Gall Bladder and Bile Ducts – Structure and Function
In Lecturio :) - The gall bladder (Latin: vesica fellea or vesica basilaris) is the storage organ for the bile and has a storage capacity of 40 – 50 ml. On its way from the liver to the duodenum, the bile runs through a duct system which is referred to as the bile ducts. The function of the gall bladder and the bile ducts is an elementary prerequisite for the complex process of digestion and can be impaired by typical diseases which a physician should know and understand. In order to understand the process of digestion, the spleen and the pancreas are also important.
Table of Contents
- Structure of the Bile Ducts
- Location of the Gall Bladder
- Shape and Structure of the Gall Bladder
- Wall Structure of the Gall Bladder
- Blood Supply and Innervation of the Gall Bladder
- Function of the Gall Bladder and the Bile Ducts
- Diseases of the Gall Bladder and Bile Ducts and Their Symptoms
- Examination of the Gall Bladder and the Bile Ducts
- Review Questions
- References
Are you more of a visual learner? Check out our online video lectures and start your anatomy course now for free!
Structure of the Bile Ducts
The bile ducts are usually divided into an intrahepatic (located inside the liver) and an extrahepatic (located outside the liver) part.Intrahepatic bile ducts
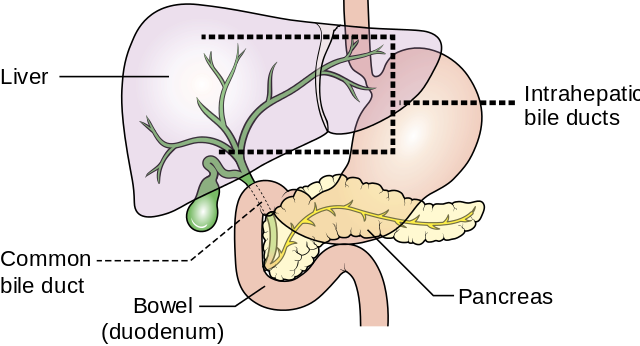
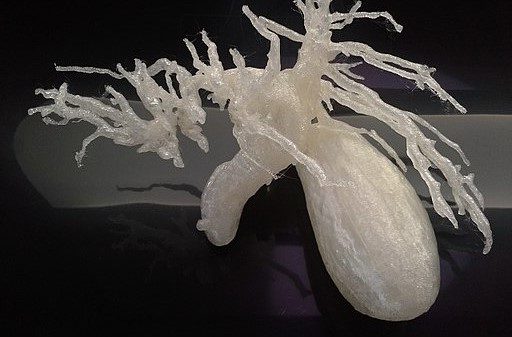
Image: “Diagram showing the position of the intrahepatic bile ducts.” by Cancer Research UK. License: CC BY-SA 4.0
At the edge of a liver lobule, bile reaches small connecting ductules (canals of Hering) and then the interlobular bile ducts (ductuli biliferi interlobulares) in the periportal fields. They have a diameter of roughly 40 µm and run alongside the branches of the portal hepatic vein and the proper hepatic artery as Glisson’s or portal triad.
The bile ducts are lined with an epithelium that can significantly increase the bile’s volume by secretion of bicarbonate and a passively following flow of water. The interlobular bile ducts eventually connect to form the two greater liver ducts, the right and left hepatic ducts.
