Breast Masses in Adolescents: Intraductal Papilloma, Fibroadenomas and More
Breast masses are uncommon in adolescents but can cause significant distress to the affected individual. They are usually benign fibroadenomas, intraductal papilloma, or phyllodes tumors. Malignant phyllodes tumors and primary breast cancer are very rare in adolescents but have been diagnosed before. Treatment of benign lesions is usually local excision, whereas malignant lesions usually need complete surgical resection. Chemotherapy and radiotherapy are not recommended in adolescents with breast cancer.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your adolescent medicine course now for free!
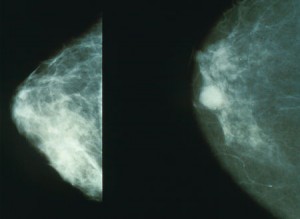
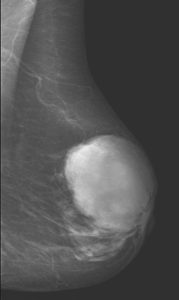
Image: “Normal (left) versus cancerous (right) mammography image.” License: public domain
Overview
Benign and malignant breast masses are uncommon in adolescents. Despite being rare, breast masses usually cause significant worry and distress to the adolescent and her family. Breast masses in adolescents are usually benign and are usually fibroadenomas. Malignant breast masses only constitute 0.02 % of the masses identified in adolescents.| Pubertal breast development mainly under influence of: | |
| Estrogen | Progesterone |
| Lactiferous ducts | Lobular tissue and alveolar budding |
| Female adoloscent breast tisse is very dense and responsive to hormonal changes. | |
| Many breast masses found accidently. | |
Epidemiology of Breast Masses in Adolescents
The estimated prevalence of breast masses in adolescents is around 3.2 %. The most common type of breast masses in adolescents is a fibroadenoma and is diagnosed in up to 95 % of the cases.Malignant breast masses are very rare in adolescent girls but have been reported to exist. Approximately, 0.02 % of the identified breast masses in adolescents are found to be cancerous. Phyllodes tumors, primary breast cancer, sarcoma, lymphangioma, hemangioma, and metastatic cancer are some examples of malignant breast masses that can be seen in adolescents.
Intraductal Papilloma in Adolescents
Clinical Presentation of Intraductal Papilloma
It is the most common cause of non-bloody nipple discharge in an adolescent. Intraductal papilloma can also cause pain. It is important to note the duration and progression of the symptoms. Physical examination of the breast with palpation can express nipple discharge. These benign lesions are usually found in the subareolar area and are usually non-palpable.Diagnostic Workup for Intraductal Papilloma
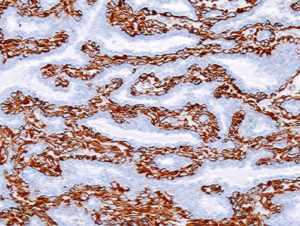
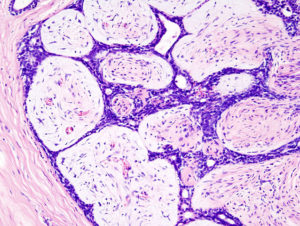
Image: “Histopathology of intraductal papilloma of the breast by excisional biopsy. Immunostaining for alpha-smooth muscle actin.” by No machine-readable source provided. Own work assumed (based on copyright claims). License: CC BY-SA 3.0
Treatment of Intraductal Papilloma
While intraductal papilloma itself is not a pre-malignant condition, the risk of breast cancer in an adult with the previous history of intraductal papilloma has been shown to be increased. Therefore, the treatment of choice of an intraductal papilloma in an adolescent is local surgical excision.Phyllodes Tumors in Adolescents
Clinical Presentation of Phyllodes Tumors
