Liver Transplantation — Clinical Presentation and Post-Transplant Complications
In patients with end-stage liver disease (ESLD), the definitive treatment is a liver transplant. In the United States, the most common indication for liver transplantation is hepatitis C followed by alcoholic liver disease. Immunosuppression is indicated post-implantation and the most common complications are rejection and infection.
Table of Contents
- Introduction to Liver Transplantation
- Definition of Liver Transplantation
- Epidemiology of ESLD
- Indications for Liver Transplantation
- Medical Therapy Before Liver Transplantation
- Clinical Presentation of Patients Needing a Liver Transplant
- Relevant Anatomy for Liver Transplantation
- Immunosuppression Post-Liver Transplantation
- Post-Transplant Complications
- References
Are you more of a visual learner? Check out our online video lectures and start your pathology course now for free!
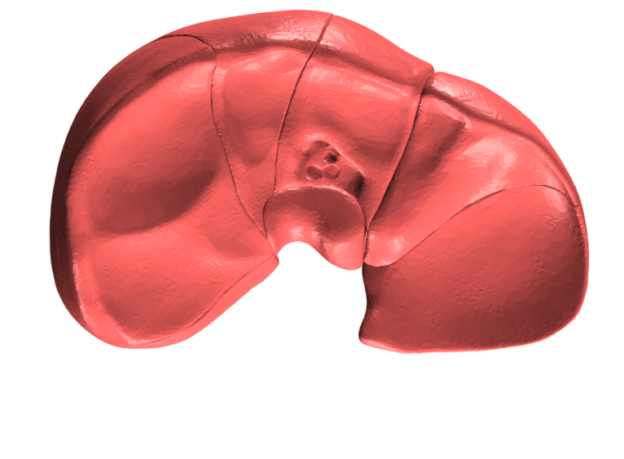
Image : “Liver” by Database Center for Life Science. License: CC BY-SA 2.1
Introduction to Liver Transplantation
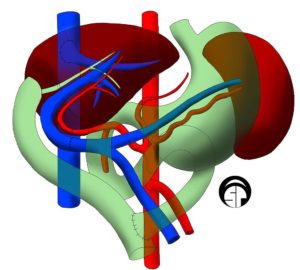
Image: “Illustration of a “split” left liver transplant.” by Aphelpsmd – Own work. License: CC BY-SA 4.0
Definition of Liver Transplantation
Liver transplantation/ hepatic transplantation is the replacement of the diseased liver with a healthy liver from another person (allograft).Epidemiology of ESLD
Approximately, six thousand liver transplants are performed per year in the United States. In 2014, 7,200 liver transplants were performed in the united states with 330 of these involving livers from live patients. This number does not meet the current waiting list of 15,850 patients with ESLD who are candidates for liver transplantation. Currently, ESLD is reported to be responsible for 9.4 deaths per 100,000 persons but this is an under-estimation as cases with acute (fulminant) hepatitis are not included in this figure. The 5-year survival rate after liver transplantation is 72%.Indications for Liver Transplantation
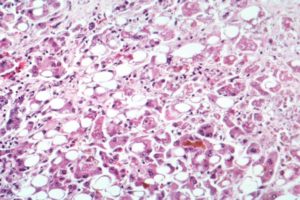
Image: “Microscopy of the liver showing evidence of alcoholic hepatitis.” The original uploader was Countincr at English Wikipedia – Transferred from en.wikipedia to Commons, License: CC BY-SA 2.5
Malignancies of the liver or biliary system, idiopathic liver disease, autoimmune disease, primary biliary cirrhosis and primary sclerosing cholangitis can also lead to ESLD, or be associated with liver cirrhosis and eventually necessitate a liver transplant.
Less common causes of ESLD that could need a liver transplantation include inborn errors of metabolisms, acute liver failure, and the hepatitis B virus.
Medical Therapy Before Liver Transplantation
Patients who will undergo a liver transplantation procedure should be medically managed before the implantation to lower the risk of post-operative complications. This medical management involves managing ESLD complications, such as encephalopathy, ascites, spontaneous bacterial peritonitis and active viral hepatitis.Clinical Presentation of Patients Needing a Liver Transplant
Patients with ESLD who present with recurrent variceal hemorrhage due to portal hypertension, intractable ascites, spontaneous bacterial peritonitis that is recurrent and medically refractory encephalopathy, should be evaluated for a possible liver transplantation.Additionally, any patient with fulminant hepatic failure that is life-threatening should be considered for liver transplantation. The decision to go for liver transplantation can also be based on a decreased quality of life that is intolerable by the patient and not on life-threatening complications alone.
