Asthma (Bronchial Asthma) — Classification, Diagnosis and Treatment
In Lecturio :) - It is the chameleon of pulmonology: With as many different clinical phenotypes, making a diagnosis isn’t always easy, and pathogenesis is complex. In the following article, you will find all the important information about one of the most common chronic diseases in human beings: bronchial asthma.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your immunology course now for free!
Definition of Asthma
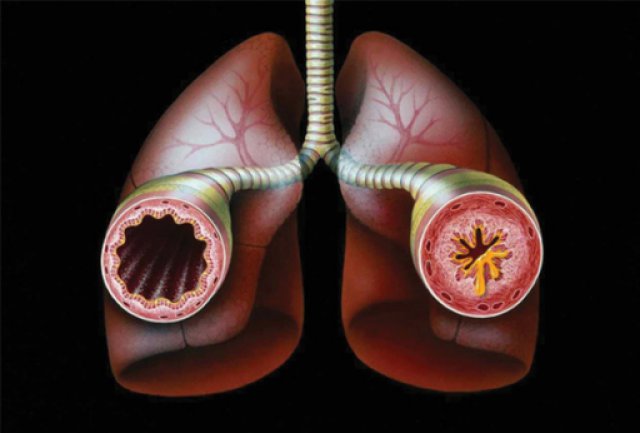
Bronchial asthma as inflammatory disease of the airways
Bronchial asthma describes a chronic inflammatory disease of the airways. During the course of the inflammation, a bronchial hyperreactivity occurs.In comparison to healthy people, the airways of patients with asthma react more sensitive to various stimuli. The consequence is a paroxysmal and recurring obstruction of the airways.
However, this obstruction occurs spontaneously, and with drug treatment, it is completely or partially reversible.
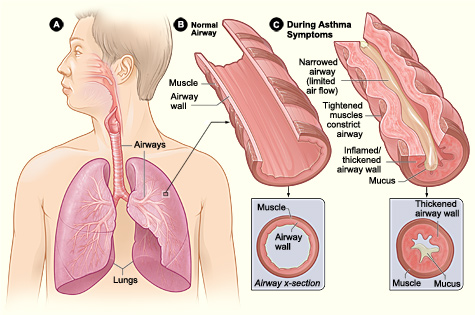
Image: “Figure A shows the location of the lungs and airways in the body. Figure B shows a cross-section of a normal airway. Figure C shows a cross-section of an airway during asthma symptoms.” by United States-National Institute of Health: National Heart, Lung, Blood Institute. License: Public Domain
Epidemiology of Asthma
Bronchial asthma in the population
Bronchial asthma is one of the most common chronic diseases in humans. Around 5 % of adults and even 10 % of children and young people are affected.With regard to gender distribution, different statements can be found in the literature. According to a study by the Robert Koch Institute (Germany), slightly more women than men were affected between 2003 and 2008. Other sources state an approximately equal distribution.
Regardless, it is an undisputed fact that the initial onset of the allergic type of asthma occurs mostly during childhood.
Etiology of Asthma
Causes and triggering factors
Generally, two types of asthma can be distinguished.1. Allergic, extrinsic asthma
Patients with allergic, extrinsic asthma develop asthma symptoms when coming into contact with environmental allergens (e.g. pollen, pet hair, house dust mites, mildews, occupational allergens such as flour dust).The allergic type of asthma often exists in combination with other diseases pertaining to the atopic syndrome, such as allergic rhinitis or neurodermatitis. They all have in common a polygenic predisposition for excessive production of IgE. If both parents are affected by allergic asthma, their children will have a risk of disease of around 60-80 %. On the island Tristan da Cunha, 50 % of the population suffer from asthma due to hereditary transmission.
2. Non-allergic, intrinsic asthma
For non-allergic, intrinsic asthma, the following trigger factors may play a role: respiratory infection (infectious asthma), acetylsalicylic acid/NSAIDs (analgesic asthma syndrome), noxious inhaled agents, gastroesophageal reflux, as well as cold air and physical or mental stress.Often, the two types cannot be rigorously distinguished especially when they occur in adult asthmatics. Only 30 % of patients suffer from a purely extrinsic or intrinsic asthma; the rest display hybrid forms of both types.
