Developmental Milestones in Newborns: Apgar Score and Low Birth Weight
Table of Contents
APGAR Score
APGAR score recorded at 1 minute provides information about how well the baby has tolerated the process of birth. It also gives insights to the physical health of the newborn and tells whether or not any immediate or future medical treatments are required.
APGAR assessment at 5 minutes provides information on how well the baby is functioning outside their mother’s womb. If previous resuscitation attempts were made, APGAR assessment at 5 minutes determines how well the baby has responded to such attempts. While APGAR score poorly correlates with long-term outcome at 1 minute, it can help in identifying who needs urgent resuscitation. APGAR score at 5 minutes correlates with mortality and morbidity.
The maximum APGAR score is ten (10). Each of the following categories is scored with 0, 1 or 2 based on the criteria given below.
Appearance or Color:
- Most infants will score 1 for color because peripheral cyanosis is seen in almost all newborns
- Score 0 is for the cyanosed or pale skin
- Score 1 is given for pink body and blue extremities
- Score 2 is given if the entire skin of the baby is pink
Pulse:
This is the most important assessment as it can help in determining who needs resuscitation. It needs to be assessed by a stethoscope.
- Score 0 is given if there is no heartbeat present
- Score 1, for a heart rate of less than 100 beats per minute
- Score 2, for a heart rate greater than 100 beats per minute
Grimace response (reflex irritability):
- Score 0, for the absence of any response to stimulation like mild pinch
- Score 1, for minimal response to stimulation
- Score 2, for grimacing, along with one or more of the following:
- Cough
- Sneeze
- Vigorous cry
Activity (muscle tone):
- Score 0, for loose and floppy muscles
- Score 1, for flexed arms and legs
- Score 2, for active motion
Respiration:
- Score 0, if the infant is not breathing
- Score 1, for slow, gasping, weak or irregular respirations
- Score 2, for a vigorous cry
Normal results
The APGAR score lies in the range of 1 to 10. For higher scores, it can be said that the baby is doing better after birth. The full score is usually not seen because almost all the infants lose at least 1 point for the cyanosed hands and feet. However, cyanosis is normal after birth. 7, 8 and 9 score is a determinant of a newborn’s good health. A reasonable score means that the infant needs only the routine post-delivery care.
Abnormal results
Note: Per the most recent the American College of Obstetricians and Gynecologists and the American Academy of Pediatrics guidelines, the need for initial resuscitation must be determined and appropriate interventions need to be carried out before obtaining the 1-minute APGAR score.
An APGAR score of less than 7 is an indication that the newborn is in need of medical attention. The lower the score, the more the help needed to survive outside the womb of the mother. Scores between 4 and 6 indicate the need for breathing assistance, and a score of less than 4 is a call for prompt, lifesaving measures.
A lower APGAR score is not necessarily indicative of long-term health problems. It is not a predictor of the future health of the child.
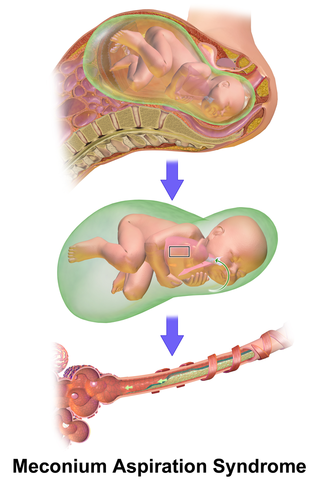
Image: “Meconium aspiration syndrome (MAS),” by Bruce Blaus – Own work. License: CC BY-SA 4.0
Low APGAR score reasons
Common causes for a low APGAR score are:
- Cesarean section
- Difficulty in the birth process
- Meconium aspiration syndrome (MAS)
Medical aid for low APGAR score babies
Low APGAR score babies need the following help:
- Clearing out the airway to assist in breathing
- Placing the newborn in the infant incubator
- Physical stimulation for a healthy heart beating rate
Persistently low APGAR score
If the APGAR assessment at 5 minutes gives a score of less than 7, the test is repeated at 5-minute intervals, four more times. The persistently low APGAR score at 20 minutes of age is related to high morbidity and mortality rates.
