Anatomy of the Respiratory System and the Respiratory Muscles
Table of Contents
Respiratory System: Function and Structure
The respiratory system is a series of organs that function as a whole to oxygenate the body by inhaling air and exhaling carbon dioxide. There are three major parts of the respiratory system: the airways, the lungs, and the muscles of respiration.
Respiratory muscles
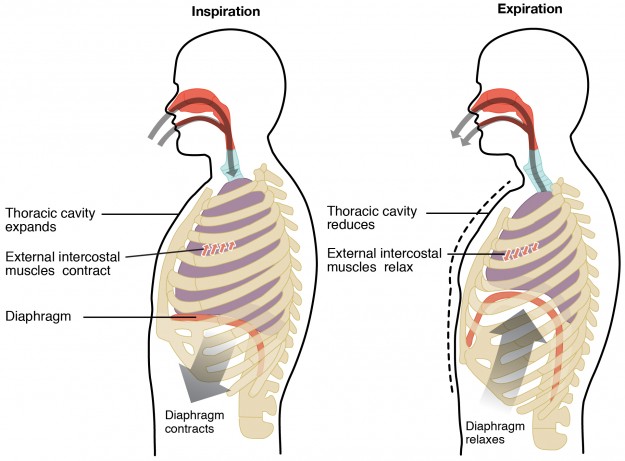
The muscles of respiration are those muscles that are necessary in order to reverse the pressure relations for inspiration and expiration. By means of contraction, they can actively increase the thoracic volume (inspiration) or decrease it (expiration) by passive relaxation. The diaphragm and the intercostal muscles drive respiration during quiet breathing.
Respiration
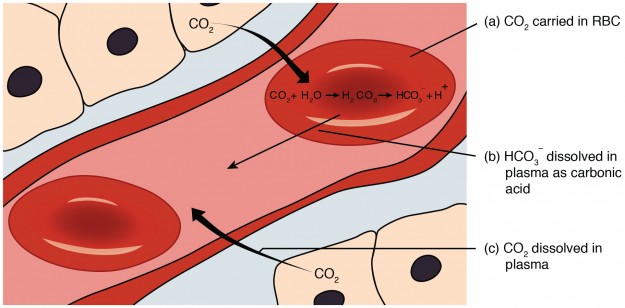
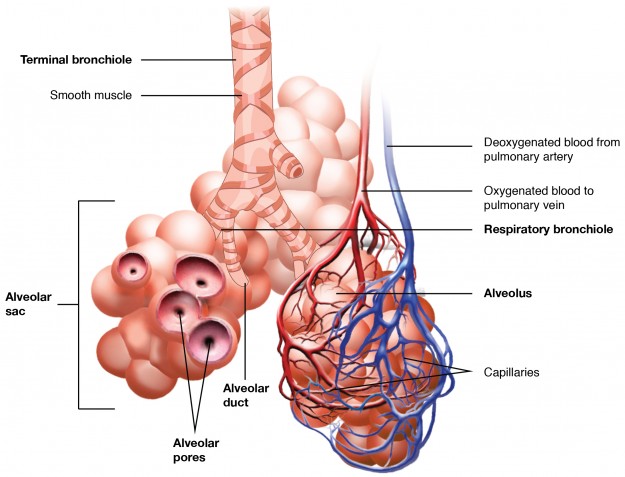
Respiration, in the narrower sense, usually refers to external respiration, and is also called pulmonary respiration. Besides the actual gas exchange between alveoli and lung capillaries, the term refers to the provision and removal of gasses via blood and air; therefore, respiration consists of three components, which span over the whole process.
- Ventilation of the alveoli
- Perfusion of the capillaries
- Diffusion: gas transport and exchange via the membrane
For gas exchange, the air of the environment has to be exchanged in the alveoli, which corresponds to their ventilation. This is realized by the alternating built up of pressure differences between the surrounding air and the lungs so that respiratory air can flow in (inspiration) and out (expiration).
