Bacterial, Viral and Fungal Infections of the Central Nervous System
Table of Contents
Gold Standard Derebrospinal Fluid Examination
Introduction
Meningitis is defined as infection and inflammation of the pachymeninges.
There are various causes of infections meningitis that can be grouped into:
- Bacterial meningitis: The most common cause of meningitis and it is a common disease in the developing world.
- Viral causes of CNS infections: They include herpes and varicella viruses. They can also lead to encephalitis.
- Parasitic causes are very rare due to high hygiene standards as they have been associated with immunosuppression.
The main reason for classification according to etiology is to:
- Differentiate the pathogen classes and thus plan on the therapeutic approach
- For classification purposes and easier diagnosis in future
In our part of the world, you will mostly encounter bacterial and viral causes of CNS infections. Parasitic causes are very rare due to high hygiene standards. Another reason to differentiate the pathogen classes is the therapeutic approach.
The gold standard for diagnosis of meningitis is a lumbar puncture with cerebrospinal fluid (CSF) examination for certain parameters as shown. The following aspects are examined in the fluid:
- Cell count and cell differentiation
- Glucose and protein
- Microbiological pathogen detection: direct pathogen detection with microscopy, PCR, antigen detection and cultivation, and indirect pathogen detection with intrathecal production of antibodies against pathogens
Overview of typical cerebrospinal fluid findings at CNS infections
Table: A. Bender et al.: mediscript Kurzlehrbuch Neurologie. Elsevier Verlag 2013. S. 191, Tab. 7.2
Bacterial Infections of the Central Nervous System
Acute bacterial meningitis
Epidemiology of bacterial meningitis
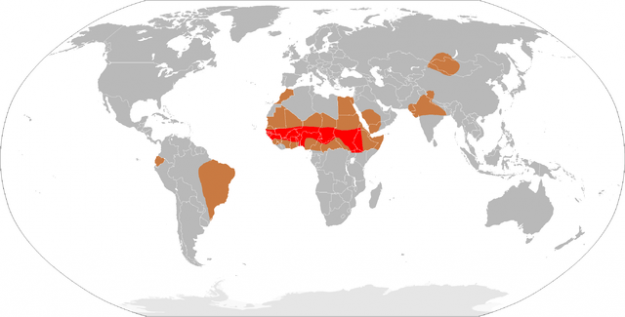
At acute bacterial meningitis, the meninges and the subarachnoid cavity are infected. Incidence in Europe is 2-6 affected people in a population of 100,000. The disease is significantly more frequent in the meningismus belt in the sub-Saharan regions of Africa. With bacterial meningitis, different pathogens are typical for respective age groups, and they undergo empiric antibiotic therapy.
- Newborns: enterobacteria, streptococci, Listeria monocytogenes ⇒ Therapy: cefuroxime and ampicillin
- Children: Streptococcus pneumoniae, Neisseria meningitidis ⇒ Therapy: ceftriaxone
- Adults: Streptococcus pneumoniae, Neisseria meningitidis, Listeria monocytogenes (in > 50-year-olds) ⇒ Therapy: ceftriaxone and ampicillin
Clinical picture of bacterial meningitis
Cardinal symptoms: Headache, neck stiffness, fever, decrease in vigilance (the symptoms do not always occur in this combination!).
Also, patients often show the following symptoms: nausea, vomiting, vertigo and photophobia. One third of the patients display focal neurological deficits like cranial nerve palsies (mostly cranial nerve 3 and 6), sensitivity impairments and speech disorders; one tenth also shows cranial nerve damages. Kerning’s sign and Brudzinski’s sign can be positive (see the article on neurological examination). In infections with Neisseria, skin bleedings in the context of Waterhouse-Friderichsen syndrome are possible.
Diagnostics of Bacterial Meningitis
CSF examination: The examination of the CSF is the diagnostic basis. The pathogens in the CSF can be detected using the Gram stain, CSF cultures, antigen quick tests, PCR and blood cultures. Cases of acute bacterial meningitis produce the following picture (before treatment):
- > 1,000 cells/µL, granulocytes dominate
- Protein and albumin ↑
- Glucose ↓, CSF/serum glucose ratio < 0.3
- Lactate ↑
Blood: The differential blood count mostly shows leukocytosis with left shift, CRP ↑ and procalcitonin ↑.
