Anatomy of the Oral Cavity and Gastrointestinal Tract
Table of Contents
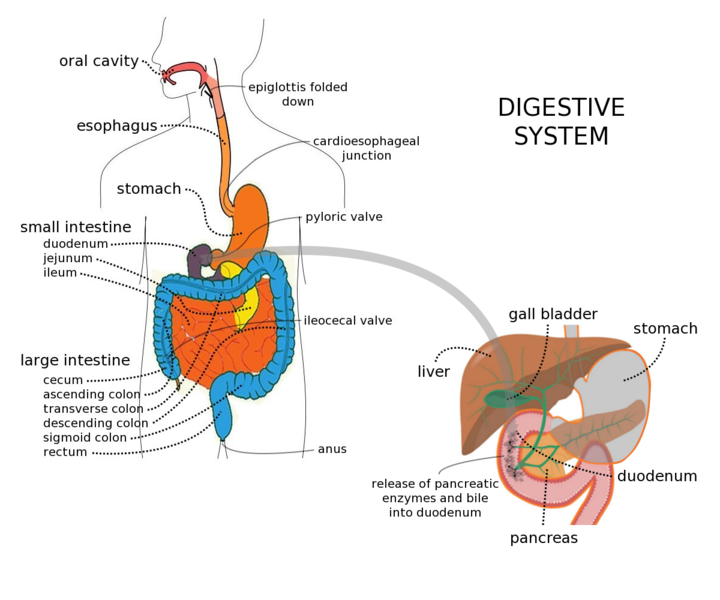
Picture: “Digestive System with Liver” by Gordon Flynn. License: CC BY-SA 2.5
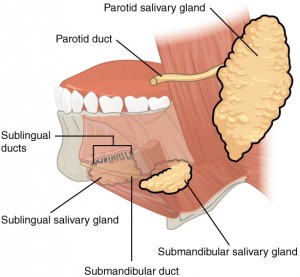
Structure and Secretion of the Salivary Gland
The swallowing process is movement of food from the mouth to the stomach. Before this happens, saliva is secreted by the salivary glands into the oral cavity.
Saliva consists of 99.5 % water and 0.5 % dissolved substances such as sodium, potassium, and bicarbonate. The main function of the secretion of saliva is to lubricate food as well as to start the chemical digestion of carbohydrates and lipids.
The autonomic nervous system controls the secretion of saliva in the oral cavity, throat and the esophagus. The daily amount of secretion by the salivary glands results in 1,000 – 1,500 ml of saliva is secreted by salivary glands every day.
There are numerous salivary glands in and around the oral cavity
A distinction is made:
Minor salivary glands
- Glandulae labiales in the lips’ mucosa
- Glandulae buccales in the cheeks’ mucosa
- Glandulae palatinae in the pharyngeal mucosa
- Glandualae linguales
Major salivary glands
- Glandula parotideae (parotid gland, below and in front of each ear)
- Glandula submandibularis (submandibular gland, lower jaw)
- Glandula sublingualis (sublingual gland)
The minor salivary glands secrete saliva through short ducts directly or indirectly into the oral cavity. Their contribution to the total saliva is small.
The major salivary glands lead directly into the oral cavity, secrete the most amount of saliva, and consist of three pairs of major salivary glands.
Glandula Parotideae (parotid gland)
These glands are located inferior and anterior to the ears, they cover the M. masseter, cranially touch the Arcus zygomaticus, and the Meatus acusticus externus in a dorsal direction. The biggest part of the gland lies deep in the Fossa retromandibularis. The glands secrete saliva through the Ductus parotideus (ear saliva duct), which extends through the M. buccinators and ends in the vestibule opposite to the second upper molar tooth.
The parotid glands solely consist of serous acini (parts of the glands that secrete serous fluid). Saliva is highly fluid and comprises of many proteins and enzymes. It contains immunoglobulins, which are secreted as a complex of immunoglobulins by the gland cells. They act as an immunological defence against germs within the oral cavity.
Glandula Submandibularis (submandibular gland)
At the bottom of the mouth, we find the submandibular gland, which is located in a canal between the inner side of the mandible, M. mylohyoideus, M. hyoglossus, and Lamina superficialis fasciae cervicalis.
Its ducts lie on both sides of the midline beneath the Mucosa (Ductus submandibularis) and reach the oral cavity next to the lingual frenulum. The submandibular gland mainly consists of serous acini and a few mucosal acini (parts of the gland that secrete mucus).