Relevant Anatomy for Liver Transplantation
The liver can be divided into two main lobes, right and left by a line running through the gallbladder fossa in the major fissure.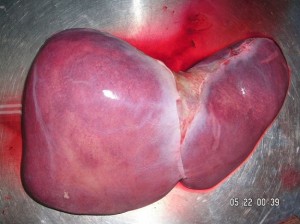
Image: “Human liver showing the right and left liver lobes.” by Suseno.
Recent advances have put forward the segmental anatomy of the liver where the liver is divided into 8 couinaud segments. Each segment has its own vascular inflow, vascular outflow, and independent biliary tract drainage and thus can be excised and replaced independently during segmental transplantation.
Furthermore, liver transplantation is a compex surgery with numerous variables in form of 4 anastomoses:
- Arterial anastomosis
- Venous inflow anastomosis (portal venous system)
- Venous outflow anastomosis ( hepatic vein and/or inferior vena cava)
- Biliary anastomosis
Immunosuppression Post-Liver Transplantation
After liver transplantation, it is important to guarantee both the survival of the transplant and the patient which is achieved by immunosuppression. Different regimens can be used but maintenance is usually with cyclosporine, azathioprine, and prednisone.The first step is to lower the risk of acute rejection by induction therapy. Induction therapy at the time of the transplant includes high-dose corticosteroids and antithymocyte globulin. Tacrolimus, a T-cell proliferation inhibitor, and mycophenolate can be also used as induction therapy.
More recently, it was shown that dual therapy with steroids and calcineurin inhibitors, such as cyclosporine, also works. Additionally, some centers taper-off steroids eventually and the patient ends up on monotherapy with cyclosporine with very little increase in the risk of graft rejection.
In addition to immunosuppresion, prophylactic antibiotics have to be administered such as septrin for respiratory infections, accyclovir for hepatic infections and nystatin drops for candida esophagitis.
Post-Transplant Complications
The most common complication after liver transplantation is acute graft rejection which can happen in up to 70% of the cases and usually in the first two weeks post-transplant. Patients present with jaundice, high bilirubin and alkaline phosphatase levels and the patient could have liver tenderness.High-dose prednisolone or methylprednisolone is the treatment of choice for acute transplant rejection. Fortunately, this regimen is effective in up to 80% of the cases. Less commonly, in 5% of the patients, chronic rejection could happen. In these patients, the usual presentation is a gradual increase in bilirubin and alkaline phosphatase. A liver biopsy would show occlusion of the small bile ducts.
Post-transplant infections are also common in the first month due to severe immunosuppression during this period and bacterial and fungal infections are common. Patients present with cholangitis, or an abdominal abscess, and complain of fever, abdominal pain or are asymptomatic.
After six months of transplantation, the risk of infection becomes similar to the general population. Cytomegalovirus infection is common in the first three months after liver transplantation and treatment includes ganciclovir IV for 2 to 4 weeks.
The risk of malignancy increases with immunosuppression, especially lymphomas and squamous cell carcinoma.
Diagnostic workup for patients with post-transplant complications
Patients who are liver transplant recipients and who present with jaundice, fever, abdominal pain, elevated bilirubin and high alkaline phosphatase are suspected to have liver transplant rejection and should be evaluated and monitored closely. Laboratory investigations include serum bilirubin and liver function tests to evaluate the synthetic and secretory function of the liver. Evaluation of bile secretion in the T-tube bile duct stent should also be attempted.Due to the similarity in symptoms between rejection and infection, blood cultures are indicated to exclude infectious complications. Patients with liver transplantation are immunosuppressed and are at risk of developing opportunistic infections such as pneumocystis carinii pneumonia (PCP), cytomegalovirus infection and candida infestations, and they should be evaluated for that.
A chest x-ray to exclude PCP, and an abdominal CT scan and ultrasonography to exclude intra-abdominal abscesses are indicated.
Useful Information, your blog is sharing unique information.
ResponderEliminarliver transplant
nice.. thanks for sharing...
ResponderEliminarAnyone want to go for Liver Transplantation In India can visit to our site for contact detail.