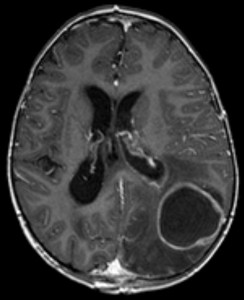
Imaging: The CT of the skull checks for:
- Signs of increased cranial pressure as result of diffuse brain edema or hydrocephalus
- Changes in density due to accumulations of purulence in the ventricles
- Abscesses
- Inflammatory foci in the paranasal sinus and the mastoid
Therapy of bacterial meningitis
Since waiting leads to a worse prognosis, the antibiotic therapy is initiated before final pathogen detection according to the typical pathogens of the respective age group (see above under epidemiology). If the pathogen detection has been made, the antibiotic therapy has to be adjusted. Of course, blood cultures are taken BEFORE medicamentous therapy!
For adults with pneumococcal meningitis, an adjuvant therapy with dexamethasone is currently (as of 2015) suggested. Studies show decreased occurrence of consequential damages like hearing impairment and lethality.
Prognosis of bacterial meningitis
Lethality of bacterial meningitis is high. 20 % of all patients die of infections caused by the pathogens pneumococci and listeria. With S. aureus as the actuator of acute bacterial meningitis, lethality reaches as high as 20—40 %. Possible consequential damages are – among others—hearing impairment, neuropsychological deficits, hemiparesis, epileptic seizures and cranial nerve palsies.
Features of meningococcal meningitis
N. meningitidis is transmitted via droplet infection. In case of suspicion, the affected persons have to be isolated until 24 hours after the start of antibiotic therapy. Contact persons should be treated with a combined chemoprophylaxis consisting of rifampicin, ciprofloxacin/or ceftriaxone in the sense of post-exposition prophylaxis.
Meningococcal meningitis is subject to mandatory reporting at the public health department.
Tubercular meningitis
Epidemiology of tubercular meningitis
The pathogens responsible for tubercular meningitis are mycobacteria out of the Mycobacterium tuberculosis complex. This subacutely or chronically proceeding disease often presents itself as basal meningitis (infectious reaction concentrates on basal cerebral areas, especially the brain stem).
Number-facts for active tuberculosis:
- Worldwide 10 million people
- Germany: 4,500 cases
Clinical presentation of tubercular meningitis
Clinical symptoms of tubercular meningitis are primarily fever, meningismus, headaches,nausea and vomiting. In 50 % of the patients, cranial nerve palsies, disorders in vigilance and confusion syndromes occur. If encephalitis or tuberculomas form, epileptic seizures are also possible.
Diagnosis of tubercular meningitis
CSF examination: pleocytosis with 50-400 cells/µL, protein ↑↑, glucose ↓ (CSF/serum glucose ratio < 0.5), lactate ↑.
Interferon-γ release assays: Blood lymphocytes are stimulated with tuberculosis-antigens. In the case of undergone or current infection, the gained cells produce interferon-γ.
Microbiology: At pathogen detection in CSF with Ziehl-Neelsen stain, Auramin stain, PCR and cultures, acid-fast rods can be found in tuberculosis. Do not wait until the final pathogen detection (like at acute bacterial meningitis) before beginning therapy!
Imaging: Cerebral changes at tuberculosis are often visible in MRI or CCT.
- Hydrocephalus
- Basal contrast agent accumulation
- Masses at CNS tuberculomas
- Ischemic infarction in case of associated vasculitis
Therapy of tubercular meningitis
Involves the use of anti-tubercular medications that take the forms of:
An intensive phase:
It is a fourfold-combination is used as standard therapy. Mostly, it consists of isoniazid,rifampicin pyrazinamide and ethambutol. The drugs are administered under direct supervision for compliance.
Dexamethasone is administered before or together with the initial dose. It has been shown to reduce mortality if properly administered as per the guidelines.
Continuation phase:
Rifampicin and isoniazid are continued for 6 more months and cure must be confirmed before withdrawing the drug.