Extrahepatic bile ducts
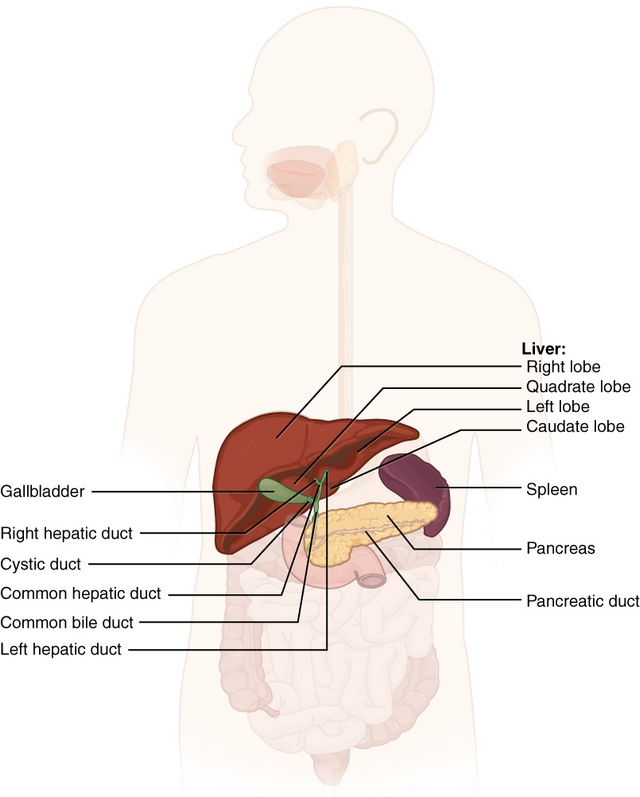
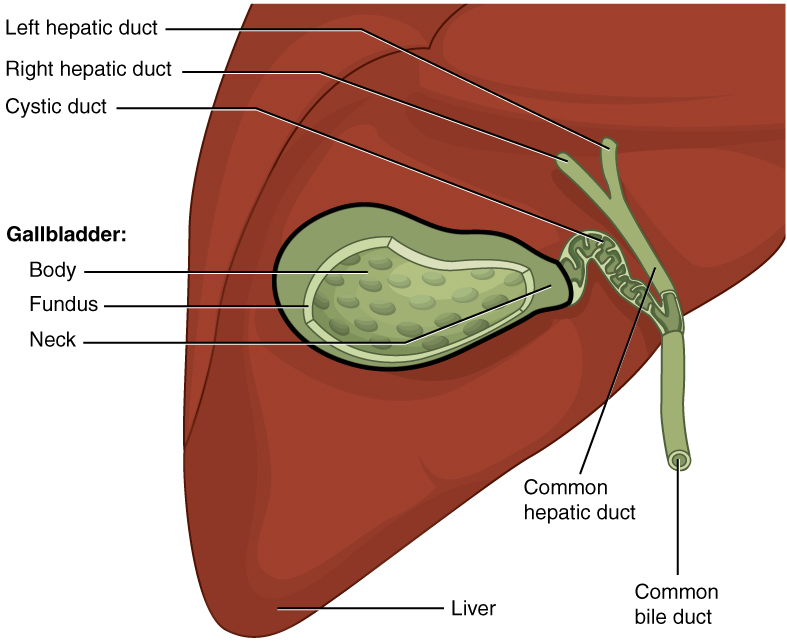
The extrahepatic – that is outside of the liver – part of the bile ducts begins with the fusion of the right and left hepatic duct which forms the common hepatic duct.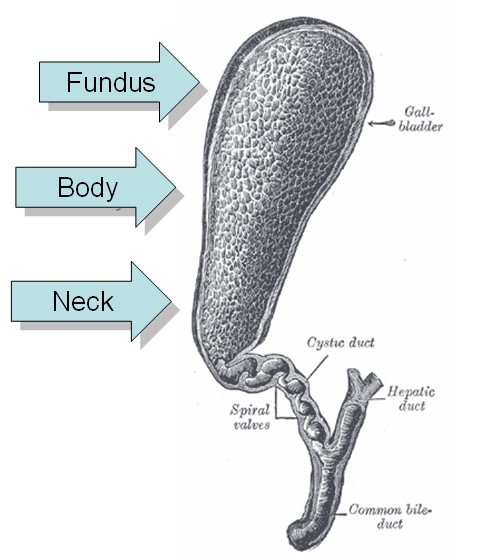
From the liver hilum, it runs roughly 4 cm in the caudal direction at the lower edge of the liver. There, it gives rise to the cystic duct which leads bile to the gall bladder. At this position, the hepatic duct becomes the common bile duct, which runs towards the duodenum for roughly 6cm, inside of the hepatoduodenal ligament.
Note: Often it is asked about the structures running in the hepatoduodenal ligament. Those are the origins of Glisson’s triad: the portal vein, the proper hepatic artery, and the common bile duct.
At its distal end and just before its fusion with the pancreatic duct, the bile duct contains a circular muscle, the sphincter muscle of the bile duct. By contraction, it can ensure an intermediate storage in the gall bladder.When the pancreatic duct connects with the common bile duct, they form a joint ampulla (hepatopancreatic ampulla), which leads to the descending duodenum at the major duodenal papilla (papilla of Vater). The sphincter muscle of the hepatopancreatic ampulla (sphincter of Oddi) consists of smooth muscles and regulates the liberation of pancreatic secretion and bile into the duodenum. The sphincter system which regulates flow of bile and pancreatic juice into the duodenum is completely imbedded into the wall of the duodenum and is an extension of the duodenal musculature.