The risk of poor neurologic outcomes also increases when the APGAR score is 3—or less—at 10-to-20 minutes of birth. An APGAR score that remains at 0 after 10 minutes might be indicative of terminating resuscitative efforts.
Limitations of APGAR Score
APGAR score limitations are important to recognize. This score is an indication of the physiological condition of the newborn at one point in time. Certain factors can have an impact on the APGAR score, such as:
- Maternal anesthesia
- Gestational age
- Trauma during birth
- Congenital malformations
- Large inter-rater variability. Therefore, the same person who performed APGAR score at 1 minute should repeat any re-assessments
Regular transitional variations may also influence the scores. It is inappropriate to use an APGAR score alone to diagnose asphyxia. Babies rarely get a perfect score on this test. It is not a predictor of a baby’s future behavior or intellect.
Low Birth Weight
When the weight of a baby at the time of birth is less than 2,500 grams, the baby is said to have a low birth weight. There is an epidemiological observation that newborns who weigh less than 2,500g have a 20 times greater chance to die than those babies who are born with appropriate weight.
A birth weight that is less than 1,500 grams (3.3 pounds) is categorized as very low birth weight, and the one below 1,000 grams (2.2 pounds) is considered extremely low birth weight.
What Causes Low Birth Weight?
Low birth weight is commonly seen in cases of preterm delivery, i.e., birth before 37 weeks of pregnancy. The shorter the gestation, the smaller the baby and the higher the morbidity, disability and death risk.
Another cause is intrauterine growth restriction. It may be because of problems with the placenta, the mother’s health or the baby’s health. Babies with intrauterine growth restrictions can be both premature and full term. Low birth weight due to restricted intrauterine fetal growth affects the person throughout life and is associated with poor growth in childhood and a higher incidence of adult diseases, such as type 2 diabetes, hypertension and cardiovascular disease.
Other than premature birth and IUGR, factors that affect the pregnant mother can also increase the chances of having a low-birth-weight baby. Some of these factors are as follows:
- Not gaining enough weight during pregnancy
- Infection during pregnancy
- History of a low-birth-weight baby
- Alcohol consumption
- Drug usage
- A very young mother
- Age more than 35
- African-American background
- Lack of nutrition during pregnancy
- Smoking
- Living in high altitudes
- Malaria, HIV, syphilis during pregnancy
- Hypertension
- Deprived socio-economic conditions
- Physically-demanding work during pregnancy
- Twin babies have a greater chance of being low birth weight
- Genetic factors
Complications of Low Birth Weight
Low-birth-weight babies have tiny bodies, and their rate of growth and development is not always similar to other babies. Low birth weight is often related to neonatal mortality and morbidity, inhibited growth and cognitive development and chronic diseases later in life.
Following are the complications in case of a low-birth baby:
- Image: “Baby in the neonatal intensive care unit.” By Jacoplane (well, his parents anyway) – Own work. License: CC BY-SA 3.0Breathing difficulties at the time of birth
- Hands and feet are usually cold
- Lag on feeding milestones
- Difficulty gaining weight
- Recurrent infections
- Infant respiratory distress syndrome
- Neurological disorders such as intraventricular hemorrhage
- Gastrointestinal problems such as necrotizing enterocolitis
- Sudden infant death syndrome (SIDS)
- Retinopathy of prematurity or Terry syndrome
- Patent ductus arteriosus
Long-term complications in low-birth babies:
These babies may have certain health conditions in later life such as:
- Cerebral palsy
- Blindness
- Deafness
- Diabetes
- Heart diseases
- Developmental delay in both motor and social category
- High blood pressure
- Metabolic syndrome
- Obesity
- Learning disabilities
- Having smaller babies when low-birth-weight girls become mothers
Summary
Low-Birth-Weight Treatment
Treatment depends upon the symptoms, age and general health of the baby. It includes:
- Temperature-controlled bed
- The babies are kept in neonatal intensive care unit (NICU)
- If the baby cannot suck, the feed is given through IV line or a nasogastric tube


Comentários
Enviar um comentário