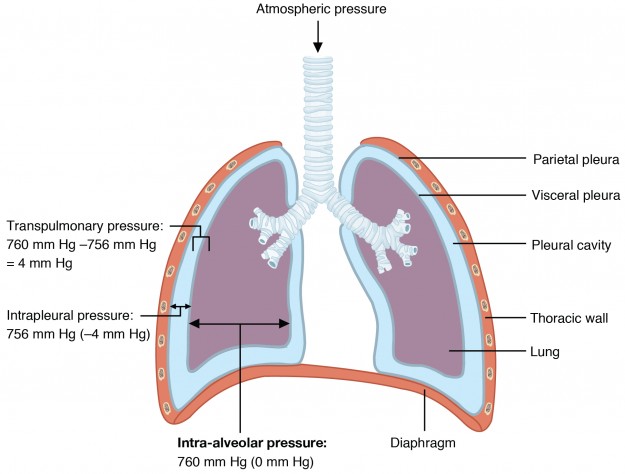
The lung follows the movements of the thoracic wall due to the negative pressure in the pleural cavity (Donder’s low pressure). This pressure acts against the elastic retraction forces of the lung, which would contract otherwise.
Related video
Inspiration
For inspiration, the fresh and oxygen-rich air from the surroundings is transported into the alveoli where gasses are exchanged. The ‘sucking in’ of air into the lungs is facilitated by the intrapleural pressure that is lower compared to the surroundings. As mentioned above, the active forces of the respiratory muscles and the negative pressure in the pleural cavity are responsible for the generation of this negative pressure.
At inspiration, the thorax widens, the pressure decreases, the lungs expand, and air flows in.
More specifically, the following structures are part of inspiration:
- Respiratory muscles: diaphragm (see below).
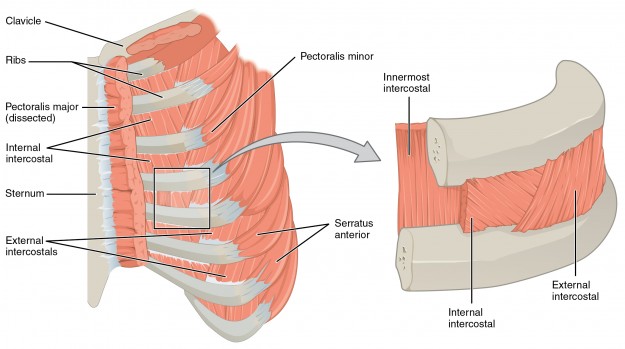
- External intercostal muscles: These muscles obliquely run from one rib to the next one in a ventral to caudal direction. Along with the internal intercostal muscles and the ribs, they form the chest wall. The contraction of the external rib muscles elevates the ribs and expands the thorax. These muscles support inspiration. The external thoracic fasciacovers the muscle from the ventral direction.
- Accessory respiratory muscles:
Sternocleidomastoid muscle
In its course, this muscle divides the neck into two triangles, the posterior triangle of the neck and the anterior triangle of the neck. The muscle is divided into a lateral head and a medial head. The origin of the lateral head is at the clavicle; the medial head originates from the manubrium of the sternum.
In the middle of the neck, the two heads form a thick round muscle belly. The insertion of the sternocleidomastoideus muscle is at the lateral side of the mastoid process of the temporal bone. The innervation occurs via the accessory nerve and branches of the cervical plexus (C1 – C3/4).
Scalenus anterior muscle
The origins of this muscle are the anterior tubercles of the transverse processes in the area of the 3rd to the 6th cervical vertebrae. It runs obliquely in caudal direction and inserts at the tubercle of the scalenus anterior muscle of the first rib. The innervation occurs via the anterior branches of the spinal nerves in the area C5 – C7.
When there is bilateral contraction and the cervical spine is fixed, the muscle elevates the first rib and therefore expands the thorax.