These tumors are cystic lesions that resemble fibroadenomas but with increased stromal content. The term cystosarcoma phyllodes can be also used to describe the lesions. Patients present with a rapidly growing tumor that is large and painless. A clinical examination might be confusing as phyllodes tumors are difficult to distinguish from giant fibroadenomas.Diagnostic Workup for Phyllodes Tumors
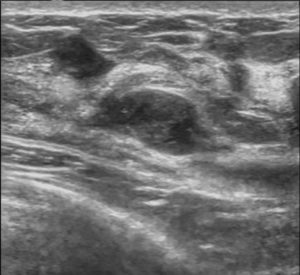
When the main complaint from the adolescent is a large breast mass, the first diagnostic test would be an ultrasonography. Ultrasonography can reveal lobulations and heterogenicity without microcalcifications. Unfortunately, these findings are not specific for phyllodes tumors and their presence is an indication for a core needle biopsy.Histology Findings in Phyllodes Tumors
The typical picture is that of a fibroadenoma with significantly increased stromal proliferation. It is important to identify the degree of dysplasia and proliferation as grading the tumors has been linked with survival rate. The 5-year survival rate for benign phyllodes tumors is 96 %, whereas it goes down to 74 % for intermediate phyllodes tumors. The survival rate after complete resection of malignant phyllodes tumors is around 66 %.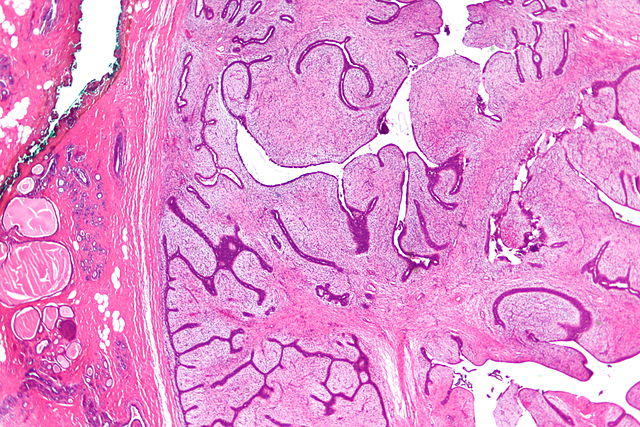
Image: “Very low magnification micrograph of a phyllodes tumour, also spelled phyllodes tumor and also known as cystosarcoma phyllodes, is a tumour of the breast that is usually benign and occasionally malignant. H&E stain. On the left of the images one can see normal breast tissue and fibrocystic change. The green seen in the image is ink to mark the surgical margin.” by Nephron. License: CC BY-SA 3.0
Treatment of Phyllodes Tumors
The treatment of phyllodes tumors in adolescents is similar to adults, i.e., complete surgical resection. The main difference in treatment between adult and adolescents is the unnecessity for a 1 cm surgical margin.Fibroadenomas in Adolescents
Clinical Presentation of Fibroadenomas
Fibroadenomas usually present as firm, non-tender well-demarcated masses. The most common site is the upper-outer quadrant of the breast. The masses can become tender or show cyclic size changes that are related to the menstrual cycle. Breast asymmetry is also a common presenting problem in adolescents. The typical mousy feel of the fibroadenomas, i.e. sliding between the fingers during palpation, is usually observed during the physical examination. The skin overlying the tumors is normal.Diagnostic Workup for Fibroadenomas
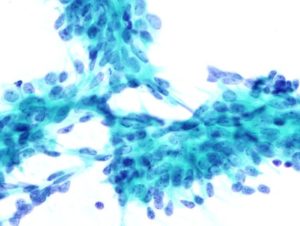
The diagnosis of fibroadenomas in adolescents is easy and is usually based on history and physical examination. If a nipple discharge is present, cytology is indicated. Ultrasonography is the imaging modality of choice for the confirmation of the diagnosis. Mammography is not recommended due to high-density breast tissue.- Image: “Histopathologic image of breast fibroadenoma. Core needle biopsy. Hematoxylin & eosin stain.” by No machine-readable author provided. KGH assumed (based on copyright claims). License: CC BY-SA 3.0
- Image: “Fibroadenoma, Fine Needle Aspiration Biopsy (Papanicolou stain). The image shows a sheet of epithelial cells in the typical antler pattern.” by KGH – Personal collection of histopathologic slides. License: CC BY-SA 3.0
- Image: “Fibroadenoma of the breast. Ultrasound image.” by © Nevit Dilmen. License: CC BY-SA 3.0