Glandula Sublingualis (sublingual gland)
The sublingual gland lies lateral to the M. genioglossus on the M. mylohyoideus and above the submandibular glands. Its small ducts (Ductus sublinguales minores) empty into the bottom of the mouth directly into the oral cavity. It mainly consists of mucosal acini and just a few serous acini.
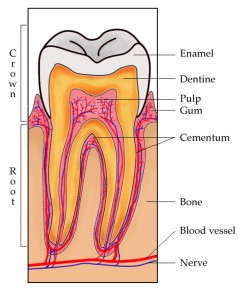
Structure of the Teeth
Teeth (dentes) are included in the accessory digestive organs, they lie in the caves of the alveolar extensions in the upper and lower jaw.
The alveolar extensions are covered by the (gingiva) that slightly reaches into every hole. On the inner side of these holes, there is the periodontal ligament (peridontium), which consists of connective tissue fibers that holding the teeth in place.
A tooth consists of three main parts:
- crown
- roots
- neck
The visible part that lies above the gingival is called the crown. One or three roots are invisibly located inside the holes. The constricted connection between crown and roots is called the neck.
Picture: “Tooth Section” by Sam Fentress. License: CC BY-SA 2.0
The main inner part of a tooth is called the dentin and consists of calcified connective tissue that is responsible for tooth’s form and consistency.
At the crown, the dentin is covered by enamel (substantia adamantinea), which consists of calcium phosphate and calcium carbonate. Due to its high concentration of calcium, enamel is harder than bones, making it the hardest substance in the body.
The main function of enamel is to protect teeth against wear from chewing and against acidswhich could dissolve the dentin. The dental cement is connected to the periodontal ligament and covers the dentin at the roots.
The dentin encompasses a defined range of each tooth. The pulp cavity is the part of the enlarged space inside the crown, which is filled with dental pulp. The dental pulp contains blood vessels, nerves, and lymph vessels.
The root canals are small expansions of the pulp cavity that traverse the root of a tooth and hold a hole at its bottom—the apical foramen—where nerves, blood, and lymph vessels are attached.
Over the course of their lives, humans have two dentitions, the primary dentition, and the permanent dentition. The first milk teeth (dentes decidui) bursts through after 6 months. Each month of a baby’s life, one or two more teeth appear until all 20 teeth are in place. Generally, all milk teeth shed between the age of 6 and 12 after which they are then replaced by the permanent dentition.
The permanent dentition (dentes permanentes) consist of 32 teeth, 16 in the upper jaw and 16 in the lower jaw respectively. Each half of the jaw contains 3 molars, 2 bicuspids, 1 canine, and 2 incisors.
The first molars (16, 26, 36, 46) burst through at the age of six years, the second molars at the age of twelve, and the so-called wisdom teeth (third molars) after the age of 17. Their function is to crunch and grind up food.
In many cases, the human jaw does not provide enough space behind the second molars to allow the wisdom teeth to burst through. When this occurs, the third molars remain embedded in the alveolar bone. Sometimes, this causes pressure and pain to the extent that they have to be surgically removed. Some people experience that the third molars atrophy or do not develop at all.
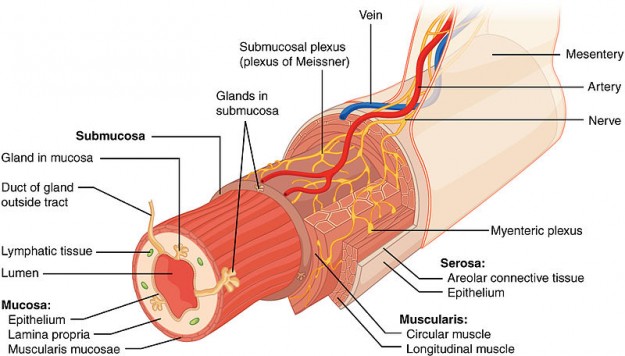
The Layers of the GI Tract
The wall of the GI tract consists of four layers each constructed in the same basic order—from the lower esophagus to the anus.
From the luminal surface to the outer surface, four layers can be distinguished:
- Mucosa
- Submucosa
- Muscularis
- Serosa
The mucosa is the innermost layer of the GI tract and it is a mucous membrane consisting of an epithelial layer, a thin layer of connective tissue, and another thin layer consisting of smooth muscle cells.
