Upper Respiratory Tract Infection (URI, URTI) — Symptoms and Treatment
Table of Contents
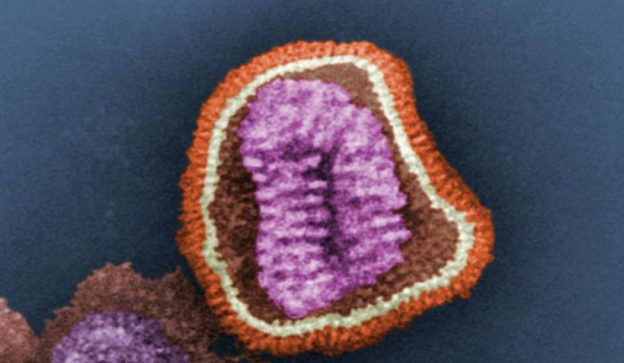
Image: “This (pseudocolored) negative-stained (false-colored) transmission electron micrograph (TEM) depicts the ultrastructural details of an influenza virus particle, or “virion”.” by Photo Credit: Cynthia Goldsmith Content Providers(s): CDC/ Dr. Erskine. L. Palmer; Dr. M. L. Martin – This media comes from the Centers for Disease Control and Prevention’s Public Health Image Library (PHIL), with identification number #10073. License: Public Domain
Definition of Upper Respiratory Tract Infection
Rhinitis can be defined as the inflammation of the nasal mucosa, which is found in some allergic conditions. Patients with sinusitis have inflammation of the paranasal sinuses which include the frontal, ethmoid, maxillary and sphenoid sinuses.
Rhinopharyngitis is the inflammation of the nasal passages, the pharynx, and the tonsils. The common cold usually results in rhinopharyngitis. Patients with epiglottitis can have bacterial etiology and the condition might be life-threatening.
Epidemiology of URIs
URIs are considered as the most common infectious diseases in the population. Patients can develop the common cold up to four times per year for adults, and eight times per year for children. Viral and bacterial pharyngitis are common in children and account for 1% of the outpatient clinic visits.
Image: “Acute epiglottitis; lateral view in X-ray imaging. The lateral soft-tissue radiograph reveals the “thumb sign” that indicates a swollen epiglottis, suggestive of epiglottitis. The diagnosis was confirmed on subsequent imaging and laryngoscopy. The patient recovered following treatment with predonine and ceftriaxone.” by Med Chaos – Own work. License: CC0 1.0
Sinusitis in patients with uncomplicated URIs is common and can be identified in up to 80% of the cases. Fortunately, bacterial sinusitis is only found in 2% of the cases.
Epiglottitis is usually caused by Haemophilus influenzae infectionand since the introduction of Hib vaccine, the incidence of epiglottitis decreased significantly. The current incidence of acute epiglottitis is estimated to be about 0.98 cases per 100,000. Pneumococcal epiglottitis is responsible for 0.28 cases of epiglottitis per 100,000.
Croup or laryngotracheobronchitis is common in children aged 6 months to 6 years. Most cases of croup occur in children aged two years. Fortunately, despite the harsh breathing sounds, the condition is self-limiting.
Pertussis is responsible for a whooping cough, another URI that has significantly decreased after the introduction of pertussis vaccination. The current incidence of a whooping cough due to pertussis is estimated to be 9 per 100,000.
URIs are usually seasonal and most cases occur in fall or winter. It is hypothesized that cold weather increases indoor time and therefore puts us at prolonged exposure with those already infected.
Additionally, low humidity in winter is thought to be a significant factor in the thrive and increased the virulence of the different viruses implicated with URIs.
The common cold appears to be more common in young women. Epiglottitis, on the other hand, is more common in men. Croup, for obscure reasons, is more common in boys rather than girls.
Classification of URIs
Some author called the term URTI as a misnomer as most of the patients with URTI has the symptoms of LRTI or most of the cases also has lower respiratory tract infection.