Scalenus medius muscle
From the origin at the transverse processes of the cervical vertebrae 3 – 7, the scalenus medius muscle runs to the first rib, occasionally also to the second rib. Innervation is provided by the spinal nerves of segments C4 – C7. At bilateral contraction, the muscle elevates the upper ribs and expands the bony thorax this way.
Scalenus posterior muscle
The muscle originates from the posterior tubercles of the transverse processes of the cervical vertebrae 5 – 6. From this location, the muscle fibers run to the outer surface of the second rib or the third rib. Innervation occurs via the anterior branches of the spinal nerves of the segments C7 and C8. At bilateral contraction, this muscle also supports the elevation of the bony thorax.
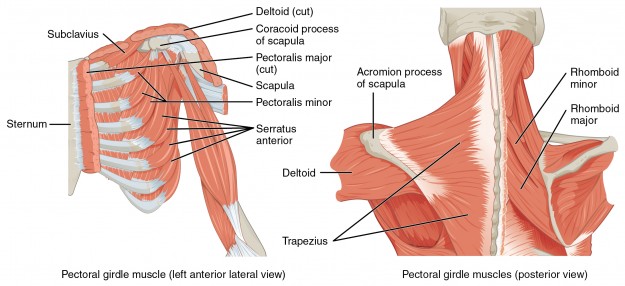
Pectoralis major muscle
The strong, a real ‘greater chest muscle’ lies on top of the pectoralis minor muscle. It is one of the chest muscles and connects the ventral shoulder girdle with the torso. Because of its large extensions, it is topographically divided into three parts:
- Clavicular part: origin at the medial clavicle
- Sternocostal part: origin at the ipsilateral edge of the sternum and the cartilage of the 2nd– 6th rib
- Abdominal part: origin at the anterior sheet of the aponeurosis of the rectus abdominis muscle
The fibers of all three parts merge into a flat tendon, which inserts at the crest of the major tubercle of the humerus. The tendon consists of two twisted laminae (layers). At an elevation of the arm, this twist is reversed.
Innervation is provided by the medial pectoral nerve (C8 – Th1) and the lateral pectoral nerve(C5 – C7) of the brachial plexus. Along with the minor pectoral muscle, it serves as a supporting respiratory muscle.
Pectoralis minor muscle
The ‘lesser chest muscle’ originates from the ventral surfaces of the 3rd – 5th rib and runs cranially and laterally. As a flat tendon, it inserts at the cranial surface of the coracoid processof the scapula.
It is innervated by the medial pectoralis muscle (C8 – Th1) and the lateral pectoral muscle (C5 – C7) of the brachial plexus. The fibers of the muscle serve as a supporting respiratory muscle.
Superior posterior serratus muscle
This muscle is part of the migrated back muscles, which are innervated by the anterior rami of the spinal nerves (Th2 – Th5). It originates from the spinous processes of the 6th – 7th cervical vertebrae and those of the first and second thoracic vertebrae.
The serrated muscle fibers insert at the 2nd/3rd – 5th rib, lateral of the costal angle. Contraction elevates the ribs and thus supports inspiration.
Inferior posterior serratus muscle
As a migrated back muscle, it is also innervated by the anterior rami of the spinal nerves (Th11- L2). It originates from the spinous processes of the last two thoracic vertebrae and the first two lumbar vertebrae. They insert at the 9th – 12th rib.
In contrast to the superior posterior serratus muscle, the fibers run upwards. Bilateral contraction moves the lower ribs dorsally and caudally, which leads to narrowing of the thorax and, thus, actually supports expiration.
Support of inspiration and expiration by the lower ribs is related to the contraction of the diaphragm. When the diaphragm contracts, the pleural pressure falls, exerting a caudal and inward force on the entire rib cage. However, the diaphragm also exerts forces in the cranial and outward direction on the lower ribs.