Pathophysiology of Asthma
The origin of bronchial asthma
In the case of allergic asthma, only a few minutes after coming into contact with a corresponding allergen, the production of IgE antibodies begins. These antibodies activate mast cells, which release mediators such as leukotriene, prostaglandin, and histamine (type 1 hypersensitivity reaction). These mediators cause bronchospasms, on one hand, and attract inflammatory cells, on the other. The latter eventually cause a long-term full picture of chronic inflammation.In the case of non-allergic asthma, the immunological process is similar but without a triggering allergen. Here, it is for instance substitute infectious agents (especially viruses) that are suspected to act as triggering factors.
All different types of asthma have the resulting pathologic consequences in common:
Constriction of the airways due to bronchospasm, but also due to an oedematous mucosal swelling; hypersecretion of thick mucus (dyscrinism); hyperplasia of smooth muscles (remodeling); in addition, bronchial hyperreactivity and (chronic) bronchial inflammation.
Symptoms of Asthma
Clinical presentations of asthma can differ greatly from patient to patient.The typical main symptoms are:
- Paroxysmal shortness of breath
- Expiratory stridor (differential diagnosis: inspiratory stridor in the event of obstruction of the upper airways!)
- Chronic cough, mostly dry and in spasms (“cough-variant asthma”)
- Thoracic tightness
Note: Also chronic cough without shortness of breath may be a sign of asthma!
Because of the low sympathetic, that is, the high vagal tone in the second half of the night, most patients describe a peak of their symptoms. If symptoms occur seasonally (e.g. during pollination), this might be a sign for allergic asthma.In most cases, the asthma appears only episodically in the beginning, and patients remain symptom-free most of the time.
Attention: During seizure-free intervals, pulmonary function often remains within normal limits. Here, a provocation test can help to confirm a diagnosis!
Diagnostics of Asthma
Medical history and clinical examination of bronchial asthma
First, inquiries about possible risk factors can be made during history: Are there any other atopic medical conditions? Are there more people with asthma in the family? Is the patient exposed to allergic agents at the workplace?During clinical examination, patients often present with symptoms like dyspnea, tachypnea, orthopnea, and an prolonged expiration – especially during an acute attack of asthma. When blood pressure falls by more than 10 mmHg during inspiration, this might indicate a paradoxical pulse.
During auscultation, wheezing, humming, or whistling (especially expiratory) may be observed.
Attention: During an acute attack of asthma with marked pulmonary hyperinflation or emphysema, a patient might present with a “silent chest” – the absence of any audible breath sounds!
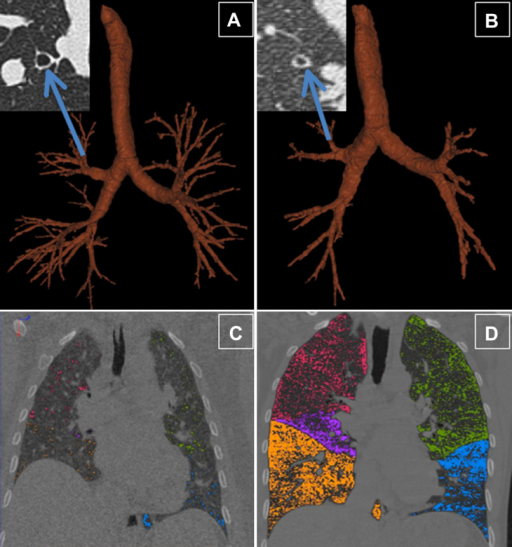
Percussion shows a hyperresonant sound as well as a low position of the diaphragm with reduced mobility during breathing.Pulmunary function tests in bronchial asthma
An essential part of diagnosing asthma is pulmonary function testing.Here, an obstruction with consecutively increased airway resistance can be observed: the forced expiratory volume in 1 second (FEV1) is reduced. Given an approximately constant vital capacity, this yields a reduced Tiffeneau-Pinelli index: FEV1 / VC < 70 %.
A decisive factor in differential diagnosis (e.g. in comparison to COPD) is the reversibility of the obstruction, tested in a bronchodilator reversibility test. The FEV1 value improves significantly either directly after administration of inhaled bronchodilator medication (e.g., 400 µg salbutamol) or in case of a lack of response, after administration of inhaled glucocorticoids over 4 weeks.
As a rule of thumb: If the FEV1 value increases after the bronchodilator test by more than 15 % compared to the initial value, the asthma requires treatment!
If the pulmonary function testing does not show any abnormalities despite suspected asthma, a provocation test (methacholine challenge test) can confirm a diagnosis. The patient inhales methacholine or histamine, and due to the hyperreactivity of the airways, this provokes bronchoconstriction, which leads to a reduced FEV1 value by least 20 % and a doubling of resistance. The following inhalation of salbutamol dilates the bronchial tubes and normalization of the pulmonary function parameters should be achieved.Further diagnosis of bronchial asthma
Since allergic asthma is generally the most common type of this disease, an allergy test should always be administered (especially intradermal or prick testing, determination of total and specific IgE).An ECG can show signs of right ventricular stress.