Etiologies of URIs
URIs can be caused by several viral and bacterial pathogens. The most commonly implicated viruses with URIs are rhinoviruses, coronaviruses, adenoviruses, and coxsackieviruses.
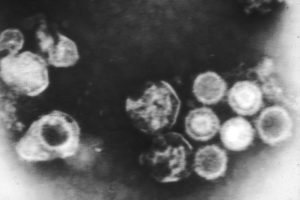
Image: “Epstein-Barr virus taken through an electron microscope.” by Linda Bartlett (Photographer) – This image was released by the National Cancer Institute, an agency part of the National Institutes of Health, with the ID 2105. License: Public Domain
The common cold is usually related to the rhinoviruses while coronaviruses can also account for a significant number of the cases. Adenovirusescan also cause nasopharyngitis.
Pharyngitis is usually caused by viruses by the recognition of group A streptococcus. Common viruses that are implicated with pharyngitis include adenovirus, the influenza viruses, and Epstein-Barr virus.
Group A streptococcal infection is responsible for up to 15% of the cases of pharyngitis in adults and 30% in children. Therefore, the early recognition of bacterial streptococcal pharyngitis is essential to prevent complications.
Patients with rhinosinusitis usually have another viral URI such as rhinovirus, coronavirus, or influenza A or B infection. These patients can have signs of sinusitis on computed tomography, which usually goes without any complications.
Secondary bacterial infection, however, can happen in few cases. Common organisms are Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis and Staphylococcus aureus.
Epiglottitis has been historically linked to Haemophilus influenzae but since the introduction of the Hib vaccine, the incidence of acute epiglottitis decreased dramatically. On the other hand, cases of streptococcus epiglottitis are becoming more commonly identified nowadays.
Croup can be caused by parainfluenza viruses types 1, 2 and 3. In few children, the cause is the influenza viruses.
Pathophysiology of URIs
Patients need to come in contact with an infected person or with inanimate objects that have been contaminated with the infecting organism. Once the person’s hand becomes contaminated with the potential pathogen, he or she can introduce the organism to him/herself when they touch the nose or the mouth. Viral or bacterial inoculation happens which is followed by the invasion of the mucosa lining the upper respiratory airway.
In addition to the virulence of the infecting organism, the person’s genetic susceptibility also plays a role in determining who is more likely to get sick once in contact with someone with URIs. Certain polymorphisms related to the immune system put the patient at an increased risk of developing severe influenza illness once exposed to the H1N1 or the H5N1 influenza viruses.
Details of Different URIs
Common Cold
The common cold is the commonest URTI mostly caused by viruses and is very contagious.
Causative organisms
- Influenza viruses
- Picornaviruses like (Coxsackie, Reo, Echo, and rhinovirus)
- Respiratory Syncytial Virus
- Parainfluenza virus
- Adenovirus
Pathogenesis
The virus invades the nasal mucosa causing an immediate irritative reaction resulting in the secretion of large quantities of mucous and cells. Within 24 hours a secondary infection can intervene converting watery nasal discharge to purulent form.
Sign and Symptoms
- Sneezing
- Rhinorrhoea
- Nasal congestion
- Sore throat
- Non-productive cough
- Pain in the eyes
- Headache
- Malaise and Myalgia
- Fever is uncommon but some patient can get fever
- Conjunctivitis can occur in adenovirus infection
- Some time it present with skin rash with enterovirus infection
On examination, post-nasal discharge, erythema around the nose and glossy nasal mucosa may be found, the pharynx shows congestion with some form of exudates. Exudates can also be present on tonsils. Jugulo-gastric lymph node may be enlarged and tender in some patients.
Complications
- Sinusitis
- Otitis media
- Croup
- Secondary bacterial pneumonia
Laboratory Investigation
Real-time polymerase chain reaction (RT-PCR) or isolation of the virus in culture or four-fold increase in virus-specific circulating antibodies are used for confirmation of the diagnosis. The clinical specimen used for this purpose are nasopharyngeal swab, nasal swab, pharyngeal swab and aspirate in case of intubated patients.