One of these forces, the “insertional force,” is applied by the muscle at its attachments to the lower ribs. The second, the “appositional force,” is due to the transmission of abdominal pressure to the lower rib cage in the zone of apposition. In the control condition at functional residual capacity (FRC) is the volume of air present in the lungs at the end of passive expiration, the balance state between inspiration and expiration when both forces are balanced at equal pressures.
The effects of these two forces on the lower ribs are nearly equal and outweigh the effect of pleural pressure, whereas, for the upper ribs, the effect of pleural pressure is greater. According to this, the lower ribs counter the cranial and ventral tension of the diaphragm, which would not be favorable for the expansion of the lungs.
Anterior serratus muscle
This muscle is part of the chest muscles and also connects the shoulder girdle to the torso. It is divided into three parts.
- Superior part: Origin 1st – 2nd rib, insertion at the scapula, which is responsible for the elevation of the shoulder.
- Intermediate part: Origin at the 2nd – 3rd rib, insertion at the medial edge of the scapula, which is the major part of the muscle and pulls the scapula ventrally.
- Inferior part: Origin 4th – 9th rib, insertion at the medial edge and the inferior angle of the scapula; allows elevation of the arm.
The innervation of all three parts is ensured by the long thoracic nerve of the supraclavicular part out of the brachial plexus (C5 – C7). If the arm is fixed, it serves as a supporting muscle for inspiration.
Role of the diaphragm in inspiration
75 % of the respiratory performance of the body can be attributed to the diaphragm; it, therefore, represents the most important respiratory muscle in the organism of mammals. Topographically, the 5mm thick dome-shaped muscle plate is located between the thorax and the abdomen.
The muscle originates from the lumbar spine, the sternum, and the ribs. The two domes reach into the thorax and are covered by connective tissue. In the thorax, the diaphragm is additionally covered by pleura and, in the abdomen, by peritoneum. Due to physiology, the right dome protrudes 1 – 2 cm higher into the thorax than the left dome. This morphology determines its asymmetric appearance.
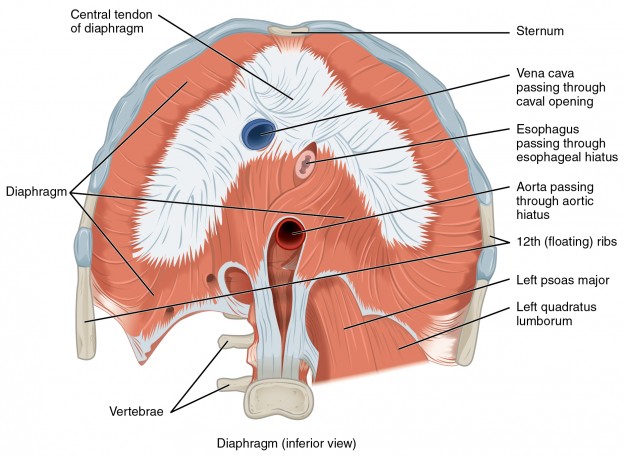
Anatomy of the diaphragm
The diaphragm is located at the inferior-most aspect of the ribcage, filling the inferior thoracic aperture. It acts as the floor of the thoracic cavity and the abdominal cavity. It has three attachments:
- Lumbar vertebrae and arcuate ligaments.
- Costal cartilages of ribs 7-10 (attach directly to ribs 11-12).
- Xiphoid process of the sternum.
In the center of the diaphragm, there is a tendinous plate, which has a V-shaped structure. Important structures pass through this area of the diaphragm: the inferior vena cava, the azygos vein, the phrenic nerve, the esophagus, the aorta and the thoracic duct.
Morphologically, the diaphragm has three major and several lesser openings through which the mentioned structures pass. The major openings are the aortic hiatus, the caval opening, and the esophageal hiatus. The aortic and esophageal fissures are only loosely kept open by connective tissue, which makes for easy sliding when the diaphragm is fully contracted.
