Syphilis — Types, Diagnosis and Treatment
Table of Contents
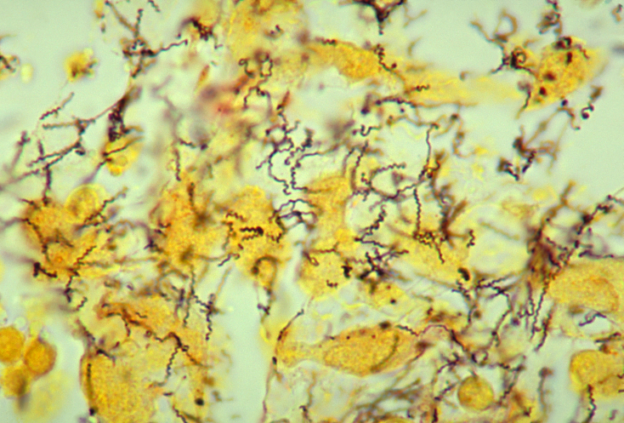
Image: “Histopathology of en:Treponema pallidum spirochetes using a modified Steiner silver stain.” Obtained from the CDC Public Health Image Library. Image credit: CDC/Dr. Edwin P. Ewing, Jr. (PHIL #836), 1986. License: Public Domain
Definition and Background of Syphilis
Syphilis is a chronic systematic disease which is easily treated in its early stages, but neglected cases very often lead to grave consequences and death consequently. Treponema palladium is the causative factor of syphilis described in 1905-1910 by Schaudinn and Hoffman; Wasserman described the blood test for long-term forms of infection.
The first outbreak of the illness was described in 1495 when French soldiers invaded Naples and came down with a deadly disease, which they called “great pox”; the whole Europe was devastated with the sickness with incidences of thousands of death.
During the First World War, syphilis had become a serious reason for the disability and absence from duty in the US Army, over 10,000 men were discharged, and 7 million lost person-days.
This illness has changed names over time: “French disease”, “Spanish fever” so forth. At the beginning, there wasn’t any efficient treatment for syphilis. For this reason, sporadic epidemic outbreaks occurred in different corners of the world.
Mercury was administered by the Esculaps of early medicine as the remedy against this infection; however, this chemical element appeared to be very toxic and became the reason of severe consequences or even death.
Etiology of Syphilis
Pathogenic treponemes are associated with the following 4 diseases:
- Venereal syphilis, caused by T. pallidum pallidum
- Yaws, caused by T. pallidum pertenue
- Endemic syphilis (bejel), caused by T. pallidum endemicum
- Pinta, caused by T. carateum
Ways of transmission
- Sexual contact
- Transplacental/congenital syphilis (vertical way, 50-80% of neonates are exposed to the infection)
- Contact with contaminated blood (while transfusion) and tissues
- Personal contact is a very rare way.
Types of syphilis
- Acquired
- Congenital
Epidemiology of Syphilis
United States
CDC analyzed data obtained from the National Notifiable Diseases Surveillance System (NNDSS), for cases of primary and secondary syphilis diagnosed during 2005–2013 among homosexual, bisexual and other men having sex with men (MSM), the figure accounted for 5.3 cases in 100,000 of population, which is twice as many as it was in the period between 2005 and 2013 (2.9).
The highest prevalence was in Western regions. Among Hispanics (53.4%, from 1,291 in 2009 to 1,980 in 2012) and whites (38.1%, 2,449 to 3,381), when compared with blacks (21.2%, 2,267 to 2,747). By age group, the greatest percentage increases occurred among MSM aged 25–29 (53.2%, 1,073 to 1,644). Nonwhite women tend to contract syphilis more than white females (13,3 times to 4 times accordingly).
International
In the developing world and sub-Saharan Africa as well as in Venezuela, syphilis has become a major public health problem; this illness has no racial predilection, however socioeconomic factors play a pivotal role in the spread of the disease. The highest incidence of Syphilis is observed in South and Southeast Asia, then in Sub-Saharan Africa and third highest in Latin America and Caribbean.