Treatment
Common cold usually treated empirically. The mainstay of treatment is symptomatic and supportive treatment. Bed rest adequate fluid, anticholinergic nasal spray, saline nasal drops, nasal decongestants like xylometazoline and oxymetazoline are used for symptomatic relief.
Pharyngitis
Definition and pathogenesis
Pharyngitis is defined as the inflammation of the pharynx, hypopharynx, uvula, and tonsils. It is usually of infectious etiology and the majority of causes are the viral origin. A beta-haemolytic streptococcus is common in children aged 4 to 7 years. persons with oro-genital contact, gonococcal pharyngitis can occur. Oral thrush involving pharynx can occur in the immunocompromised patient.
Sign and symptoms
- Throat discomfort
- Odynophagia
- Cough
- Constitutional symptoms like body ache, fever, myalgia, and malaise
Differential diagnosis
Epiglottitis, laryngitis, laryngotracheitis and peri-tonsillar abscess.
Laboratory diagnosis
- Throat swab Culture and serological testing
- Identification of beta-haemolytic streptococci by this method is of paramount importance as it is associated with the development of rheumatic heart disease
Complications
Treatment
The mainstay of treatment is symptomatic and supportive treatment. Some patient may require antibiotic for secondary bacterial infection or infection with beta hemolytic streptococci. Viral pharyngitis is self-limiting and resolves spontaneously. However, the clinician should be aware of a potential complication.
Epiglottitis
It is the infection of the epiglottis. Mostly it is a viral infection but sometime it may be of bacterial origin.
Epidemiology
- It can occur at any age
- Hemophilus influenza type B is mostly associated with Epiglottitis but current trend shows the rising trend of infection with beta haemolytic streptococci after mass vaccination against influenza virus
- The incidence of acute epiglottitis in adults ranges from 0.97 to 3.1 per 100,000, with a mortality of approximately 7.1%
- There is no seasonal variation in the incidence of epiglottitis
Sign and symptoms
- Throat discomfort
- Odynophagia
- Cough
- Difficulty in swallowing with sitting up and leaning forward position
- Constitutional symptoms like body-ache, fever, myalgia, and malaise
- Dysphagia, drooling, and stridor subsequent to thermal or caustic injury to epiglottis
Differential Diagnosis
- Croup
- Foreign body in airway
- Bacterial tracheitis
- Retropharyngeal abscess
Laboratory diagnosis
- Antero-posterior radiographs of the neck are helpful in confirming the diagnosis and helps in ruling out the presence of the foreign body
- “Thumb sign” in radiograph is indicative of sever acute epiglottitis
- Laboratory tests are usually not helpful
- Performing a flexible fiber optic laryngoscopy in a controlled clinical setting is reliable
- Ultrasonography has been described as a way to investigate the epiglottis by visualization of the “alphabet P sign” in a longitudinal view through the thyrohyoid membrane
Complication
- Death from asphyxia
- Secondary bacterial infection
- Pneumonia
Treatment
- Viral epiglottitis is self-limiting and require only supportive treatment
- Patients with secondary bacterial infection or with complication or epiglottitis of bacterial origin may require antibiotics. Broad-spectrum antibiotics like chloramphenicol or co-amoxiclav are the antibiotic of choice
Rhinitis
Definition
It is defined as the inflammation of the membranes lining the nose and it is characterized by nasal congestion, rhinorrhoea, sneezing, itching, conjunctival symptoms and other constitutional symptoms.
Classification
Rhinitis can be classified according to its etiology i.e. allergic or non-allergic
Pathogenesis
Allergic rhinitis is due to inflammation in the nose which is immunoglobulin specifically IgE mediated. It is mostly due to acute exposure to inciting allergens. Non-allergic rhinitis pathogenesis varies according to their etiology but the main pathogenesis lies in the inflammation of nasal mucosa.
Signs and symptoms
- Nasal congestion
- Rhinorrhoea
- Sneezing
- Itching
- Conjunctival symptoms
- Other constitutional symptoms like fever, malaise etc.