Location of the Gall Bladder
The gall bladder is situated at the visceral surface of the liver, which faces the abdominal organs. There, it lies in the gallbladder fossa. The gall bladder is located on the level of the ninth rib and borders the right colic flexure with its body.Dorsally, the neck and parts of the body directly lie next to the superior part of the duodenum. The gall bladder shares the peritoneal cover of the liver on the side that faces the intestine and, thus, lies intraperitoneally.
Shape and Structure of the Gall Bladder
In its shape, the gall bladder can be compared to a pear. In length, it measures eight to twelve centimeters and four to five centimeters in width. The gall bladder is divided into three parts:- Neck (collum vesicae biliaris)
- Body (corpus vesicae biliaris)
- Fundus (fundus vesicae biliaris)
Wall Structure of the Gall Bladder
The wall structure of the gall bladder complies with the basic structural scheme of human hollow organs and shows the following layers from inside to outside: tunica mucosa, tunica muscularis, and lamina subserosa.The tunica mucosa protrudes into the lumen with mucous folds due to a layer of connective tissue. When the gall bladder fills up, these folds flatten and thus give the organ great elasticity. Sometimes, deep Rokitanski-Aschoff sinuses can be found. Characteristic of the mucosa of the gall bladder are mucous bridges, which can be explained by the contact of the mucous folds with one another.
The lumen of the gall bladder is lined with simple columnar epithelial cells with microvilli and tight junctions. Via Na+-reabsorption and a passive fluid flow, these epithelial cells function is to concentrate bile. The lamina propria of the mucosa consist of collagenous connective tissue, elastic fibers, and blood vessels that supply the mucosa.
The muscular tunica consists of smooth muscles in a sliding grill-like arrangement. Via contraction, the gall bladder is emptied into the bile duct.
Facing the liver, the outermost layer is the lamina subserosa, a connective tissue layer, which merges with the fibrous capsule (Glisson’s capsule) of the liver. Facing the intestine, it corresponds to the serous tunica (peritoneum).
Blood Supply and Innervation of the Gall Bladder
The arterial supply of the gall bladder is provided by the cystic artery, which originates from the right ramus of the proper hepatic artery. The cystic vein leads to the portal vein at the hepatoduodenal ligament.The vegetative innervation originates from the hepatic plexus, which receives fibers from the coeliac plexus. A parasympathetic stimulation increases the otherwise hormonally controlled contraction of the gall bladder muscles and relaxes the sphincter muscles.
The peritoneal cover of the gall bladder is innervated by the phrenic nerve. The segment C4 also innervates the shoulder, which explains the development of shoulder pain after removal of the gallbladder.
Function of the Gall Bladder and the Bile Ducts
First of all, the gall bladder is an intermediate storage for the bile while it is not needed in the small bowel. In physiological conditions, the gall bladder can reach a volume of 40-50 ml.Bile is highly concentrated in the gallbladder, where the mucosa actively absorbs Na+ and water. This way, bile can reach five to ten times its original concentration. This ‘thickened’ bile is referred to as bladder bile.
To prevent unintentional emptying of the gall bladder at high abdominal pressures, e.g. at defecation, there is the Heister’s valve at the transition from the neck of the gall bladder to the bile duct. This is a sequence of helically arranged mucous folds that can seal the exit of the gall bladder.
Mainly responsible for the release of the bile is the hormone cholecystokinin (CCK), which is produced by enteroendocrinal cells of the intestinal mucosa of the duodenum and is released when the chyme is rich in fats and amino acids. The hormone causes a contraction of the muscular tunica of the gall bladder, which presses the stored bile through the cystic duct, back into the bile ducts.
By relaxation of the sphincter muscle of the bile duct (sphincter of Oddi), the bile follows the lowest drainage resistance into the descending part of the duodenum. Mediated by acetylcholine, the vegetative nervous system has a similar effect. The hormone secretin, which also originates from the small bowel, directly stimulates secretion in the liver and thus increases the production of liver bile.
When the bile finally reaches the duodenum at the major duodenal papilla, it is an important factor for lipid absorption since bile acids and phospholipids form micelles with the fats of the food. Those micelles can be absorbed by the intestinal mucosa.
To minimize the synthetic expense, the important bile acids are re-absorbed in the terminal ileum. Via the portal vein, they are transported back into the liver. This is referred to as the enterohepatic circulation.
