Modes of Ventilation
In Lecturio :) Sometimes ventilation is the only way to save a patient's life. Here you'll read about the different forms of mechanical ventilation, how it is different from spontaneous breathing and what modes of ventilation exist.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your course “Pulmonary Pathology” now for free!

What is Mechanical Ventilation?

Image: “Respirator “Evita4” on an ICU” by Blogotron. License: CC0 BY 1.0
- Partial pressure of oxygen < 50mmHg
- Partial pressure of carbon dioxide > 50mmHg
This form of ventilation may be invasive requiring intubation or non-invasive, making use of masks and tubes. When discussing ventilation, there are certain terms you need to be familiar with:
- Respiratory rate: Rate of breaths: could be a ventilator setting or the actual respiratory status of the individual being tracked by the ventilator
- Volume of breaths: Frequently known as tidal volume;: again could be a ventilator setting or patient’s status being tracked
- Breathing sensitivity: Related to the inspiratory effort required from the ventilator to identify the patient’s effort of inhaling
- Flow of breaths: Peak flow
Modes of Ventilation
There are various combinations of modes and breath types offered by manufacturers of ventilators to determine the breath delivered to a patient. Some common ventilator modes are as follows.Assist/Control (A/C)
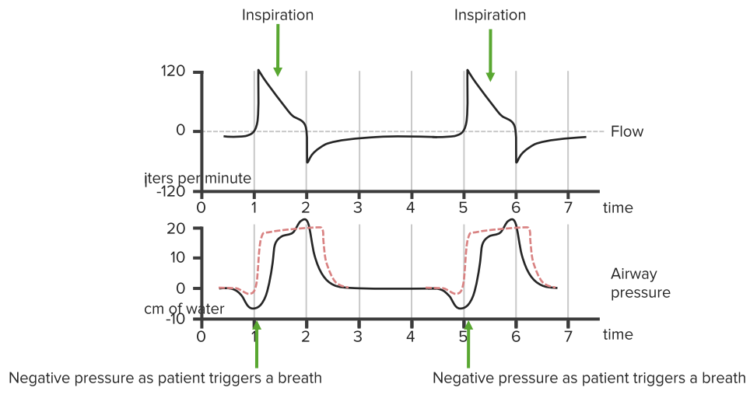
This is the mode where every breath is supported by the ventilator, whether initiated by the patient or the ventilator itself. Often the patient rests and ventilator does the work. This type of support is required in:
- Resuscitated patients
- Patients with acute respiratory distress syndrome
- Paralyzed patients
- Sedated patients
Risk: Barotrauma risk is there due to the highest level of positive pressure in the chest.
Synchronized Intermittent Mandatory Ventilation (SIMV)
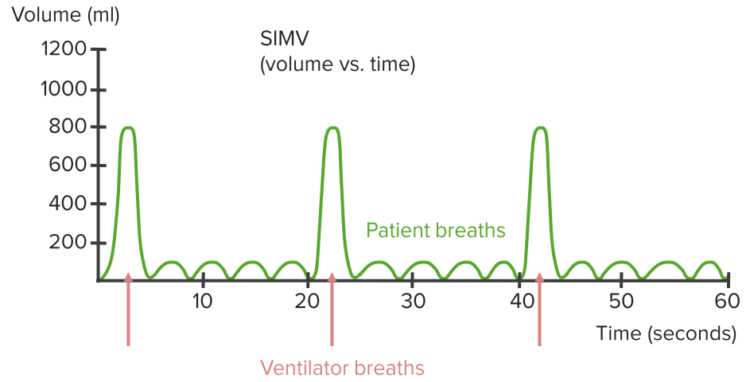
This mode assures a certain number of breaths and reduces the risk of hyperinflation and alkalosis. Mandatory breaths are synchronized such that they coincide with spontaneous respirations. SIMV in patients with LV dysfunction has shown to reduce the cardiac output.
Disadvantages: An increased work of breathing and reduced cardiac output prolonging ventilator dependency.
While deciding between SIMV and A/C, personal choice is seen, however, SIMV is preferred in patients who breathe rapidly and A/C is the choice is patients with:- Respiratory weakness
- Left ventricular dysfunction
Continuous Positive Airway Pressure (CPAP)
This is the mode where the patient is responsible for initiating and sustaining the breathing process. The ventilator:- Controls delivered oxygen concentration
- Delivers required flow and volume meeting the patient’s inspiratory demands
Pressure Controlled Ventilation (PCV)
PCV can be used in both SIMV and A/C modes, and targets a particular pressure during inspiration. In simple words, pressure controls the end point instead of volume. The flow rate being delivered depends on the following characteristics, which also determine the tidal volume:- The patient’s demands
- Lung compliance
- Airway resistance
Pressure Support Ventilation (PSV)
A kind of spontaneous breath that can be used in either CPAP or SIMV mode is basically like PCV targeting specific inspiratory pressure. However, the difference here is that the inspiration ends as the lungs get full and the flow delivered reduces to a value set by the clinician. PSV can be delivered through special face masks. In this mode, the patient gets to decide:- Respiratory rate
- Inspiratory time
- Tidal volume
- Flow rate
Positive End-Expiratory Pressure (PEEP)
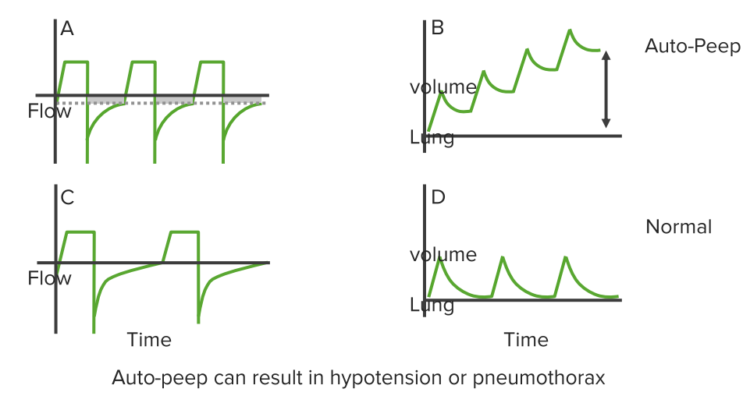
This involves applying mechanical positive pressure at the end of expiration so that complete emptying of lungs is prevented. The plus point of this type of mode is the increased lung volume and improvement in oxygenation.
The effect of PEEP can be very well measured by looking at the peak inspiratory pressure (PIP). If PIP increases less than added positive end-expiratory pressure then lung compliance has improved. PEEP is clinically indicated for:
- Low-volume ventilation cycles
- Stiff and diffusely injured lungs with FiO2 requirement > 0.60
- Obstructive lung disease
Comentários
Enviar um comentário