Anatomy of the Spinal Column
In Lecturio . The human spine has various tasks. It helps us to be upright, ensures stability, provides muscles, tendons and other tissues with osseous starting points and passage openings, can distribute loads and is still flexible and movable. The downside of this is that such a complex structure with so many functionalities is, unfortunately, an equally versatile focus for diseases. In 2011, approximately 230,000 spinal surgeries were performed, and an upward trend has been observed. Students of human medicine should be introduced to the anatomy of the spine early on, to diagnose pathologies timely and spare patients’ problems associated with such an operation.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your anatomy course now for free!

General Information about the Spinal Column
Overview of the spine
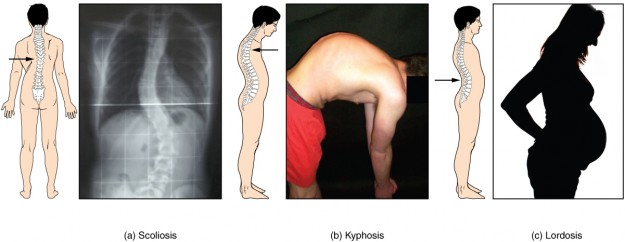
Image: “Abnormal Curvatures of the Vertebral Column” by Phil Schatz. License: CC BY 4.0 a) Scoliosis is an abnormal lateral bending of the vertebral column. (b) An excessive curvature of the upper thoracic vertebral column is called kyphosis. (c) Lordosis is an excessive curvature in the lumbar region of the vertebral column.
The sacrum is a bony structure consisting of 5 coalesced sacrum vertebrae. Because the sacral vertebrae, however, are no longer motion segments due to the merger, they are not counted as real vertebrae of the spine. The same is true for the tailbone (coccyx), which represents a fusion of 4 coccyx vertebrae, which no longer contain motion segments.
Some people have 6 lumbar vertebrae (lumbarization of S1) or 3-6 coccyx vertebrae; this, however, has no pathogenic effect on the skeletal system. Except in the segments C0/C1 and C1/C2 a disc is located between each vertebra, which primarily takes over buffering and protection functions.
Considering the spine laterally, a clear S-curvature can be seen. The S-shape is determined by a lordosis of the cervical and lumbar spine, as well as a kyphosis of the thoracic spine. The S-shape serves to mitigate longitudinal forces; secondary and lateral shear forces, even if the muscles intercept them more than the osseous and capsular ligament structures of the column vertebrae.
The spine is covered by strong band systems that ensure stability and limit certain movements so that they cannot inflict any harm to the surrounding structures. Furthermore, the spine makes up the spinal canal, which serves as a port for our spinal cord and spinal nerves that pass into peripheral neural structures outside of the canal.
The mobile segment
The motion segment is the functional unit of the spine, which is formed by two adjacent vertebrae (e.g. C6 and C7 in the cervical spine). In addition, the following structures are part of the mobile segment:- The space between the vertebrae and the intervertebral disc
- Vertebral arches
- Spinous and transverse process sets
- All soft tissue present in the segment
- The spinal nerve in the segment
- The skin area innervated by segment spinal nerve
The ventral system – consisting of the vertebral body and intervertebral disc – has the primary task to incorporate axial compressive forces and to pass them on, so that they can be compensated without causing damage. Furthermore, the ventral system is capable of limiting movements. The dorsal system consists of the vertebral arch joints, muscles, and ligaments and serves the implementation and inhibition of movement.