Diseases of the Gall Bladder and Bile Ducts and Their Symptoms
The function of the gall bladder and the bile ducts can be disturbed by some typical and frequently interrelated diseases. The following selection of the most important pathologies provides you with an overview.Cholelithiasis – Bile Duct Stones
The impairment of excretion of bile by concretion (bile-duct stones) is referred to as cholelithiasis. In the intrahepatic bile ducts, this is called hepatolithiasis, while concretion in the bile duct is called choledocholithiasis. However, the most common location is the gall bladder, which is called cholecystolithiasis.
Image: “Unauffälliger Gallen- und Pankreasgang, mehrere unterschiedlich große Gallensteine in der Gallenblase und im Gallenblasengang” by J. Guntau. License: CC BY-SA 3.0
Patients do not show symptoms until a stone leaves the gall bladder and becomes lodged in the neck of the gallbladder, within the cystic duct or in the common bile duct, obstructing the flow of bile. Then, they primarily suffer from colicky pain in the right upper quadrant, nausea and vomiting a few hours after ingesting a fatty meal.
A gallstone can best be diagnosed with sonography where it can be seen by sonic shadowing.
Note: The 6xF rule for risk factors: female, fat, fertile, forty, fair, family
Cholecystitis – Inflammation of the Gall Bladder
Cholecystitis is the inflammation of the gall bladder and is based on cholecystolithasis in 90% of the cases. Through bile stasis, the mucosa is damaged and secondarily infected by ascending intestinal bacteria.Patients suffer from pain in the right upper abdomen with radiation into the right shoulder and scapula. Often, they have fever and sometimes jaundice.
On sonography, a thickening of the wall of the gall bladder can be seen. Typical for this disease is the triple layering due to a wall edema. Treatment involves surgical removal of the gall bladder via a laparoscopic cholecystectomy.
Note: Examiners often ask for Murphy’s sign, which is positive at a sudden stop of inspiration at palpation of the right upper abdomen.
Icterus – Jaundice
Icterus (jaundice) is the manifestation of hyperbilirubinemia which is an increase in bilirubin in blood with excretion of bile colorants from the blood into tissue.Initially, an icterus can be seen in the sclera (scleral icterus). In more severe cases, it can also be seen on the whole skin of the patient. Types of icterus are differentiated depending on the location of the impairment:
- Prehepatic icterus develops due to excessive production of bilirubin.
- Hepatic icterus develops due to disturbance within the liver cell.
- Posthepatic icterus develops due to mechanical drainage impairment in the bile ducts like a stone occluding the common bile duct.
Other severe diseases of the gall bladder and the bile ducts are gall bladder cancer and cancer of the common bile duct. Newborns may be born with a condition called biliary atresia in which the biliary system is hypotrophic or absent.
Examination of the Gall Bladder and the Bile Ducts
| Palpation | The healthy gall bladder is not palpable. In case of drainage impairments, the gall bladder can bulge and be palpated under the right costal arch. If not associated with pain, this is called a positive Courvoisier’s sign. Courvoisier’s law (or Courvoisier syndrome, or Courvoisier’s sign or Courvoisier-Terrier’s sign) states that in the presence of a palpably enlarged gallbladder which is nontender and accompanied with mild painless jaundice, the cause is unlikely to be gallstones and more likely to be cancer. |
| Sonography | The ultrasound-examination of the gall bladder is an easy, quick, and widely available diagnostic method and allows the assessment of size, wall texture, and potentially presence of stones in the gall bladder. |
| ERCP | ERCP (endoscopic retrograde cholangiopancreaticography) is an endoscopic examination method to show the bile ducts, the gall bladder, and the pancreatic ducts using contrast agents. The bile ducts are accessed retrogradely from the duodenum. The advantage of the examination is that therapy can simultaneously occur via the endoscope. On the other hand, this invention still has an overall complication rate of roughly 10 %. |
Review Questions
The solutions can be found below the references.1. Which of the following statements is true concerning the bile?
- The liver bile has a higher concentration of bile acids than the bladder bile.
- The bile is transported to the gall bladder through the common bile duct.
- The bile enters the duodenum at the minor duodenal papilla.
- The emptying of the gall bladder is mediated by the hormone CCK.
- The sphincter of Oddi is the sphincter muscle of the cystic duct.
- Age > 40 years
- Smoking
- Obesity
- Female gender
- Fair skin
- Often, patients with cholecystitis have pain in the right shoulder.
- Gallstones can most frequently be found intrahepatically.
- Mostly, icterus can initially be seen at the sclera.
- The gall bladder roughly has a size of 10cm x 5cm.
- The gall bladder is located in the drainage area of the hepatic portal vein

Comentários
Enviar um comentário