Sex: Men are prone to contract syphilis more frequently than women. Also, syphilis has a strong affiliation with HIV infection, in drug users and those who tend to practice promiscuity in their sexual contacts.
Age: adolescents and young adults are at risk of infection with TP due to their reckless attitude towards sex and drugs.
Clinical Presentation of Syphilis
History
It is vital to collect the whole history of a particular patient in order to determine or assume the stage of the disease: thorough sexual and social history, including the number of sexual partners, condom use, history of STDs in the patient and their partners, intravenous (IV) drug use, and exposure to blood products.
Image: “Primary stage syphilis sore (chancre) on the surface of a tongue.” by Centers for Disease Control and Prevention (CDC) – http://www.cdc.gov/std/syphilis/images.htm#. License: Public Domain
Physical examination
Primary (10-90 days after exposure to the pathogen)
- Hard chancre on genitals
- Painless regional lymphadenopathy
Secondary (4-10 weeks after the first manifestation)
- General: fever, fatigue, pain in joints, sore throat, headache, anorexia, neck stiffness and polylymphadenopaty.
- Skin: red or brown maculopapular non-itchy rash
- Mucosa: patches, “snail track” ulcers on the place of TP penetration.
Late stages (tertiary) occur if there is inappropriate treatment or late administration of the medicines and progresses to tertiary syphilis.
Image: “Rash on the palms of both hands due to secondary syphilis.” by Centers for Disease Control and Prevention (CDC) – http://www2a.cdc.gov/stdtraining/self-study/syphilis/syphilis-sb15.asp. License: Public Domain
- Late benign: gummas (bone and viscera)
- Heart and vessels: affected aorta (inflammation of the wall and regurgitation)
- Neurosyphilis: meningovascular lesion, paralysis of the insane and tabes dorsalis
If without treatment, symptoms and signs adate over 3-12 weeks, in 20% may recur in early latency period (2 years)
Congenital syphilis
Image: “A photograph of Hutchinson’s teeth resulting from congenital syphilis. Hutchinson’s teeth is a congenital anomaly in which the permanent incisor teeth are narrow and notched. Note the notched edges and “screwdriver” shape of the central incisors.” by CDC/Susan Lindsley – http://phil.cdc.gov/phil_images/20021114/34/PHIL_2385_lores.jpg. License: Public Domain
Early stages become apparent between 2-6 weeks after birth.
- Stillbirth or retardation of physical and mental development
- “Snuffles” nasal infection
- Appearance of skin like in secondary syphilis
Late stages become apparent after 2 years age.
- “Stigmata”: abnormalities of long bones, sabre tibia
- Hutchinson’s teeth
- Eyes problems: keratitis, uveitis, facial gummas
- CNS disease
Differential Diagnosis of Syphilis
- Chancroid
- Condyloma acuminata
- Cystitis in females
- Dermatologic manifestations of herpes simplex
- Drug eruptions
- Genital warts in emergency medicine
- Granuloma inguinale (donovanosis)
- Herpes zoster
- HIV disease
- Lymphogranuloma venereum
- Urethritis
- Urinary tract infection in males
- Urinary tract infections in pregnancy.
- Varicella-zoster virus
- Yaws
Diagnosis of Syphilis
Laboratory studies
Imaging studies
- CT as well as MRI detect numerous infarcts in the brain tissue in neurosyphilis.
- X-ray examination is informative when there is severe lesion of the bones suspected.
Staging of Syphilis
Acquired
- Primary syphilis
- Secondary syphilis
- Late (tertiary) stage
- Quaternary syphilis (nowadays extremely rare case owing to appropriate medication and diagnostics)
Congenital
- Early stages
- Late stages
Management of Syphilis
Pharmacotherapy
Surgical intervention
It is not required for the direct treatment unless there are severe complications which lead to the secondary infection of the skin and bone lesions and tertiary syphilis.



Comentários
Enviar um comentário