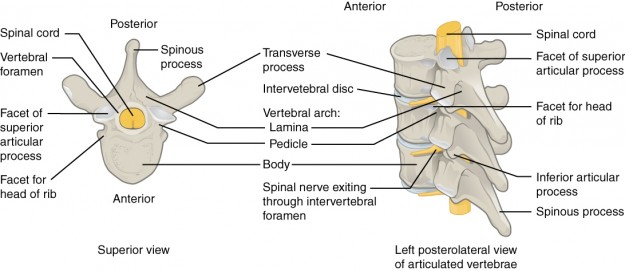
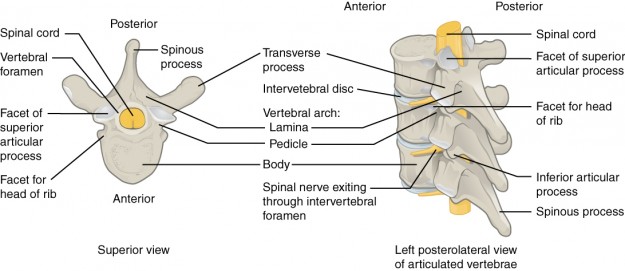
Vertebral body
Looking at the vertebral body laterally, the block-like vertebral body, which is forming the so-called borders cranially and caudally, can be observed. These borders are bony ridges that limit the bearing surface of the disc onto the vertebral bodies and act as a point of fixation for fibrocartilage.In the transverse section, the vertebrae are structured anteriorly convex and posteriorly straight. The osseous body itself is made of a cancellous bone structure, which is encased in cortical bone. These structures ensure fault lines within the corpus, running cranial to caudal to the spine and ensure the transmission during axial compression. If this system did not exist, the lightest pressure forces would cause the vertebral body to fracture. The base- and endplates covered with hyaline cartilage close the corpus from the disc, the disc surface facing the spinal disc consists of fibrocartilage.
Vertebral arch
The vertebral arch, also called neural arch, is present posteriorly to the vertebral body. It is formed by lamina dorsally and pedicles laterally. In the transition region between pedicle and lamina, the articular processes are present, cranial (superior articular process) and caudal (inferior articular process), which, together with the respective adjacent segments, make up the so-called facet joints. The lamina consists of two symmetrical halves, which are fused bones.From the vertebral arch, three processes project. The spinous process (or spine) is present in the posterior midline, while the two transverse processes are present on either side at the junction of the pedicle and lamina.
Vertebral foramen
The vertebral foramen is a large central opening that is formed between the vertebral body anteriorly and vertebral arch posteriorly. The diameter and shape of the vertebral foramen varies, depending on the segment level, as a result of the differences in size of the vertebral bodies, depending on the spine section and their positioning in the cavity.Due to its “building-block appearance” of the spine, the vertebral foramina collectively form the vertebral canal through which the spinal cord run along with its meninges and associated structures. In the lumbar spine, the transition region between the spinal canal and intervertebral foramen is described as a lateral recess, which is lined with epidural fatty tissue. Here the nerve root passes through.
The spinal canal
The spinal canal (or vertebral canal) forms a passage opening for a number of important structures of the human body. This contribution is limited to the neuronal structures spinal cord, and the spinal dura mater.Spinal cord
The spinal cord is a core element of the central nervous system. It ends at L1/L2 with the conus medullaris, which continues caudally in the cauda equina. Furthermore, the spinal cord consists of cervical and lumbosacral enlargements, from which the cervical and lumbar spinal nerves emerge and form their respective plexus.
Spinal dura mater
The dura mater is the outer sheath of the meninges, which consists of collagen and elastic fibers. The spinal dura mater is only localized on the canalis. The other portion of the dura mater is located in the skull and is called cranial dura mater due to its location.
Transverse Processes
The transverse process springs from the vertebral arch of each vertebra from the junction of the pedicle and the lamina and differs depending on the segment in size, shape, and orientation in the cavity.In the cervical spine, the transverse process bears anterior and posterior tubercles. Between these bony structures, the transverse foramen is located, which serves as a pass-through opening for the vertebral artery.
In the thoracic spine, the transverse processes are dominantly established and are equipped with articulating surfaces, which articulate with the tubercle of the ribs.
In the lumbar spine, the transverse process bears three tubercles/processes i.e., costiform process, mamillary process and accessory process.
