Humoral Immunity and Cell-Mediated Immunity
Table of Contents
- Primary Immune Response
- Secondary Immune Response
- T-Dependent, T-Independent Antigens and Class Switching
- Structure of Antibodies and Immunoglobulin Domains
- Antibody Polymers and Antibody Binding to Antigens
- The Function of Antibodies
- Classes of Antibodies (Immunoglobulin)
- Autoimmune Disease
- Conclusion of Humoral Immunity and Cell-Mediated Immunity
- References
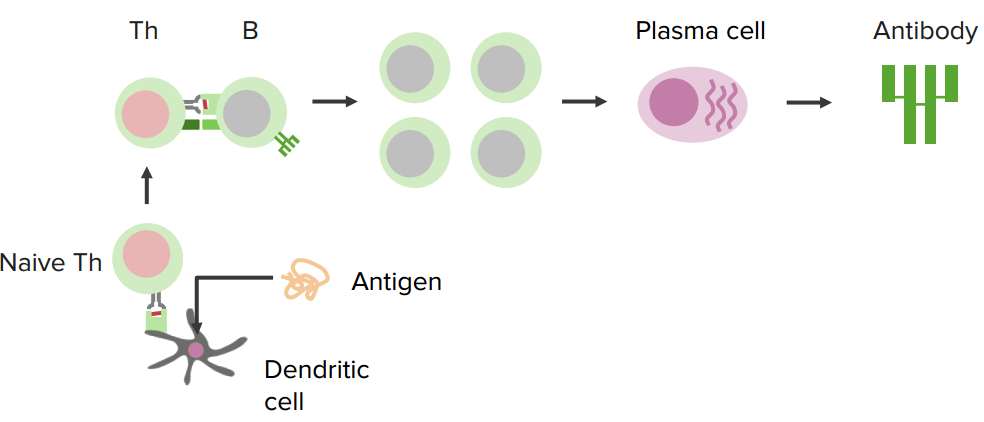
Image : “T helper cell” by
allinonemovie. License: CC 0
Primary Immune Response
This refers to the first encounter of the body-host with the antigen, in which naïve B cells activate and proliferate to induce an effective immune response against this antigen. The primary immune response is relatively slow in protecting against invasive pathogens, mostly because it induces the release of polyspecific, natural antibodies that have a low affinity, but they are used by the body in the initial protection against the pathogen.
Secondary Immune Response
The secondary immune response occurs as a result of the activation of certain types of cells, called “memory B-cells“. In contrast to the primary response, the secondary immune response is relatively faster and more effective in suppressing the infection progress, because of the increased antibody binding affinities. This is actually how the vaccines work. As vaccines induce the initial primary immune response, the body responds faster, and more effectively, upon re-exposure to the same antigen (secondary response) from which the vaccine was made.
The study of the molecular and cellular parts that present the type of this humoral system are the central science of this medical specialty, all together with their operations and interactions.
Humoral immunity refers to protein production, therefore the accent processes that accompany it include Th2 activation and protein production, germinal centre formation and isotope changing, affinity maturation and memory cell generation. Jointly, it refers to the effective functions of antibodies that embrace infectious agent and poisonous substance neutralization, classical complement activation, and antibody promotion of phagocytosis and infectious agent elimination.
T-Dependent, T-Independent Antigens and Class Switching
A B cell response area is classified as T-dependent (T-D) or T-independent (T-I) antigens which are supported for the necessity of lymphocyte facilitate in protein production.
The T-D antigen area unit protects that area unit, processes and gives on MHC category II molecules for recognition by its cognate T cells helper.
T-I antigens area units are divided into sort I and sort II. The previous area unit of the mutagenic stimuli like LPS, Chg., or poly-IC elicit polyclonal B lymphocyte activation via Toll-like receptors, whereas the latter area unit polysaccharides, have interaction with the B lymphocyte receptor and, therefore, induce antigen-specific B lymphocyte responses.
T-I sort II antigens cause strong and long primary protein responses. Sugar vaccines, like Menomonee confer, semi-permanent body substance, protects adults.
However, T-I sort II antigens do not cause a recall response, i.e. a lift in protein production upon secondary protection. Help from unsusceptible with T-I sort II antigens, will answer the secondary challenge once adoptively transferred into naïve, irradiated recipients, and the injection of immune bodily fluid into naïve recipients, before the adoptive transfer suppresses this response.
T-D antigens cause memory B cells which develop in T-D germinal centres, and might be known by physical mutations in their immune serum globulin loci, or by surface expression of secondary immune serum globulin isotopes.
T-I sort II antigens stimulate extrafollicular foci of lymph cell production and fugacious presumptively unsuccessful T-I germinal centres. It is not known whether or not T-I sort II immune responses can generate memory B cells. Terribly low levels of physical hypermutation and low frequency of shifts to secondary immune serum globulin isotopes through T-I sort II responses hinders the identification of T-I memory B cells and mistreat this criterion. It is widely accepted that memory B cells area units are derived solely from T-D responses.