| Inspection | Palpation |
|
|
Treatment of Fibroadenomas
The potential of malignant transformation in adolescents who have fibroadenomas is very low. Therefore, the treatment of fibroadenomas in adolescents can be challenging. When the fibroadenoma is diagnosed for the first time, a follow-up should be arranged to see if the mass disappears after the next menstrual period. If the mass does not disappear, they are small and are not painful, treatment can be mainly observation and follow-up. If the lesions are growing in size, or are associated with tenderness, then surgical excision of the tumors is indicated.| Clinical follow up | Surgical excision | NSAIDs or OCPs |
| Most require only clinical follow up | Surgical excision for symptomatic, rapidly growing | NSAIDs or OCPs to help pain with hormone-dependent changes |
Primary Breast Cancer in Adolescents
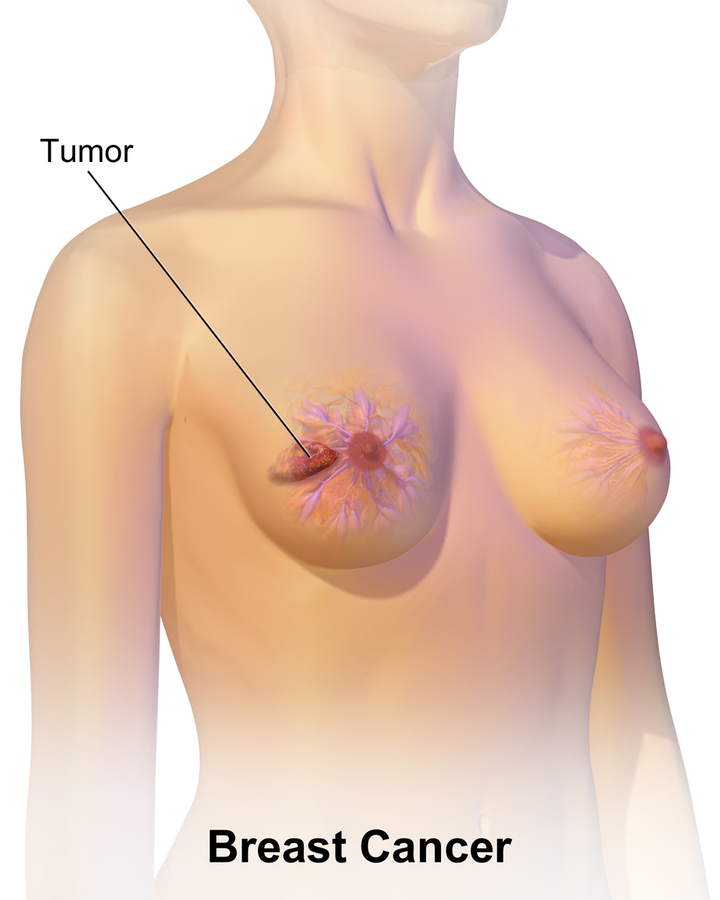
Clinical Presentation of Primary Breast Cancer in Adolescents
The incidence of breast cancer in adolescents is 1 in 1,000,000. Adolescents with breast cancer usually present quite late to the clinic and the mass is usually large. Physical examination reveals a firm, nonmobile mass with poorly circumscribed borders. Nipple discharge and retraction are uncommon in adolescents with breast cancer compared to adults.Diagnostic Workup for Primary Breast Cancer in Adolescents
The most common type of breast cancer in adolescents is a secretory adenocarcinoma. These tumors are characterized by their cystic appearance on ultrasound with a thick wall. Mortality and nodal metastasis are uncommon with secretory adenocarcinoma. Medullary and inflammatory cancer has been also reported in adolescents and pediatrics. Mammography is not recommended in the diagnostic workup for breast masses in adolescents due to the relatively higher density of the adolescent breast compared to the adult breast. Core needle biopsy is indicated for grading and histological examination.Treatment of Primary Breast Cancer in Adolescents
Complete surgical resection should be attempted in all cases. A complete breast resection might be psychologically traumatic to the adolescent; therefore, reconstructive surgery is also indicated. Axillary lymph node staging is indicated. Ultrasonography should be used to assess the status of the axillary lymph nodes and if no metastasis is identified, then a sentinel lymph node should be obtained during surgery.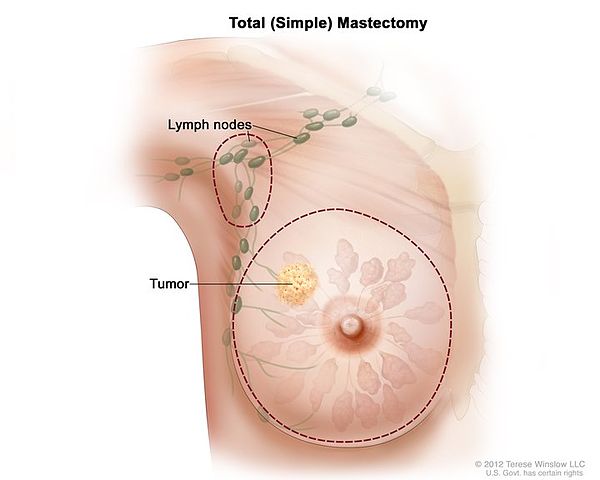
Image: “Total (simple) mastectomy.” by National Cancer Institute – This image was released by the National Cancer Institute, an agency part of the National Institutes of Health, with the ID 7129. License: Public Domain
Metastatic Cancers of the Breast
Many cancers have been associated with metastatic disease to the breasts. The most common examples are hepatocarcinoma, non-Hodgkin lymphoma, leukemia, and rhabdomyosarcoma. The management of these tumors should also cover the breast metastatic disease if present.Management of Breast Infections
Mastitis
- Common in lactating adolescents
- Group A Strep or Staph Aureus
- May present with fever alone, then develop into erythematous, confluent painful rash
- Fever is common
- Treat with cephalexin or clindamycin
Breast abscesses
- Antibiotics
- Warm compresses
- Drainage

Comentários
Enviar um comentário