The epithelial layer serves as a protective layer and with the help of the single-layered columnar epithelium, it contributes to secretion and resorption. Additionally, exocrine cells are located between the epithelial cells, which secrete mucus and liquid into the lumen (the inner space of a cavity) of the GI tract.
The submucosa or lamina propria (lat. lamina = thin, flat layer; propria = own) contains many blood and lymph vessels. The lamina propria enables nutrients which are reabsorbed in the GI tract to reach other parts of the body. They also contain the majority of cells of the mucosa-associated lymphoid tissue (MALT), which in turn contain cells of the immune system that help protect the body from diseases.
The muscularis mucosae is a thin layer of smooth muscle fibres that enlarges the surface for better digestion and resorption and further ensures that all reabsorbing cells get in contact with the substances in the GI tract.
The submucosa consists of loose reticular fibres which strike through numerous fenestrations (areolar connective tissue) and connect the mucosa to the muscularis. Its structure comprises of many blood and lymph vessels which contain absorbable food molecules. The special feature of the submucosa is the included Meissner’s plexus, a vast network of neurons. It can also contain glands and lymphoid tissue.
The muscularis of the GI tract consists of skeletal muscles as well as smooth muscle fibres. The arbitrary swallowing is generated by the muscularis of the mouth, the pharynx, and the upper and middle part of the esophagus. On the other hand, the deliberate control of defecation is possible due to the skeletal muscles found at the outer anal sphincter.
The smooth muscles are located in the rest of the GI tract and are characterized by an inner layer of circular fibres and an outer layer of longitudinal fibres. They help to degrade food, mix up digestive secretions, as well as move food along the tract. The second plexus of neurons, the so-called Auerbach’s plexus, is located between the layers of the muscularis.
The serosa or surface layer is a serous membrane of areolar connective tissue and single-layered squamous epithelium. The surface layer of the esophagus is comprised of just one single layer of areolar connective tissue (adventitia) with the absence of a serosa.
Specifics of the Wall Structure of the Esophagus, Small Intestine and Large Intestine
Esophagus:
The esophagus has the same wall structure as all the other segments of the GI tract.
The mucosa (mucous membrane) of the esophagus consists of non-keratinized multi-layered squamous epithelium, lamina propria, and a muscularis mucosa (smooth muscle), which is responsible for the onward movement of food (peristalsis) to the stomach.
The muscularis consists of fasciated skeletal muscles (voluntary muscles) in the upper third, whereas the lower third consists entirely of smooth muscles. In between are voluntary as well as smooth muscle cells.
Small intestine:
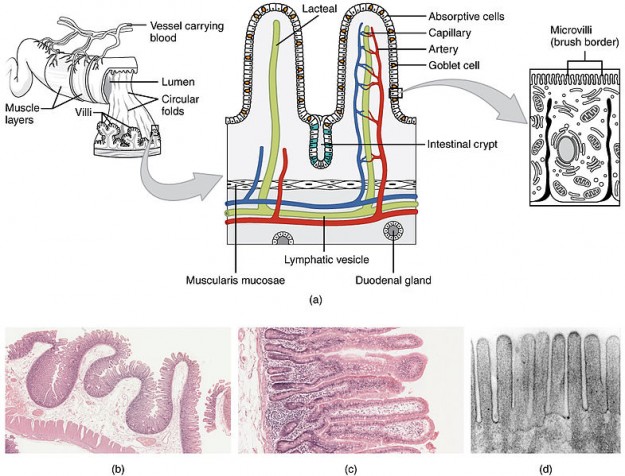
The small intestine is organized in 3 parts, namely the duodenum, jejunum, and ileum. The wall of the small intestine also consists of the same four layers as the larger part of the GI tract. However, the small intestine has some specifics.
The epithelial layer of the small intestine’s mucosa is built of single-layered cylindrical epithelium, which contains many different cell types, e.g.
- Resorption cells: responsible for digesting and reabsorbing nutrients in the bolus
- Goblet cells: responsible for secreting mucus
The small intestine mucosa contains many deep fissures.
Intestinal glands (crypt of Lieberkühn) are the cells furnishing the fissures and secreting the intestinal juice. Apart from resorption and goblet cells, intestinal glands contain Paneth cellsand enteroendocrine cells.
The submucosa of the duodenum contains Brunner’s glands that secrete alkaline mucus to neutralize the stomach acid in the chymus.
The muscularis of the small intestine consists of two layers of smooth muscles.