Prognosis of tubercular meningitis
If no antibiotic therapy is performed, tubercular meningitis mostly ends lethally. If sufficient treatment is performed, lethality is reduced to roughly 20 %. Circa 30 % of the affected people suffer from consequential damages like hydrocephalus, organic brain syndrome, cranial nerve palsies, ataxia and epileptic seizures.
Brain abscess
Etiology of brain abscesses
Image: “Hirnabszess in der MRT” by Hellerhoff. License: CC BY-SA 3.0
A brain abscess is a bacterial abscessing infection of the brain.
Brain abscesses can form in different ways: via transmission of meningeal foci, hematogenic, and iatrogenic in the course of surgical interventions. The responsible pathogens responsible are mostly streptococci, anaerobics, Gram-negative enterobacteria,pseudomonads and S. aureus. With immunodeficiency, fungi and parasites can also be the actuators of abscesses.
Clinical presentation of the brain abscess
Concerning brain abscesses, there is a broad variety of symptoms which can develop over days or weeks. They include:
- Headache
- Fever
- Nausea and vomiting
- Epileptic seizures
- Neurological examination: vigilance impairments, meningismus
Diagnostic of the brain abscess
Laboratory, microbiology and imaging procedures: In laboratory parameters, CRP is mostly increased; CSF examination is not necessary since the findings are too unspecific. More important is the examination of abscess material via bacterial cultivation, PCR and the test for fungi and mycobacteria.
Therapy of the brain abscess
Prognosis of the brain abscess
In case of timely and appropriate therapy, lethality is < 10 %.
Neuroborreliosis
Epidemiology of neuroborreliosis
Neuroborreliosis, triggered by the bacterium Borrelia burgdorferi, which is transmitted by ticks, is one of the most frequent CNS diseases in Germany: 100—50 / 100,000 inhabitants suffer from this disease. The regional dissemination of the infected ticks is very different and should be taken into account for diagnosis.
Clinical features of neuroborreliosis
The symptoms of neuroborreliosis typically proceed in three stages:
Stage I: Formation of erythema migrans: circularly limited skin reddening, which mostly develops ca. 2 weeks after the tick bite. Only half of the patients who reach stage II had erythema migrans.
Stage II: Meningoradiculitis: searing, radicular pain (Bannwarth syndrome), partially radicular palsies, palsy of the facial nerve. Joint involvement, myocarditis, pericarditis and lymphadenosis cutis benigna are also possible.
Stage III: Detection of antibodies against B. burgdorferi in the enzyme-immune-assay. The detection of antibodies has to occur in both the serum and the CSF. The antibodies are not suitable for therapy assessment! The antibodies can circulate in the CSF over the course of months to years after successful antibiosis.
Therapy of neuroborreliosis
Erythema migrans is treated with an oral 14-day antibiosis: amoxicillin, cefuroxime, doxycycline, or penicillin. If neuroborreliosis has reached stage II or III, oral therapy should be performed with doxycycline over 14 days. The alternative is intravenous treatment with ceftriaxone, cefotaxime, or penicillin.
Prophylaxis of neuroborreliosis
If a tick is removed within the first 12 hours after the bite, the risk of borrelia infection is decreased. There is no vaccination against borrelia.
Viral Infections of the Central Nervous System
The most common viruses causing CNS infection are herpes-simplex-virus (HSV), varizella-zoster-virus (VZV), HIV, Ebstein-Barr-virus (EBV) and enteroviruses.
Herpes-simplex-virus-encephalitis
Epidemiology of herpes-simplex-virus-encephalitis
The herpes-simplex-virus-encephalitis is rare, but it has a fulminant course. Incidence amounts to 1/250,000 inhabitants.
Clinic of herpes-simplex-virus-encephalitis
Besides possible aphasia, ataxia, hemiparesis, cranial nerve palsies and visual field deficits, especially these cardinal symptoms of herpes-simplex-virus-encephalitis occur:
- High fever
- Headache
- Personality changes
- Epileptic seizures in 60 %
- NO meningismus
Diagnostic of herpes-simplex-virus-encephalitis
CSF: CSF findings mostly show a typical relation: lymphomonocytic pleocytosis, elevated protein and albumin and non-decreased glucose (see above table concerning typical CSF findings in bacteria and viruses).
Microbiology: With PCR, HSV-DNA is detected in the CSF.
