Skin Infections: Erysipelas and Molluscum Contagiosum — Symptoms and Treatment
Table of Contents
- Definition of Erysipelas and Molluscum Contagiosum
- Epidemiology of Erysipelas and Molluscum Contagiosum
- Etiology of Erysipelas and Molluscum Contagiosum
- Pathophysiology of Erysipelas and Molluscum Contagiosum
- Clinical Presentation of Erysipelas and Molluscum Contagiosum
- Diagnostic Workup for Erysipelas and Molluscum Contagiosum
- Differential Diagnosis of Erysipelas
- Treatment of Erysipelas and Molluscum Contagiosum
- References
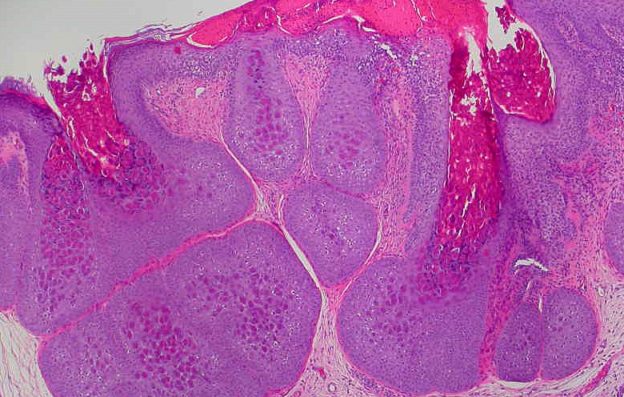
Image: “Molluscum Contagiosum skin biopsy from the back of a 13-year-old girl.” by Ed Uthman, MD. License: Public Domain
Definition of Erysipelas and Molluscum Contagiosum
Erysipelas can be defined as superficial skin infection that affects the dermis in addition to the superficial cutaneous lymphatics. The condition is caused by bacterial agents.
Molluscum Contagiosum is defined as viral infection of the skin that only affects humans resulting in a mild skin rash. The disease is generally mild and should not be a reason for concern or worry. It is not serious and generally clears within 12 – 18 months without treatment. Molluscum Contagiosum causes multiple raised dome-shaped pink skin lesions that are umbilicated. The virus belongs to the Poxviridae family.
Epidemiology of Erysipelas and Molluscum Contagiosum
Erysipelas incidence has been decreasing recently since the introduction of antibiotics. In the past, most cases of erysipelas occurred in the face. Nowadays, 80% of the cases occur in the lower legs most likely due to an aging population.
Possible risk factors for erysipelas include poor hygiene, poor sanitation and history of lymphedema. The peak incidence of erysipelas is in patients older than 60 years. History of recent mastectomy, pelvic surgery or bypass grafting increases the risk of erysipelas most likely because of the associated risk of lymphedema.
Image: “Erysipelas of the left ear.” by Evanherk – Own work. License: CC BY-SA 3.0
Molluscum Contagiosum is accountable for at least 1% of all skin conditions presenting to the treating physician. Hence, the condition is considered as one of the most common skin infections in the United States. Prevalence of Molluscum Contagiosum is higher in patients with HIV especially if the CD4 count is less than 100 cells/microliter. Prevalence of Molluscum Contagiosum skin infection in AIDS patients is estimated to be 30%.
Molluscum Contagiosum infection rates are higher among whites compared to other races. Males are also more likely to develop the condition. The highest incidence of Molluscum Contagiosum infection is reported to be in children younger than 5 years of age. The condition is very rare in children younger than 1 year most likely due to maternal transmitted antibodies against the virus.
Etiology of Erysipelas and Molluscum Contagiosum
The most commonly implicated organism in erysipelas is streptococci. Group A streptococci are responsible for most cases of facial erysipelas while non-group A streptococci are the etiology of lower limbs erysipelas. Newborns might also develop erysipelas that is due to group B streptococci.
Risk factors for developing Erysipelas :
- People with lymphedema
- Nephrotic syndrome
- Arteriovenous insufficiency,
- Diabetes
- Compromised body immunity
- Paretic limbs
Molluscum Contagiosum skin infection is caused by the exposure to infected people who have the condition. The virus can be inoculated from other people or from the same patient, i.e. auto-inoculation. Most cases have history of recent skin trauma, i.e. shaving, because the virus is more likely to invade damaged skin rather than intact skin. Molluscum Contagiosum can also be transmitted sexually, hence it can be considered as a sexually transmitted disease in adults.
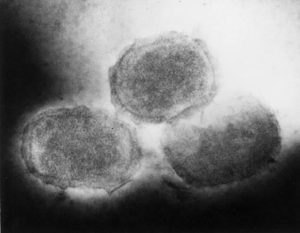
Three different viruses are thought to be responsible for Molluscum Contagiosum disease. Orthopoxvirus, Parapoxvirus and unclassified Poxviridae viruses.
Pathophysiology of Erysipelas and Molluscum Contagiosum
Once streptococci get entry to damaged skin, especially if the patient has lymphedema, the infection quickly invades the lymphatic vessels in the superficial layers of the skin. There, the bacteria start spreading in the lymphatic vessels, and the skin overlaying the infected area develops streaking. Regional lymphadenopathy happens.