In the laboratory, eosinophilia might be observed. In addition, in cases of allergic asthma, the IgE is often increased; in cases of non-allergic asthma, leucocytosis as well as increased ESR – and CRP – values may be found.
In an x-ray of the thorax, the overinflated lung can show an increased radiographic transparency, the diaphragm is in a low position and the intercostal space is broadened. The impression of a “barrel chest” arises. Also, the cardiac silhouette is narrowed.
Classification of Asthma
During the initial diagnosis, the asthmatic condition is classified into different degrees of severity:- intermittent
- mild persistent
- moderate persistent
- severe persistent
The German disease management guidelines for asthma have established the following classification:
| Criterion | Controlled asthma | Partly controlled asthma | Uncontrolled asthma |
| Symptoms during the day | ≤ 2 times/week | > 2 times/week | Three or more criteria of the partly controlled asthma are met during one week. |
| Limitation of activities during everyday life | no | yes | |
| Symptoms during the night | no | yes | |
| Use of medication on demand or emergency treatment | ≤ 2 times/week | > 2 times/week | |
| Pulmonary function (PEF or FEV1) | normal | < 80 % of the set point (FEV1) or of the personal best value (PEF) | |
| Exacerbation (asthmatic attack) | no | One or more per year | One per week |
Differential Diagnosis of Asthma
Similar diseases such as bronchial asthma
It is not without reason that the comparison of COPD and asthma is a frequent topic in medical education. Patients very often exhibit similar symptoms. However, treatment options and prognosis differ greatly, which is why an accurate diagnosis is crucial!Already during history, there can be many signs which are more likely an indication for COPD (e.g., smoking, age (> 40 years), gradual onset). The most distinctive criterion is the reversibility of the obstruction of airways during the bronchodilator reversibility test (see section on diagnostics). A complete reversibility rules out COPD!
Additional important differential diagnosis are:
- Cardiac asthma: Patients with left-sided heart failure who have developed a lung congestion with shortness of breath. Bilateral basal rales during auscultation of the lungs and a chest x-ray with signs of pulmonary congestion lead to the right diagnosis.
- Pulmonary embolism with shortness of breath: acute and sudden onset. However, small pulmonary embolisms can also simulate asthma!
- Tension pneumothorax: Watch out for differences between sides during auscultation!
- Inspection: Neck veins may be distended, unilateral diminished of chest movement
- Percussion: the chest is hyperresonant in the affected side.
- Auscultation: decreased or absent breath sounds on the affected side.
- Palpation: the trachea will be deviated away from the affected side.
- Obstructions with other etiology: for instance, aspiration of foreign objects, tumor, glottal edema. An inspiratory stridor during the auscultation is an indication for an obstruction of the upper airways!
Treatments of Asthma
The goal of any treatment should be to reach the controlled form of asthma (see classification). Therefore, depending on the degree of severity, PRN medication (relievers) are used for acute attacks, and if necessary, a long-term therapy with so-called controllers is put in place.This results in a gradual treatment method based on the principle: as much as necessary, as little as possible. The step to a higher level of therapy is taken when the attacks persist in spite of treatment efforts.
The current therapy recommendations according to the guidelines of the GINA (Global Initiative for asthma) reads as follows:
| Level 1 | Level 2 | Level 3 | Level 4 | Level 5 | |
| Long-term therapy | Long-term therapy | ICS low dose | ICS (or LABA) low to middle dose | ICS middle to high dose PLUS LABA | ICS middle to high dose PLUSLABAPLUSOCSlowest effective dose |
| Long-term therapy alternative | ICS if necessary low dose | LTRA | ICS low dose and LTRA or theophylline | PLUS if necessary and LTRA and/or theophylline | Omalizumab if necessary (anti-IgE antibodies) for allergic asthma |
| PRN medication | Inhaled short-acting beta-2 sympathomimetic (salbutamol, fenoterol, terbutalin) | ||||
LABA = Long-acting beta-2 agonists (salmeterol, formoterol)
LTRA = Leuktoriene receptor antagonists (mostly montelukast)
OCS = Oral corticosteroids
For asthma treatment in children, the following applies: montelukast and the mast cell stabilizing cromoglicic acid are preferable to the use of long-acting beta-2 mimetics.
