (β1, β2 and β3) or non-selective – stimulate adenylyl cyclase, causing increased intracellular cAMP levels.
Dopamine-receptor stimulation: Dopamine receptor agonists can act on D1 or D2 receptors. D1 receptors activate adenylyl cyclase and increase intracellular cAMP mainly in neurons and vascular smooth muscle. D2 receptors reduce intracellular cAMP and are found in the brain and as pre-synaptic receptors.
Indirect acting sympathomimetics
Indirect-acting drugs are those that act indirectly to increase the concentration of the endogenous neurotransmitter by causing its release (e.g., amphetamine derivatives and ephedrine) or inhibiting its reuptake (e.g., cocaine and tricyclic antidepressants).
Mixed-acting sympathomimetics
Mixed-acting drugs employ both mechanisms, e.g., ephedrine, which, in addition to acting on the α and β receptors, causes noradrenaline release.
Ephedrine is used to treat nasal congestion.
Effects on Various Organ Systems and Clinical Uses of Sympathomimetics
Sympathomimetics (α and β agonists) have varying effects on various organ systems.
The effects of sympathomimetics on various organ systems are summarized in the following table:
Cardiovascular effects of sympathomimetics
α and β agonists have significant effects on vascular systems. These effects are essential to understand and learn the cardiovascular pharmacology of α and β agonists/sympathomimetics.
It is interesting to mention the mechanism of action of clonidine. Other α agonists increase the blood pressure; however, clonidine is used in the treatment of hypertension (it decreases the BP). Clonidine acts on α adrenoceptors in the medulla of the brain. It is a centrally acting α2 agonist. It decreases the BP by decreasing peripheral vascular resistance, thus lowering blood pressure and reduces the release of catecholamine levels in the blood. It also decreases heart rate and cardiac output, though decreased blood return eventually results in reflex tachycardia.
Cardiovascular effects of sympathomimetics are summarized in the following table:
Other clinical uses of sympathomimetics
Epinephrine: anaphylaxis
Epinephrine is a mixed-acting agonist. It is the drug of choice for anaphylaxis and cardiac arrest. This is because it antagonizes the effects of many mediators of anaphylaxis. It counteracts hypotension through β1 receptor stimulation and causes bronchial muscle relaxation, thereby relieving bronchospasms through β2 receptor stimulation.
Toxicity of Sympathomimetics
Toxicities of sympathomimetic drugs are basically the extension of their physiologic effects of α or β receptor stimulation – excessive vasoconstriction, cardiac arrhythmias, myocardial infarction, stroke, pulmonary edema, pulmonary hemorrhage, etc.
Obviously, drugs that have more selective subtype affinity will have toxicities more related to stimulation of that subtype. For example, β1 agonists will cause tachycardia and arrhythmias, and toxicity of α1 agonists will manifest as hypertension.
Side Effects of Sympathomimetics
Common side effects of α agonists
- Headache
- Reflex bradycardia
- Excitability
- Restlessness
Common side effects of β agonists
- Cardiac arrhythmia
- Headache
- Tremors
- CNS effects of catecholamines are limited because of their low CNS penetration; however, higher doses can cause some CNS effect. CNS toxicity of phenylisopropylamine derivatives depends on the dosage. It can be mild to severe, ranging from nervousness and insomnia to anxiety and aggressiveness and even paranoid behavior and convulsions.
- As mentioned in the introduction, the selectivity is only relative, and, at high doses, other receptor types can be activated.
- An important interaction is observed between tyramine and MAOa inhibitors. Both of these drugs should be contraindicated as MAOa inhibitors as they increase the bioavailability, resulting in severe increase in blood pressure (hypertensive crisis).
Review Questions
The correct answers can be found below the references.
- A patient presents with chronic obstructive pulmonary disease (COPD), which is an obstructive airway disease that causes problems in breathing because of poor airflow. Which of the following types of drug would you preferably administer to this patient?
- Long-acting α2 receptor agonist
- Long-acting β1 receptor antagonist
- Short-acting β2 receptor agonist
- Long-acting β2 receptor agonist
- Short-acting α2 receptor agonist
- Which of the following drugs is the most useful for terminating an acute attack of asthma?
- Salmeterol
- Formoterol
- Olodaterol
- Clonidine
- Terbutaline
- Which of the following drugs would be the most appropriate to treat nasal congestion?
- Pseudoephedrine
- Xylometazoline
- Adrafinil
- Methyldopa
- Cocaine
Comentários
Enviar um comentário