Structure of Antibodies and Immunoglobulin Domains
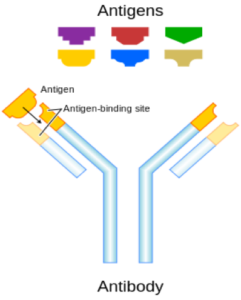
Image: “Each antibody binds to a specific antigen; an interaction similar to a lock and key.” by Fvasconcellos 19:03, 6 May 2007 (UTC) – Color version of Image:Antibody.png, originally a Work of the United States Government, License: Public Domain
Antibody molecules are square measured, roughly Y-shaped molecules, consisting of 3 equal-sized parts, loosely connected by a versatile tether. The schematic representations of the protein structure that have been determined by X-ray natural philosophy are square measured as shown in figure 1.
However, this structure was created, and it permits protein molecules to hold out their twin tasks, i.e. binding on the one hand to a good kind of antigens, and on the opposite hand to a restricted variety of effector molecules and cells.
Every task is disbursed by dissociable elements of the molecule. The both arms of the Y finish in regions that fluctuate between totally different protein molecules; the V regions. These square measures are concerned in matter binding, whereas the stem of the Y, or the C region, is way less variable and just the half interacts with effector cells and molecules.
The serious and light-weight chains of square measures are composed of a series of distinct super molecule domains. These super molecule domains have the same pleated structure.
Among these basic three-dimensional structures, there are distinct measure variations between V and C domains. The structural similarities and variations can be seen in the diagram of a lightweight chain.
Every domain is made from 2 β sheets, square measure parts of supermolecule structure, created of strands of the peptide chain (β strands) packed along; the sheets of square measure, joined by a type of disulphide bridge together, a roughly barrel-shaped structure, referred to as a β barrel.
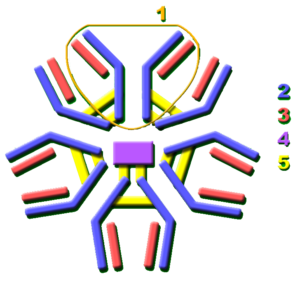
Image: “Secreted mammalian IgM. The higher panels show, schematically, the folding pattern of the constant (C) associated with degree variable (V) domains of a lightweight chain.” The original uploader was TimVickers at English Wikipedia – Transferred from en.wikipedia to Commons, License: CC BY-SA 3.0
Every domain can be a barrel-shaped structure with strands, and each one forms the essential similarity out of V and C domains, and the vital distinctionbetween them. The Square measure is most clearly seen in the bottom panels. Wherever the cylindrical domains square measure are opened, resolute reveals the peptide chain folds, and forms every part of the β sheets. They form versatile loopsbecause it changes direction. The distinction between the V and C domains is that the V domain is larger and with an additional loop.
Antibody Polymers and Antibody Binding to Antigens
The antigen-antibody reaction is widely used in laboratory diagnostics, including immunohematology. It is a reversible chemical reaction:
Antigen+antibody⇄antigen−antibody complex
The forces which connect the antigen-antibody are not sturdy valence bonds; however, weaker bonds are fittingly named “weak interactions”. The first vital issue is governing the behaviour of antibodies and it depends on the genetic system and how mature the response is (affinity maturation). The low-affinity antibody area unit is notably sensitive to substances, such as protein concentrations, and a substance called zygosity.
On the opposite hand, the high-affinity antibody area unit is sensitive to the serum/cell quantitative relation. The second most vital issue is the activity at low ionic strength: the Rh antibody area unit notably increases, and most alternative antibody area unit decreases, however, Kell antibodies are not increased in the slightest degree.
An appropriate technique for all clinically important red cell antibodies ought to meet a series of needs.
- Incubation at terribly low ionic strength (I=0.03–0.04) or within the presence of PEG.
- Period of incubation not but twenty minutes.
- The best serum/cell quantitative relation.
- The minimum quantity of red cells.
- Homozygous red cells.
In applying, volume limitation forces a compromise between low ionic strength and therefore, the quantity of serum/plasma. To succeed in ionic strength, 0.4 humour should be diluted to a minimum of 1:4 with a coffee ionic strength answer. Moreover, the minimum quantity of red cells depends on the detection system; tube tests need a lot of red cells than gel or solid part tests.
The Function of Antibodies
Activated B cells differentiate into either antibody-producing cells, referred to as plasma cells, or memory cells that survive in the body years later, for the system to recollect an Associate in Nursing substance and respond quicker to future exposures. At the antenatal and baby stages of life, the presence of antibodies is provided by passive protection from the mother. Early endogenous protein production varies from various sorts of antibodies, typically showing the primary years of life.
Since antibodies exist freely within the blood, they are said to be a part of the body substance system. The current antibody area unit is created by organism B cells that specifically reply to only one substance.
Antibodies contribute to immunity in 3 ways: preventing pathogens from coming into or damaging cells by binding to them, stimulatingly removing of pathogens by macrophages and alternative cells by coating the pathogen, and triggering the destruction of the offending pathogens by stimulating alternative immune responses like the complement pathway.