Diagnosis
Identification of etiological cause is based on the pattern, chronicity and seasonal variation of symptoms, history of medication, the presence of co-existing conditions, occupational exposures, environmental history and identification of precipitating factors.
Physical examination should also focus on the identifying surgically correctable condition like deviated nasal septum, polyps or enlarged turbinate. Allergen skin test or in-vitro testing is useful in detecting allergic rhinitis.
Treatment
- Antihistaminic mostly nonsedating oral or intra-nasal antihistaminics like loratadine, cetirizine, fexofenadine, etc.
- Antileukotrine
- Combination of antihistaminic and Antileukotrine
- Topical corticosteroids like mometasone, furoate, beclomethasone
- Avoidance of inciting allergens
- Anticholinergic drugs like ipratropium bromide
- Nasal decongestant like xylometazoline or oxymetazoline
- Oral corticosteroids and allergen immunotherapy may help in some cases
Sinusitis
Sinusitis is the inflammation of the paranasal sinuses. Moreover, with every URTI, there is an acute inflammation of sinus membranes.
There are many factors that predispose to development of sinusitis:
- Anatomic abnormalities like deviated nasal septum, concha bulosa, and bony spurs
- Allergic rhinitis
- Vasomotor rhinitis
- Rhinitis medicaments
- Cocaine abuse
- Nasal polyp
- Tumour causing obstruction
- Recurrent URTI
- Immune deficiency syndrome
- Cystic fibrosis
- Katargener’s syndrome
- Environmental pollution
Signs and symptoms
- Nasal congestion
- Mucopurulent or purulent nasal discharge
- Headache
- Facial pain or heaviness which increases with bending forward
- Fever
- Localized tenderness indicates infection of group of sinuses
- On examination, nasal mucosa looks oedematous
Laboratory investigations
- Smear examination of nasal secretion with giemsa’s stain or Wright’s stain shows 10% of eosinophil in allergic sinusitis.
- In sinusitis with infectious origin, eosinophilia is absent
- Nasal endoscopy
- X-ray of paranasal sinus (Occipito-mental view or Water’s view and Submental view)
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
Treatment
- NSAIDs for fever and pain relief
- Appropriate antibiotic for infectious etiology
- Nasal saline spray
- Topical decongestants like xylometazoline or oxymetazoline
- Steroids like fluticasone, beclomethasone
- Cromolyn sodium for symptomatic relief
- Surgery is indicated for chronic sinusitis refractory to medical therapy, recurrent sinusitis, large obstructing popyp, suspicion of the tumor, sinus mucocele, pyocele, intracranial extension, cavernous sinus thrombosis and fungal sinusitis.
- Surgical procedure adopted are Functional Endoscopic Sinus surgery (FESS) and Caldwell-Lue operation
Influenza
Definition:
Influenza is an acute respiratory illness caused by infection with influenza viruses. This disease affects the upper or the lower respiratory tract and it’s usually associated with systemic manifestations such as fever, headache, myalgia, and weakness.
Etiology
Influenza viruses are members of the Orthomyxoviridae family, of which influenza A, B, and C viruses constitute three separate genera.The designation of influenza viruses as type A, B, or C is based on antigenic characteristics of the nucleoprotein (NP) and matrix (M) protein antigens.
Influenza A viruses are further subdivided (subtyped) on the basis of the surface hemagglutinin (H) and neuraminidase (N)antigens. Influenza A has 18 distinct H subtypes and 11 distinct N subtypes, of which only H1, H2, H3, N1, and N2 have been associated with epidemics of disease in humans.
Influenza B and C viruses are designated similarly to influenza A viruses, but H and N antigens from these viruses do not receive subtype designations.
Epidemiology
Influenza outbreaks occur virtually every year, although their extent and severity vary widely. Global pandemics have occurred at variable intervals, but much less frequently than interpandemic outbreaks. The most recent pandemicemerged in March of 2009 and were caused by an influenza A/H1N1 virus that rapidly spread worldwide over the next several months. The most extensive and severe outbreaks of influenza arecaused by influenza A viruses, in part because of the remarkable propensityof the H and N antigens of these viruses to undergo periodicantigenic variation.