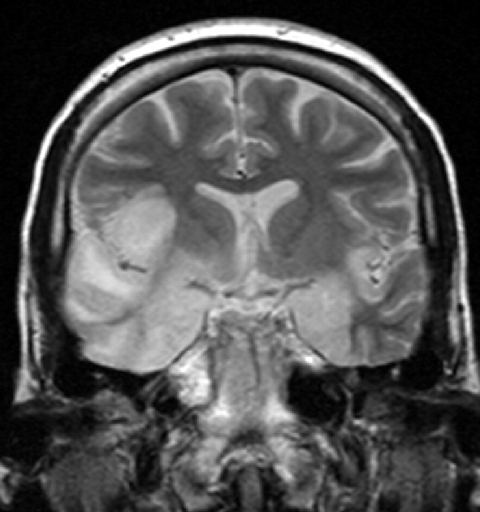
Imaging procedures and EEG: Mostly, the temporal lobe is affected. Necrosis and hemorrhages are typical signs. The EEG often shows temporal slowdowns.
Therapy and prognosis of herpes-simplex-virus-encephalitis
Treatment consists of the intravenous injection of acyclovir five times a day for 14 days. Despite timely introduced therapy, 20 % of all diseased people die. Most survivors suffer from consequential diseases.
Viral meningitis
Epidemiology of viral meningitis
Incidence of viral meningitis is 6-10/100,000 inhabitants. In Germany, mostly enteroviruses are the actuating pathogens. HHV6, VZV, measles viruses, mumps viruses and EBV should also be taken into account.
Clinic of viral meningitis
Viral meningitis causes the typical picture of a meningitic disease: fever, neck stiffness and headache. Often, patients also display flu symptoms.
Diagnostic and therapy of viral meningitis
The CSF findings show the typical picture for viruses with elevated protein and non-decreased glucose levels. Microbiologically, PCR and indirect serological pathogen detections are used.
If viral meningitis is caused by VZV or HSV, treatment with aciclovir is reasonable. If, however, enteroviruses are the cause, only symptomatic treatment occurs.
Herpes zoster: the shingles
Etiology of herpes zoster
If an earlier varizella-zoster-infection (chickenpox) reactivates, herpes zoster develops. This is often an expression of immunodeficiency. However, herpes zoster may also occur in immunocompetent people.
Clinical presentation
Typically, after a painful phase, skin reddening with blister formation in the dermatome of a nerve root sets in. Especially severe are disease courses in facial dermatomes: zoster oticus and zoster opthalmicus. A frequent complication is poster-zoster-neuralgia with pain and allodynia.
Diagnostic and therapy of herpes zoster
Mostly, the diagnosis of herpes zoster is made on the basis of the dermatological picture. Rarely, pathogen detection with blister secretion and biopsy material is used.
The virostatics aciclovir, brivudin, famciclovir or aciclorvir can be used orally for treatment of uncomplicated herpes zoster. In severe cases, intravenous therapy is indicated.
Early summer meningoencephalitis (ESME)
Etiology of ESME
Early summer meningoencephalitis is actuated by the flavivirus, which is – like borrelia – transmitted by ticks. Also, there is a different regional dissemination in Germany.
Clinic of ESME
Early summer meningoencephalitis proceeds in two phases:
- Phase I: 8—10 days after the infection, the patient has flu-like symptoms
- Phase II: 1 week fever-free interval, then vigilance disorders, confusion syndrome, stand and gait ataxia, intention tremor, extrapyramidal symptoms
Diagnostic, therapy and prevention of ESME
Typical for early summer meningoencephalitis is a CSF syndrome with lymphocytic pleocytosis, blood-liquor barrier disorders, positive detection of ESME-IgM and IgG-antibodies, and intrathecal ESME-specific antibody production 2 weeks after disease onset.
At ESME, therapy can only occur symptomatically. People living and working in risk areas should vaccinate.
Progressive multifocal leukoencephalopathy (PML)
Etiology of PML
The pathogen of PML is the JC-virus, which leads to demyelination of white matter at infections. Mostly, the disease occurs due to immunodeficiency, like T-cell-defects. While it almost exclusively affected HIV-patients in the past, PML now also frequently affects people who are medically immunosuppressed due to multiple sclerosis.