- Esophageal hiatus (hiatus esophagus): Esophagus, vagal nerve (anterior/posterior vagal trunks), left gastric artery and vein, and lymphatic vessels run through this orifice. Surrounded by muscles, this orifice is narrowed at inspiration (contraction of the muscle), a motion that inhibits the occurrence of reflux.
- Caval opening (foramen vena cavae): In the shape of a firm ring of connective tissue, the vena cava is grown together with the diaphragm. This way, it is not compressed when the diaphragm contracts. Besides the inferior vena cava, the right phrenic nerve also runs through this orifice.
- Aortic hiatus (hiatus aorticus): Again, a firm tendinous arch for stabilization of the opening inhibits narrowing at inspiration. The aortic hiatus also contains the thoracic duct and the azygos vein.
The major and minor splanchnic nerves, the superior epigastric vein, the left phrenic nerve, the hemiazygos vein, and the sympathetic trunk run through the minor orifices.
The following structures take care of the provision of nutrients and nervous control:
- Arteries: abdominal aorta, internal thoracic arteries, left and right phrenic arteries.
- Veins: left suprarenal vein and azygos system
- Nerves: phrenic nerve with origin in the cervical segment (cervical plexus C3 – C5)
Diaphragmatic respiration
The muscle contracts for inspiration; for expiration, it relaxes. This is controlled by the autonomous nervous system via the respiratory centers in the medulla oblongata and pons, and occurs involuntarily.
During inspiration, the lungs expand, and the volume of the thorax increases at the expense of the abdominal volume. The diaphragm becomes flatter, lowers in the caudal direction, and also pushes the abdominal organs caudally. The abdominal space protrudes.
The tidal volume during relaxed inspiration is roughly 500 ml. Expiration is accompanied with the relaxation of the diaphragm. During this process, the diaphragm elevates, the air leaves the lungs, and the protruded belly flattens and returns to its original dome shape.
The diaphragm does not only manage the major part of the respiratory performance, it also acts as the abdominal press in collaboration with the abdominal muscles. This press is necessary for the processes of birth and defecation.
Diseases of the diaphragm
Those are possible diseases of the diaphragm:
- Side Stitches: Side stitch is an intense stabbing pain under the lower edge of the ribcage that occurs while exercising. This is believed to be because this is a referred site of pain for the diaphragm via the phrenic nerve. Mostly, they occur in the initial phases of physical performance. They result from overloading and simultaneous oxygen deficiency.
- Diaphragmatic hernia: This disease is usually congenital and manifests as a cranial shifting of abdominal organs into the thoracic space. Symptoms like bloating, dyspnea and nausea can be caused by the disease. In most cases, it can be treated surgically.
- Diaphragmatic elevation: Impaired inspiration, in combination with protrusion of the diaphragm into the thorax, indicates diaphragmatic elevation. It is often caused by abnormal changes in the abdominal space or lung diseases. The paralysis of a hemidiaphragm, caused by damage to one of the phrenic nerves, may lead to dyspnea and respiratory failure.
Diaphragmatic paralysis: It is caused by an interruption in its nerve supply due to damage caused by mechanical trauma, compression by a tumor inside the chest cavity, Myasthenia gravis, and diabetic neuropathy. It is generally asymptomatic in case of unilateral diaphragmatic paralysis. It may lead to dyspnea and fatigue.
A special case is the hiccups:
Mostly, hiccups occur suddenly and unexpected. It is the involuntary cramp-like contracting of the diaphragm caused by an irritation of the phrenic nerve. Inspiration is abruptly interrupted by the closure of the vocal folds, which causes the characteristic inspiration sound (‘hics’). Prolonged attacks are serious happening with morbidity and can cause even death.
The purpose of this strong reflectory inspiration movement remains unknown. Often, hiccups are the consequence of hasty eating, smoking, nervousness and hot or cold beverages.