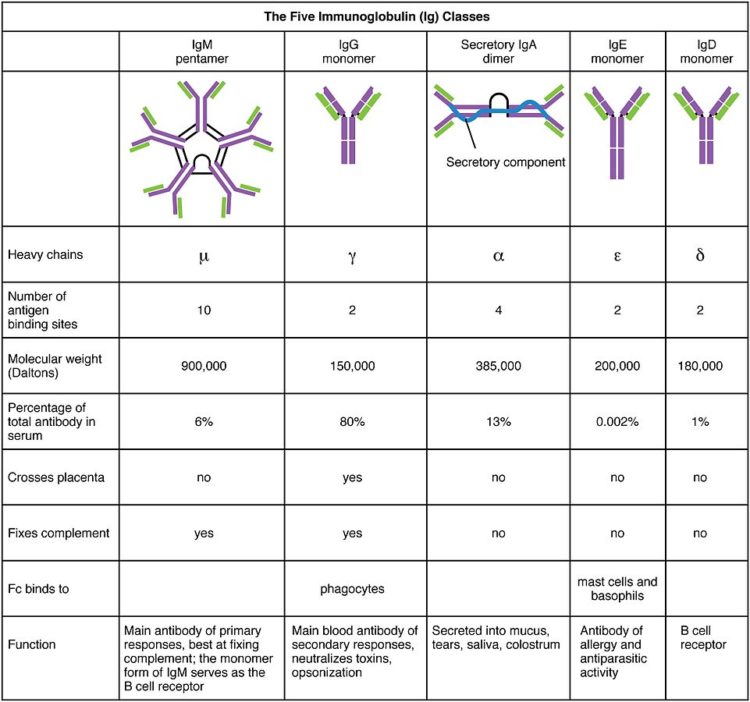
Classes of Antibodies (Immunoglobulin)
Autoimmune Disease
Autoimmune disease can affect the human immune system, so the primary goal is to create self-immunity. However, if a person’s body hasn’t developed an adequate human immune system, some autoimmune disease can appear, e.g. rheumatic fever, rheumatoid arthritis, ulcerative colitis, myasthenia gravis, Lyme disease, microbial etiology, Guillain-Barre syndrome, Reiter’s syndrome or reactive arthritis, or insulin dependent diabetes mellitus (IDDM) etc.
Conclusion of Humoral Immunity and Cell-Mediated Immunity
Antigens are any foreign substance that elicits an immune response when introduced into the tissues of a susceptible animal, and capable of combining with the specific antibodies formed.
They are generally of a high molecular weight. They are usually proteins or polysaccharides. One of the most familiar antigenic is microbes, which contain and produce many antigens. Antigens are consisted of many specific sites that connect and bind to antibodies called epitopes. Immunity and immune responses are consisted of two cellular systems: humoral or circulating antibody system (B cells) and cell-mediated immunity (T cells).
The immune system itself identifies antigens (unfamiliar proteins or polysaccharides) like its components of microbes, or likewise their partially degraded by-products and other unfamiliar proteins and polysaccharides, which includes nucleic acids. On the other hand, the host can be human or animal antigens and are not made by the individual, so it can result in a graft or transplant rejection etc.
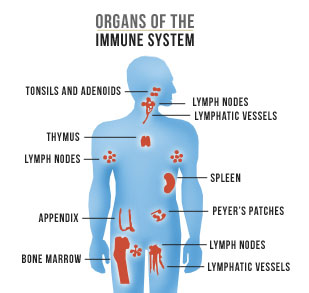
Image: “Organs of the human immune system” by AIDS.gov – https://www.aids.gov/hiv-aids-basics/just-diagnosed-with-hiv-aids/hiv-in-your-body/immune-system-101/, License: Public domain
The human immune system begins since birth, as it develops from the beginning (embryo stage) and starts with hematopoietic stem cells (Greek: “Blood making”). Those stem cells are developing and differentiating into bigger cells in the immune system (granulocytes, monocytes, and lymphocytes).
Stem cells differentiate throughout human life and they can also differentiate into cells in the blood which are not involved in the human immune function (erythrocytes and megakaryocytes).
Humoral Immune Responses to antigens begin by exposing the human immune system to antigen. While exposing to antigen “A” for the first time, the immune system begins to make low levels of antibody, approximately in a week. During the second exposure to the antigen “A”, the human immune system produces a much faster response, several orders of magnitude higher levels of antibody, and the ability of these antibodies to bind, the antigen increases dramatically during the secondary response to the exposure.
Whilst injecting a new antigen “B” with “A” can only elicit a primary response, and it shows that memory or prior exposure is required for a fast response.
The role of selection of new microbial strains in susceptibility to infection and illness
Antigenic changes in microbes can overcome immunity, which increases the risks of re-infection or illness. Antigenically different strains of microbes appear and are selected for over time and space. The constant selections of new strains are selected by antigenic shift and drift. It is partly driven by “herd” immunity and genetic recombination, re-assortment, bacterial conjugation, bacteriophage infection, and point mutations.
The difference between antigenic shift and antigenic drift
The antigenic shift is a bigger change in virus genetic composition by gene substitution or replacement (e.g., re-assortment).
The antigenic drift is small changes in the virus genetic composition, often by a mutation involving specific codons in existing genes like point mutations.
Comentários
Enviar um comentário