Clinic of PML
Depending on the localization of the demyelination focus, symptoms like behavioral problems, cognitive deficits, palsies, visual impairments, vigilance disorders and speech disorders can be observed.
Diagnostic and therapy of PML
JC-viruses can be detected in CSF via PCR. In the MRI, typical signs of PML are confluent demyelination foci without contrast agent accumulation.
Therapeutically, only an improvement of immunocompetence is possible. Antiviral therapy does not (yet) exist. Affected patients with PML do not have a good prognosis: Often, the patients die within two years.
Cytomegalovirus (CMV) infection
CMV-infection occurs in the course of AIDS-disease at very severe immunosuppression. In imaging procedures, the infection shows micronodular changes in the brain and/or hydrocephalus. With PCR, the viruses can be detected in CSF. Concerning therapy, ganciclovir is used.
Protozoa- and Fungal Infections of the Central Nervous System: Facts-Overview
The following overview allows a quick access to facts concerning the most important CNS-diseases caused by protozoa and fungi.
Opportunistic Diseases With HIV
Immunosuppression in AIDS-patients leads to several diseases, which manifest in the CNS. Mostly, the diagnosis of AIDS is made on the basis of so-called AIDS-defining diseases. They occur if certain levels of CD4-cells are undercut.
- CNS-toxoplasmosis (at < 100/µL)
- Primary CNS-lymphomas (no limit)
- Cerebral Cryptococci-infections (at < 100/µL)
- CNS-tuberculosis (no limit)
- CMV-encephalitis (at < 50/µL)
- PML (at < 250/µL)
Review Questions
The answers can be found below the references.
1. Which medicament is not used at neurotuberculosis?
- Isoniazid
- Rifampicin
- Amphotericin
- Pyrazinamide
- Ethambutol
2. The CSF finding presents like this: > 1,000 cells/µl with dominantly granulocytes, protein and albumin ↑, glucose ↓, CSF/serum glucose ratio < 0.3, lactate ↑. For which disease are those parameters typical?
- Cryptococci-meningoencephalitis
- Bacterial meningitis
- CMV-meningitis
- Neuroborreliosis
- Brain abscess
3. Which assignment of typical bacteria, age and treatment is not correct concerning bacterial meningitis?
- Newborns: streptococci group B, cefuroxime and ampicillin
- Children: Streptococcus pneumoniae, ceftriaxone
- Adults: Neisseria meningitidis, ceftriaxone and ampicillin
- Children: Listeria monocytogenes, ceftriaxone
- Newborns: enterobacteria, cefuroxime and ampicillin




I'm here to give my testimony how I was cured from HIV, I contacted my HIV via blade. A friend of my use blade to peel of her finger nails and drop it where she use it, so after she has left i did know what came unto me i looked at my nails, my nails were very long and I took the blade which she just used on her own nails to cut of my finger nails, as i was maintaining my names, i mistakenly injured myself. I did even bother about it, so when I got to the hospital the next week when i was ill the doctor told me that I am HIV positive, i wondered where did i got it from so i remembered how I use my friend blade to cut off my hand so i feel so sad in my heart to the extent that i don’t even know what to do, so one day i was passing through the internet i met a testimony of a lady that all talk about how she was cured by a doctor called DR Imoloa so i quickly emailed the doctor and he also replied to me and told me the requirements which i will provide and I do according to his command, he prepare a herbal medicine for me which I took. He message me the following week that i should go for a test which i did to my own surprise i found that i was HIV negative. He also have cured for all kinds of incurable diseases like: Huntington's disease, back acne, chronic kidney failure, Addison's disease, Chronic Disease, Crohn's Disease, Cystic Fibrosis, Fibromyalgia, Inflammatory Bowel Disease, Fungal Nail Disease, Paralysis, Celia Disease , Lymphoma, Major Depression, Malignant Melanoma, Mania, Melorheostosis, Meniere's Disease, Mucopolysaccharidosis, Multiple Sclerosis, Muscle Dystrophy, Rheumatoid Arthritis, Alzheimer Disease and so many. Thanks to him once more the great doctor that cured me dr. Imoloa so you can also email him via drimolaherbalmademedicine@gmail.com or what'sapp him on +2347081986098.. God Bless you Sir.
ResponderEliminar