Pathogenesis
The initial event in influenza is infection of the respiratory epithelium with influenza virus acquired from respiratory secretions of acutely infected individuals. In all likelihood, the virus is transmitted via aerosols generated by coughs and sneezes, although transmission through hand-to-hand contact, other personal contact, and even fomites may take place.Experimental evidence suggests that infection by a small particle aerosol (particle diameter <10 μm) is more efficient than larger droplets.
Initially, viral infection involves the ciliated columnar epithelial cells, but it may also involve other respiratory tract cells, including alveolar cells, mucous gland cells, and macrophages.In experimentally induced infection, the incubation period of illness has ranged from 18 to 72 h, depending on the size of the viral inoculum.
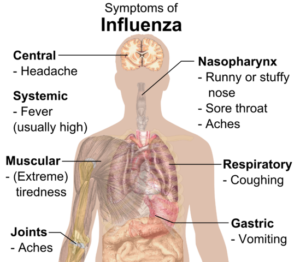
Signs and symptoms
- Fever
- Headache
- Chills with rigor
- Myalgia and malaise
- Cough
- Sore throat
However, the spectrum of clinical presentations is wide, rangingfrom a mild, afebrile respiratory illness similar to the common cold(with either a gradual or an abrupt onset) to severe prostration withrelatively few respiratory signs and symptoms.
Physical findings are usually minimal in uncomplicated influenza. Early in the illness, the patient appears flushed, and the skin is hot and dry, although diaphoresis and mottled extremities are sometimes evident, particularly in older patients. Examination of the pharynx may yield surprisingly unremarkable results despite a severe sore throat, but injection of the mucous membranes and postnasal discharge are apparent in some cases.In uncomplicated influenza, the acute illness generally resolves over 2—5 days, and most patients have largely recovered in 1 week, although a cough may persist 1—2 weeks longer.
Complications
- Primary influenza viral pneumonia
- Secondary bacterial pneumonia
- Mixed viral and bacterial pneumonia
- Myositis, rhabdomyolysis and myoglobinuria
- Myocarditis and pericarditis
- Encephalitis and transverse myelitis
- Reye’s syndrome
- Toxic shock syndrome
Laboratory diagnosis
- Throat swab, noso-pharyngeal swab, or washes or sputum culture
- RTPCR is most sensitive and specific
- Rapid diagnostic test
- Tissue culture
- Serological test
Differential diagnosis
- Mycoplasma pneumonia
- Streptococcal pharyngitis
- Early bacterial pneumonia
Treatment
Specific antiviral therapy is available for influenza: the neuraminidase inhibitors zanamivir
and oseltamivir for both influenza A and influenza B and the adamantane agents amantadine and rimantadine for influenza A. (1—6)
Clinical Presentation of URIs
The symptoms of Influenza, other URIs and allergies can overlap. Patients with the common cold usually develop it within 2 to 3 days after exposure and include rhinorrhea, nasal congestion, and sneezing. Patients can also complain from a sore throat and painful swallowing. A cough can be a symptom in some cases. Patients might develop a fever for a day or two.
Image: “Main symptoms of influenza.” by Mikael Häggström. License: Public Domain
Patients with influenza virus infection develop body aches, high fever, severe sore throat, andheadaches. Patients with severe or progressive pharyngitis might have streptococcal pharyngitis.
Patients with bacterial pharyngitis might have a low-grade fever. Children can develop a skin rash. Unfortunately, history taking alone is usually not sufficient to exclude streptococcal pharyngitis.
The presence of anterior cervical lymphadenopathy is not characteristic of bacterial infection. The presence of tonsils exudates, tender anterior cervical lymph nodes and the absence of conjunctivitis, cough, and rhinorrhea are suggestive of bacterial rather than viral pharyngitis.