Spinous Process
The spinous process (or spine) is the posterior bony projection of the vertebral arch. It is a fixation point for muscles and ligaments and is also a noticeable starting point in palpation diagnostics. It splits up in two (kind of like a fishtail) in the segments C2 – C6 and merges again from C7 on. In the thoracic spine, the spinous processes are very long and have an oblique caudal course, while in the lumbar region they are formed high and are more heavily built.Intervertebral foramen
The intervertebral foramen is formed by the superior and inferior vertebral notches of each adjacent vertebral segment and serves as a passage opening for the spinal nerve, meningeal branch, spinal artery and intervertebral vein.Articular processes
Four vertebral articular processes (two superior and two inferior) spring from each vertebral arch; ending with an articular surface, the articular facet, and a vertebral arch joint.The facet joints
The facet joints are real joints, each of which consists of cartilage joint covered surfaces and a joint capsule. They absorb compressive forces and transmit them so that movements can be performed selectively and without injury. The control is achieved via proprioceptive receptors in the capsular ligaments.Due to the spatial alignment of the joint surfaces, certain movements can be made better or worse than in other portions of the spinal column. The angle of inclination of the articular surfaces in the cervical spine is approximately 45 degrees, relative to the horizontal, while this angle is significantly higher in the thoracic spine, approximately 80 degrees. In the lumbar region, the angle of inclination is about 90 degrees, which makes the rotation in the lumbar spine significantly lower than that of the thoracic or cervical spine.
Intervertebral Disc
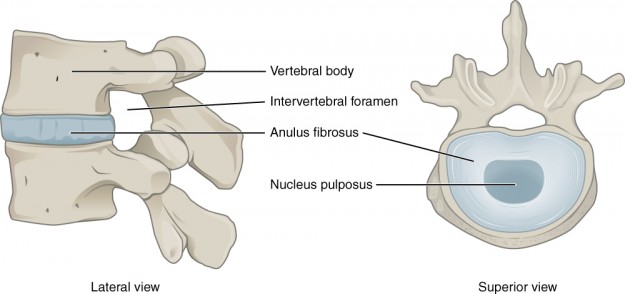
The human body has 23 intervertebral discs as there are no discs located between the two upper cervical segments (the atlas and the axis). Their diameter varies according to the size of the spine “column” because of the different pressure loading conditions. An intervertebral disc is divided into two parts: the annulus fibrosis and the nucleus pulposus.Annulus fibrosis
The annulus fibrosis is composed of several layers and encloses the spinal disc nucleus, the nucleus pulposus. It is composed of 60 – 70% of water. The layers are composed of collagen fibers running in different directions depending on the layer. This makes sense for compiling enough compressive and tensile strength during every movement, functioning as a shock absorber, and protecting the discs from immediate rupture. The annulus is attached by its sharp fibers to the edge strips of the vertebral body and is adhered dorsally with the posterior longitudinal ligament. It shares low fiber contents with the anterior longitudinal ligament.
Nucleus pulposus
The nucleus pulposus is a gel-like substance inside the disc. It consists of a combination of collagen fibers and glycans (proteoglycan, glycosaminoglycan), resulting in a high matrix formation and, therefore, strong water binding tilt. The nucleus pulposus contains neither vessels nor nerves and serves the voltage shift of discs during spinal movements. It receives its nutrition from the surrounding vessels by the process of diffusion. Overnight, the disc takes on liquid, which increases its height. This is the reason why a person is taller in the morning after a restful night’s sleep following a tiring day.
When a herniated disc nucleus occurs, the nucleus emerges through a tear of the annulus fibrosis and compresses the nearby spinal nerve roots, which may result in pain and neural deficits.