 The above mentioned medications are administered by inhalation mostly using metered-dose inhalers, which are commonly known as “asthma sprays”. It is important to instruct the patient well on how to use the device – only if the medication is inhaled correctly, it can work properly!
The above mentioned medications are administered by inhalation mostly using metered-dose inhalers, which are commonly known as “asthma sprays”. It is important to instruct the patient well on how to use the device – only if the medication is inhaled correctly, it can work properly!A great option for both patient and doctor to get an objective assessment of the therapeutic success is using a peak flow meter.

Image: “Two peak flow meters.” by Hosse. License: Public Domain
Patients should also try to minimize irritations of the airways by:
- Not smoking
- Allergen avoidance
- Avoiding cold air, fog and dust
- Infection prophylaxis and avoiding extreme physical activities
Furthermore, additional patient education concerning the use of inhalation systems, smoking cessation, and respiratory physiotherapy can be considered.
Acute exacerbation
Presentation- Usually known as asthma
- Comes on over minutes to a few hours
- Often preceded by a few days of poor control (e.g. increased nocturnal symptoms, using salbutamol more)
- Frequently there is an obvious trigger (e.g. URTI, stress, smoke exposure)
- Acute dyspnoea, wheeze, cough
- On auscultation widespread polyphonic expiratory wheeze
- Fall in PEFR
- Unable to talk in complete sentences
- High pulse (> 110) and respiratory (> 25) rates
- Pulsus paradoxcus (fall in systolic BP on inspiration)
- Peak flow < 50 % predicted/ previous best
- Low and irregular pulse or respiratory rates
- Reduced blood pressure
- Reduced conscious level
- Quiet breath sounds
- Barely recordable peak flow
- Central cyanosis
- Increasing PaCO2
- Falls in milder attacks
- Normal in more severe attacks
- Naised only in severe disease
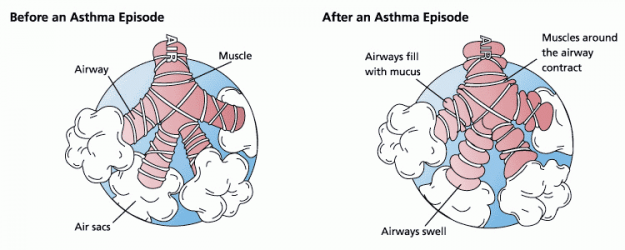
Complications of Asthma
Asthma attacks
An asthma attack is the acute obstruction of the lower airways. When it is life threatening and treatment-refractory, we speak of a “status asthmaticus“. This represents an emergency! The patient has to be brought to the closest hospital immediately by an emergency doctor.
Image: “Animation of the airway (bronchiole) constriction which occurs in an asthma attack. Irritants entering the lung and mucus formation are also shown.” by 7mike5000. License: CC BY-SA 3.0
In addition, the patient should take a supportive body position that facilitates breathing (sitting upright with rested arms) and possibly apply self-help techniques (pursed lip technique, use of the respiratory muscles).
Subsequent treatment management depends on the severity of the asthma attack:
| Severity of the attack | Symptoms | Assistance | Therapy |
| Low to moderately severe | Normal speech RR < 25/min HR < 110/min PEF > 50 % of set point | Waiting fora response to the initial treatment | 2-4 inhalations of a short-acting beta-2 sympathomimetic |
| Severe | Shortness of breath when speaking RR > 25/min HR > 110/min PEF < 50 % of set point | Consider hospitalization | 2-4 inhalations of a short-acting beta-2 sympathomimetic O2 2-4 l/min 50-100 mg of prednisolone equivalent Oral or IV Inhalation of ipratropium bromide |
| Life-threatening | “Silent chest”, frustrane breathing, cyanosis Hypotonia, bradycardia, exhaustion, coma SaO2 < 92 % PEF < 33 % of set point | Immediate hospitalization accompanied by an emergency doctor |
Note: Never administer beta blockers during an acute asthma attack!
Prevention of Asthma
How to prevent bronchial asthma
Especially exposure to smoking during childhood should be prevented. Factors like extended breast feeding, hypoallergenic baby food and reduction of house dust mites, are being considered as preventive measures in academic discussions; however, as of now, there is not sufficient scientific evidence.Review Questions
Solutions can be found below the references.1. Which statement concerning allergic asthma is not correct?
- Initial manifestation normally occurs during childhood.
- The IgE-transmitting hypersensitivity reaction (type I) plays an important role in pathogenesis.