Patients with bacterial sinusitis can develop persistent nasal discharge for more than 10 days, worsening of their cough and fever, or develop a severe cough and fever from the start for three consecutive days.
Patients with epiglottitis usually complain of a sore throat, muffled sound, fever, drooling and can present the tripod position.
Diagnostic Workup in URIs
The identification of the exact infecting organism should be attempted only when specific treatment can be provided or in the immunocompromised patient. Rapid tests are available for the detection of influenza and parainfluenza viruses. Viral cultures are the standard criterion for the identification of the viral etiology of the URI but the results are usually available too late to alter the medical treatment, two to four weeks.
Complete blood count is helpful in excluding possible bacterial infections which are characterized by neutrophilia. Unfortunately, leukocytosis is rarely seen in URIs and complete blood count is usually not helpful in most cases.
Patients presenting with symptoms consistent with the common cold should not be offered routine imaging studies. Patients presenting with high fever, tender neck examination and signs suggestive of peritonsillar abscess need specific imaging studies including x-rays.
Patients with suspected group A streptococcal infection should undergo throat swab testingfor group A streptococcus detection by rapid antigen testing, culture or both. Positive rapid antigen detection testing for group A streptococcus is highly specific and warrants specific treatment.
On the other hand, negative results should be backed up by a negative throat swab culture. Routine testing for streptococcal antibodies including the antistreptolysin O antibody is not helpful in the identification of acute infection because these antibodies usually peak 5 weeks after the infection.
Patients with suspected bacterial sinusitis should undergo computed tomography imaging of the sinuses. Computed tomography imaging should be preserved only for bacterial cases because it can be positive in up to 80% of the cases of uncomplicated rhinosinusitis.
Pertussis is usually a clinical diagnosis. Rapid direct fluorescent antibody testing can be used to confirm the diagnosis if needed. Patients with possible epiglottitis should undergo neck x-ray which is usually enough to exclude the diagnosis.
Treatment of URIs
Treatment of URIs is usually symptomatic but can be sometimes specific to the exact etiology or disease process.
Treatment of the common cold
Patients with symptoms consistent with uncomplicated common cold should drink plenty of water, might benefit from steamy baths and can use nasal decongestants for a limited period of time. Nonsteroidal anti-inflammatory drugs can be used to alleviate pain and inflammation. No specific antiviral treatment is usually indicated.
Treatment of influenza
Antiviral therapy can be helpful early in the disease as it was found to decrease the duration and the severity of the illness. Additionally, annual influenza vaccination not only decreases the risk of developing influenza during the season but also decreases the severity of the symptoms if one acquires the infection. Nonsteroidal anti-inflammatory drugs, drinking plenty of water and decongestants are also helpful.
Treatment of Rhinosinusitis
Image: “3D structure of amoxicillin.” License: Public Domain
Symptomatic treatment of viral rhinosinusitis is usually sufficient. Patients with suspected bacterial sinusitis should receive high-dose amoxicillin/clavulanate as first line therapy. Patients allergic to penicillins can receive doxycycline or levofloxacin. Patients who are not responsive to initial antibiotic treatment should undergo culture and sensitivity testing to confirm the infecting organism and its resistance profile.
Treatment of croup
Inhaled corticosteroids in addition to intravenous steroids are helpful in alleviating the symptoms of croup. Additionally, fluid replacement therapy should be started in children to avoid dehydration. Inhaled racemic epinephrine can also provide symptomatic relief.
Treatment of epiglottitis
Intravenous administration of antibiotics is indicated and should be started before the availability of the culture results. Ceftriaxone and cefuroxime are common first-line therapies for epiglottitis. Close contacts of the patient should also receive prophylactic antibiotic therapy.
Treatment of group A streptococcus pharyngitis
Group A streptococcus is sensitive to amoxicillin and penicillin. Therefore, oral administration of one of these two antibiotics is usually sufficient. Patients with non-anaphylactic shock to penicillins can receive a first generation cephalosporin. Patients with severe allergies should receive clindamycin, azithromycin or clarithromycin.


Comentários
Enviar um comentário