Ligaments
Ligament system of the spinal column
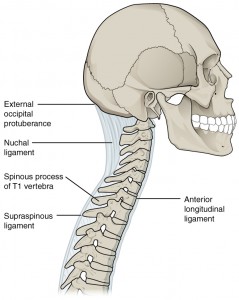
A motion segment can only be fully understood with its functional ligament structures. They stabilize the spine in the neutral zero position and limit movements before they fall into pathological proportions and delicate structures can be irritated or damaged.Posterior longitudinal ligament
This ligament originates at the clivus of the occipital bone and runs the entire dorsal side of the spine to the ventral edge of the sacrum canal. On its way, it connects with the annulus fibrosis of the intervertebral discs in each segment, as well as the marginal edges of the vertebral bodies. Its purpose is stabilizing the posterior intervertebral disc area and controlling or limiting flexion.Anterior longitudinal ligament
The anterior longitudinal ligament has its origin at the anterior tubercle of atlas. It runs anterior along the vertebral bodies and is attached to the same. In contrast to the posterior longitudinal ligament, the anterior ligament is connected to the intervertebral discs with only a few fibers. In addition to its stabilizing function, this ligament controls and limits the extension and lateral flexion of the spine.Interspinous ligaments
As the name suggests, the interspinous ligaments extend from the spinous process to spinous process of the adjacent vertebral bodies. They also connect to the supraspinous (dorsal) and the flava (ventral) ligaments. In the cervical spine, they become a part of the lig. nuchae and serves to stabilize, control and limit flexion, lateral flexion and rotation.Supraspinous ligament
This ligament extends from the spinous process to spinous process of the adjacent vertebral bodies of C7 to the sacrum. It assumes the same functions as the interspinous ligaments, namely stabilization, control and limitation of flexion, lateral flexion and rotation.Intertransverse ligament
Like the supraspinous ligament, the intertransverse ligament also connects the spinous process tips of adjacent vertebral bodies. It limits both flexion and lateral flexion.Flavum ligament
The flava ligaments extend over the dorsolateral spinal canal and originate from the vertebral arch lamina of two adjacent vertebrae, or insert into them. In the thoracic and lumbar spine, they are connected to the joint capsule of the zygapophysial (facet joint) type. It is one of the strongest ligaments of the spine and stabilizes the vertebral arch joint during flexion.Functional Anatomy
Movement axes of the spinal column
The movement axes of the spine are located in the intervertebral disc.- The horizontal axis for flexion is located ventrally, the one for extension—dorsally.
- The sagittal axis for lateral flexion is located laterally—this means that the left lateral flexion corresponds to the left, and the right lateral flexion corresponds to the right.
- Finally, the longitudinal axis for rotation is located almost exactly in the middle of the disc.
Flexion and extension
If someone performs a flexion of the spine, the intervertebral disc and the ventral vertebrae are compressed, and the inferior articular surface of the cranial vertebra slides cranially. In biomechanics, this phenomenon is called divergence. Conversely, during spine extension, the dorsal portions are compressed, the intervertebral foramen narrows and the facets of the facet joints lock. This movement is called convergence.Lateral flexion and rotation
During lateral flexion, the concave side of the vertebral joints converges, while divergence takes place on the contralateral side. This causes the foramen to narrow on the side to which the lateral flexion is then performed. During rotation, a contralateral sliding of the facies superior articular takes place. In the cervical spine, this movement always takes place coupled with a lateral flexion.Clinical Examples
Diseases of the spinal column
For the purpose of clarity, this portion will be limited to just three examples.Chondrosis
When the water content in the body, and therefore also the disc, decreases with advancing age, the amount of collagen fibers increases. The result is a hardening of the nucleus pulposus and decrease in disc height. Thus, the cover plates are more stressed and cracking occurs in the annulus fibrosis. This results in sclerotherapy, or a rupture of the annulus, which may cause a prolapse.Prolapsed (Slipped) disc
If all tissue layers of the annulus fibrosis rupture, the gel-like nucleus pulposus leaks outwardly and compresses the delicate tissue (colloquially herniated disc). If the nucleus enters into the spinal canal and irritates the spinal nerve, pain can develop and neuronal lesions (such as paresthesia or motor paralysis) can occur. Depending on the height of the segment at which the prolapse occurs, it can also lead to the loss of the bladder rectum function (cauda equina syndrome). If the nucleus dissolves completely from the annulus, this is called sequestration. If the nucleus only penetrates partially, and without the annulus suffering a complete tear, this is known as a protrusion in medicine.Spinal Stenosis
Spinal stenosis refers to a narrowing phenomenon, which can be the result of a prolapse, but also tumors or inflammation with edema. There is a central and lateral stenosis, depending on the localization of the pathogenic event. Depending on the location and severity, the spinal nerve, spinal cord or blood vessels may be affected by the compression.Common Exam Questions about the Spinal Column
The answers can be found below the references.Where in the human spine is there no intervertebral disc?
- L1/L2 + L2/L3
- Th11/Th12 + Th12/L1
- C0/C1 + C1/C2
- L4/L5 + L5/S1
- An intervertebral disc is located between each vertebra.
- C1 – C4
- C1 – C7
- C2 – C7
- C2 – C6
- C3 – C6
- Vertebrae
- Vertebral arch
- Vertebral foramen
- Zygapophysial joint
- Intervertebral disc

Comentários
Enviar um comentário