Image: “Molluscum contagiosum.” by Evanherk from nl. License: CC BY-SA 3.0
Molluscum Contagiosum viruses enter the cytoplasm of the epithelial cells where they replicate. The infected cells enlarge in size and develop cytoplasmic inclusions. The virus can only replicate in the epidermis and is thought to exclusively affect humans. While the virus initially resides in the basal cell layer, it is noted that viral replication and DNA synthesis only happen after 7 weeks. Therefore, it is suggested that the virus can only replicate once it is in the spindle and granular layers of the epidermis.
Viral replication and infection of the epidermis causes epithelial cell proliferation and the formation of lobulated epidermal growth. Additionally, fibrous septa between the epidermal growths occur, which eventually leads to the formation of the characteristic skin lesions associated with the virus. The virus does not develop latency, instead it evades the immune system by tricking it with viral-specific proteins.
Clinical Presentation of Erysipelas and Molluscum Contagiosum
Recent history of minor skin trauma can be noted in few cases of erysipelas but most cases happen without any precedent event. Here are some of the common prodromal systemic symptoms often experienced by patients before the onset of the skin infection ;
- Chills
- High fever
- Infected site is tenderto palpationcan
- Burning sensation
- Nausea
- Muscle pain and headaches
Previous medical history of diabetes, hypertension and lymphedema are usually present.
Patients infected with Molluscum Contagiosum are usually asymptomatic. If patients develop any symptoms, they usually complain of recent onset of rounded dome-shaped skin lesionsthat can be multiple or single. These lesions are tender and painful. Fever, nausea and fatigue are not common in this condition.
Patients with certain skin conditions such as eczema or psoriasis are more likely to have more spread of the viral infection. Once the patient scratches the skin lesions, auto-inoculationhappens and new lesions can form in the scratched areas. Multiple lesions can last up to 3 years while single lesions usually resolve within two months. Recent history of contact with an infected individual might be elicited in a number of cases.
People with history of HIV infection are at an increased risk of severe wide spread erysipelas and Molluscum Contagiosum infections.
Diagnostic Workup for Erysipelas and Molluscum Contagiosum
Erysipelas is a clinical diagnosis and laboratory investigations are not needed. If blood testingis performed, patients can have leukocytosis, elevated erythrocyte sedimentation rate and increased C-reactive protein levels in the blood.
Patients with severe joint pain might have septic arthritis or osteomyelitis. In these patients, magnetic resonance imaging and bone scintigraphy can be helpful. Blood and skin cultures can confirm the presence of bacterial infection but are usually negative, therefore, they are not recommended.
Image: “Transmission electron micrograph of poxvirus of molluscum contagiosum.” by Unknown – http://phil.cdc.gov/PHIL_Images/08061998/00006/B81-166_lores.jpg. License: Public Domain
Similarly, Molluscum Contagiosum is also a clinical diagnosis. The skin lesions of Molluscum Contagiosum are very characteristic and are usually enough for the diagnosis. If a biopsy is performed, intracytoplasmic inclusion bodies can be seen on histologic examination.
Compression of the lesions can reveal a pasty corewhich if stained properly is usually abundant with the virus particles. Serum specific antibodiesagainst Molluscum Contagiosum viruses are not clinically indicated but they are available for research indications.
Polymerase chain reaction testing is available for quick and accurate confirmation of the presence of the virus in the skin lesions. Viral cultures do not have a role in Molluscum Contagiosum because routine cultures are not known to grow the virus. Adults with Molluscum Contagiosum are at risk of other sexually transmitted diseases and should be examined and offered the appropriate diagnostic workup to exclude them.
Differential Diagnosis of Erysipelas
Erysipelas is a type of soft-tissue infection, and should be differentiated from another similar dermatological condition, called: Cellulitis.
Treatment of Erysipelas and Molluscum Contagiosum
Erysipelas
Treatment of erysipelas consists of two main components – prompt antibiotic administrationand symptomatic treatment. Symptomatic treatment for fever and headache, adequate hydration, cold compresses of the affected lower limb and elevated of the affected limb are essential to avoid spread of the infection.
Penicillin administration orally or intramuscularly is the antibiotic of choice for the treatment of erysipelas. Patients with penicillin allergies can be prescribed a first generation cephalosporin. Clindamycin is a second-line antibiotic because some group B streptococci might be resistant. Roxithromycin and pristinamycin are two recently approved drugs for the treatment of erysipelas. They are superior to penicillins and with fewer side effects.
Molluscum Contagiosum
Treatment options for Molluscum Contagiosum can be neglect, direct lesion trauma, antiviral therapy and immune response stimulation. Children and healthy individuals should be assured that the lesions will eventually disappear and should be advised to simply neglect them.
Those who refuse this approach can benefit from minor direct lesion trauma. Cryotherapy with liquid nitrogen, and curettage are the most commonly used forms of direct lesion trauma. They are effective but can be painful and not comfortable for a child.
Imiquimod is a drug that was found to activate the immune response against Molluscum Contagiosum. Despite its efficacy, the cost of applying this product is deemed too high to be considered as a first-line therapy for the disease in healthy individuals.
Immunocompromised patients with Molluscum Contagiosum are at risk of severe and extensive infections, therefore, ritonavir and cidofovir intravenously should be used. These antiviral drugs have been continuously shown to be effective in the treatment of extensive Molluscum Contagiosum disease in AIDS patients


Comentários
Enviar um comentário