- The methacholine challenge test (provocation test) is usually negative.
- Fenoterol can be used as PRN medication.
- First, a long-acting beta-2 sympathomimetic should be administered.
- The patient should lie down immediately.
- During auscultation, humid rhonchus can be heard.
- The patient should be hospitalized immediately, accompanied by an emergency doctor.
- …measures the expiratory maximum flow in l/sec.
- …measures the Tiffeneau-Pinelli index.
- …is used with inpatients for controlling the therapy of asthma.
- …determines once a year the most important pulmonary function parameters ofa patient with asthma.
Este comentário foi removido por um gestor do blogue.
ResponderEliminarIt was during my research on HIV/Herpes that I stumbled upon the Hiv/Herpes information; information which is quite easy to find when doing a search for STD on google. I was into conspiracy at the time thought of HIV/Herpes Cured' being a conspiracy was something Ignorance though,I found pretty interesting about herbal medicine. I asked questions about the Herbal cure's on official HIV/Herpes websites and I was banned for doing so by moderators who told me that I was parroting Hiv/Herpes propaganda. This reinforced my belief that there is a cure for Hiv/Herpes Then i found a lady from germany name Achima Abelard Dr Itua Cure her Hiv so I send him a mail about my situation then talk more about it and send me his herbal medicine I drank for two weeks.And today I'm Cured no Hiv/Herpes in my life,I searched for Hiv/Herpes groups to attempt to make contact with people in order to learn more about Hiv/Herpes Herbal Cure's I believed at this time that you with the same disease this information is helpful to you and I wanted to do the best I could to spread this information in the hopes of helping other people.That Dr Itua Herbal Medicine makes me believes there is a hope for people suffering from,Parkinson's,Alzheimer’s disease,Bechet’s disease,Crohn’s disease,Cushing’s disease,Heart failure,Multiple Sclerosis,Hypertension,Colo_Rectal Cancer,Lyme Disease,Blood Cancer,Brain Cancer,Breast Cancer,Lung Cancer,Kidney Cancer,Love Spell,psoriasis,Lottery Spell,disease,Schizophrenia,Cancer,Scoliosis,Fibromyalgia,Fluoroquinolone Toxicity Syndrome Fibrodysplasia Ossificans Progressiva.Infertility,Tach Disease ,Epilepsy ,Diabetes ,Coeliac disease,,Arthritis,Amyotrophic Lateral Sclerosis,Autism,Alzheimer's disease,Adrenocortical carcinoma.Asthma, (measles, tetanus, whooping cough, tuberculosis, polio and diphtheria)Allergic diseases.Parkinson's disease,Schizophrenia,Lung Cancer,Breast Cancer,Colo-Rectal Cancer,Blood Cancer,Prostate Cancer,siva.Fatal Familial Insomnia Factor V Leiden Mutation ,Epilepsy Dupuytren's disease,Desmoplastic small-round-cell tumor Diabetes ,Coeliac disease,Creutzfeldt–Jakob disease,Cerebral Amyloid Angiopathy, Ataxia,Arthritis,Amyotrophic Lateral Scoliosis,Fibromyalgia,Fluoroquinolone ToxicitySyndrome Fibrodysplasia Ossificans ProgresSclerosis,Seizures,Alzheimer's disease,Adrenocortical carcinoma.Asthma,Allergic diseases.Hiv_ Aids,Herpe ,Copd,Glaucoma., Cataracts,Macular degeneration,Cardiovascular disease,Lung disease.Enlarged prostate,Osteoporosis.Stroke,
ResponderEliminarDementia.Lung Cancer, Leukemia Lymphoma Cancer,Lung Mesothelioma Asbestos,
Ovarian Cervical Uterine Cancer,
Skin Cancer, Brain Tumor, ,Hiv_ Aids,Herpes,Inflammatory bowel disease ,Copd,Diabetes,Hepatitis,Lupus,I read about him online how he cure Tasha and Tara,Conley,Mckinney and many more suffring from all kind of disease so i contacted him . He's a herbal doctor with a unique heart of God, Contact Emal. ... drituaherbalcenter@gmail.com Phone or whatsapp..+2348149277967.
good post, also refer Wheezing Expert In Jaipur.
ResponderEliminarBuy Asthalin Hfa Inhaler Online USA. Generic Blue Pills provides fast and secure doorstep delivery of Asthalin Hfa Inhaler 100 Mcg at the best price.
ResponderEliminarvisit now : https://www.genericbluepills.com/products/49/asthma-products
TollFree No : +1-678-593-0624