- Longitudinal fibres—outer, thinner layer
- Circular fibres—inner, thicker layer
Apart from the main part of the duodenum, the serosa covers the entire small intestine.
Specifics of the Small Intestine
Special structural characteristics of the small intestine facilitate digestion and resorption—the so-called valves of Kerckring. They are mucosal and submucosal folds. They boost the resorption by extending the surface and allow the chymus to move helically instead of straightthrough the intestine.
The small intestine also has villi, which do some resorption and digestion and give the intestinemucosa its velvety appearance.
Apart from valves of Kerckring and villi, the small intestine also contains microvilli, extensions of the free membrane of the resorption cells, which build a fuzzy line (brush border) and reach into the lumen of the small intestine.
Specifics of the Large Intestine
Just like the esophagus and small intestine, the large intestine contains four typical layers: mucosa, submucosa, muscularis, and serosa.
The epithelium of the mucosa contains most notably resorption cells whose purpose is to reabsorb water and goblet cells that secrete mucus thus lubricating the bogus. The resorption and goblet cells are located in the intestinal glands (crypts of Lieberkühn), which are found in the entire diameter of the mucosa.
As opposed to the small intestine, there are no valves of Kerckring or villi. However, microvilliof the resorption cells for reabsorbing purposes are present.
The muscularis consists of the following layers:
- Outer layer of the smooth longitudinal muscles
- Inner layer of the circular muscles
One characteristic of the GI tract is the presence of longitudinal muscles, which are thickened into three well-visible longitudinal ligaments (Taeniae coli). These ligaments run across the whole length of the large intestine. Clonical contractions give rise to a range of pockets (haustra coli, singular: haustrum), which give the colon its puckered appearance.
Between the longitudinal ligaments, there is one single layer of smooth circular muscles.
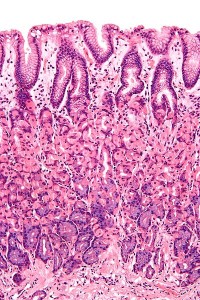
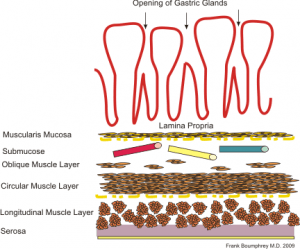
Gastric mucosa and its glands’ Histology
Apart from some deviations, the gastric mucosa consists of the same four layers as the whole GI tract.
One single layer of cylindrical epithelial cells constitutes the surface of the mucosa. Their function is to secrete mucus. The mucosa consists of a lamina propria with areolar connective tissue and muscularis mucosae, which is characterized by smooth muscles.
Many epithelial cells are located in the lamina propria, forming columns with secretory cells. These are called gastric glands, which in turn are lined with many narrow canals, the so-called gastric pits. Each of these gastric pits is filled with the secretion of several gastric glands before the secretion flows into the lumen of the stomach.
The gastric glands contain three types of exocrine gland cells:
- Foveolar cells: They secrete mucus just like the mucous cells at the surface
- Gastric chief cell: Their main function is the secretion of pepsinogen and gastric lipase.
- Parietal cells: They produce hydrochloric acid and the intrinsic factor, which is essential for reabsorption of vitamin B12.
Picture: “Normal gastric mucosa intermed mag” by Nephron. License: CC BY-SA 3.0
Gastric juice consists of the secretions of foveolar, parietal, and gastric chief cells. They produce 2—3 liters of gastric juice per day.
The G cell, an enteroendocrine cell which secretes the hormone, gastrin, into the blood, is also one of the gastric glands and is mainly located in the pyloric glands of the stomach antrum.
Three additional layers, namely the submucosa, muscularis, and serosa, lay beneath the mucosa.
The submucosa is characterized by areolar connective tissue.
The muscularis of the stomach has three layers of smooth muscles. An outer longitudinal layer, a middle circular layer, and an inner angular layer that is primarily limited to the corpus of the stomach.
The serosa consists of single-layered squamous epithelium and areolar connective tissue. It covers the stomach and is part of the peritoneum viscerale. At the small curvature of the stomach, it reaches into the liver.
Picture: “Gastric anatomy” by Boumphreyfr. License: CC BY-SA 3.0
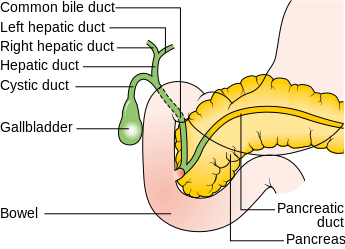
Liver – Lobules and Glisson’s Capsule
The liver is the heaviest organ in a human body and is located below the diaphragm. At the bottom of the liver, there is a pear-shaped, 7—10 cm long pouch: the gallbladder.
The liver can be divided into two main lobes separated from each other by the falciform ligament:
- Right lobe
- Smaller left lobe
The falciform ligament spreads from the bottom of the diaphragm through the two lobes to the upper surface of the liver. Its function is to “fasten” the liver in the abdominal cavity.
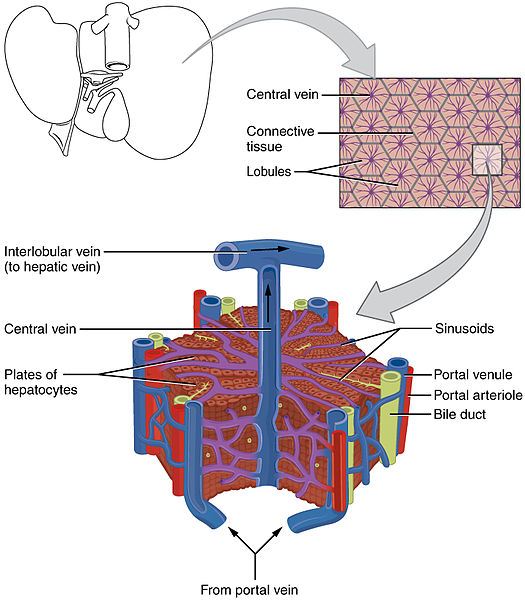
The lobes of the liver consist of many small functional units, the so-called liver lobules. These lobules have a hexagonal structure and are made of specialized epithelial cells that are called hepatocytes. The cells are arranged in irregularly branched and linked panels having a vein at the center.
The liver lobules additionally contain highly permeable capillaries through which blood flows. They are called liver sinusoids.
Kupffer cells are found in the liver sinusoids and are responsible for phagocytosis. They destroy dead white and red blood cells and other bacteria as well as impurities that originate from the gastro-intestinal tract.
The hepatocytes secrete bile that reaches the small biliary canal and empty into the small bile ducts (ductus biliferi). The bile ducts create the large right and the left hepatic duct, which incorporates and leaves the liver as common hepatic duct (ductus hepaticus communis). Together with the ductus cysticus (cystic duct), it creates one single bile duct after the gall bladder, the so-called ductus choledochus.
Blood Supply of the Liver
Picture: “Diagram showing the position of the bile ducts” by Cancer Research UK uploader. License: CC BY-SA 4.0
The liver receives blood from two different sources:
- Blood rich in oxygen from the hepatic portal vein (A. hepatica)
- Blood poor in oxygen from the hepatic arteries (V. portae), including nutrients, pharmaceutical substances and possibly microbes and toxins from the gastro-intestinal tract
The hepatic portal vein and the hepatic arteries carry blood into the sinusoidal liver capillaries, where oxygen, nutrients and specific toxins are absorbed by the hepatocytes. Through the central vein, which ends in a liver vein, specific nutrients required by different cells are carried through the blood.
Glisson’s Capsule (Trias hepatica)
The Glisson’s capsule is located at the edge of the liver lobules and consists of the branching of the portal vein, the proper hepatic artery, and the bile duct.
Common Exam Questions on Oral Cavity and Gastrointestinal Tract
Solutions can be found below the references.
1. Which saliva gland serves as an immunological defence against germs in the oral cavity?
- Glandula parotideae (ear)
- Glandula submandibularis (lower jaw)
- Glandula sublingualis (sublingual)
- Glandulae buccales in the mucosal of the cheeks
- Glandulae palatinae in the mucosal of the pharynx
2. Which are the three special features of the mucosa of the small intestine help in the resorption of nutrients?
- Villi, microvilli, and Brunner’s glands
- Microvilli, Brunner’s glands, and haustra coli
- Valves of Kerckring, villi, and microvilli
- Valves of Kerckring, villi, and haustra coli
- Adventitia, Brunner’s glands, and haustra coli
3. Which of the following carries out the process of phagocytosis of dead white and red blood cells in the liver?
- Peyer’s patches
- Lobuli hepatis
- Hepatocytes
- Kupffer cells
- Alveolar monocytes
Comentários
Enviar um comentário