Besides these harmless triggers, there also are pathological causes that lead to chronic hiccups; they can be a sign of other diseases, like disorders of the CNS (subarachnoid hemorrhages, tumors, and encephalitis), impairments of the phrenic nerve (cardiac infarction), and/or impairments of the diaphragm (stomach ulcer, pleuritis, gastroesophageal reflux diseases, pancreatitis). Treatment is usually symptomatic.
Expiration
In the process of expiration, deoxygenated air that has been loaded with carbon dioxide and deprived of oxygen in the gas exchange that occurred in the alveoli is released to the outside. The lung becomes smaller and a higher surrounding pressure is built up. Thus, air flows out.
Expiration involves the diaphragm, the intercostal muscles, and the accessory respiratory muscles:
- Diaphragm: It elastically collapses and allows for the recoil of the lungs.
- Intercostal muscles: The internal intercostal muscles contract, lower and reduce the diameter of the thorax.
- Accessory respiratory muscles:
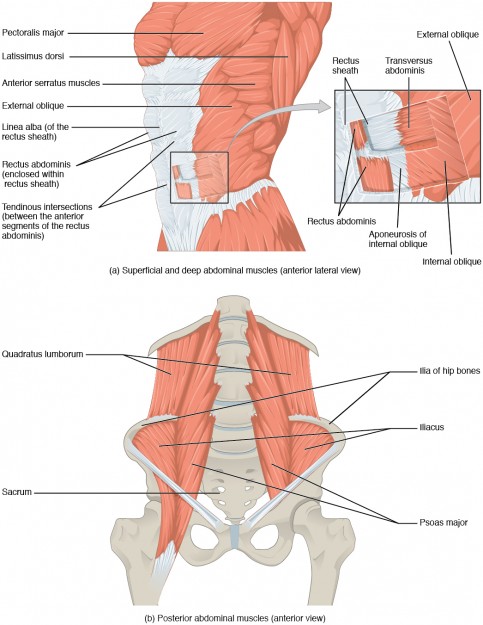
Rectus abdominis muscle
This paired, long and vertically running skeletal muscle belongs to the abdominal muscles. Its origin is at the anterior surface of the fifth, sixth and seventh rib. The right and left muscles meet at the white line (linea alba) and insert at the superior ramus of the pubic bone and at the ligaments of the pelvic symphysis. A particularity is the fact that the rectus abdominis muscles are completely divided by three intermitting tendons (intersectiones tendineae) and partially by a fourth one. These tendons divide the muscle into segments.
Two broad tendinous sheaths surround the muscle completely on both ventral and dorsal side, forming the so-called rectus sheath. In athletically trained persons with little subcutaneous fat tissue, the muscle relief can be seen on the body surface as the notorious six-pack.
The innervation of this muscle is supplied by the anterior rami of the 7th – 12th thoracic or intercostal nerves (Th7 – Th12) and the first and second lumbar nerves (L1 – L2). The arterial supply is provided by the superior epigastric artery and the inferior epigastric artery.
The rectus abdominis muscle increases the tension of the abdominal wall, and together with the pelvic floor muscles and the diaphragm, it increases the pressure in the abdomen.
Transversus abdominis muscle
The fibers of this innermost muscle run mostly horizontally and originate from the inner surface of the eleventh and twelfth rib, the iliac crest, the inguinal ligament, the thoracolumbar fascia(deep sheet), and the superior anterior iliac spine.
The muscle inserts at the white line and the pubic bone; its aponeurosis forms a part of the rectus sheath. A particularity of this muscle is that it joins the internal oblique muscle to form the cremaster muscle and attaches to the spermatic cord. The equivalent in women is the teres uteri ligament.
Innervation is provided by the intercostal nerves (Th7 – Th11), as well as the ilioinguinal nerve, the genitofemoral nerve, the iliohypogastric nerve and the subcostal nerve (Th12). At bilateral contraction, the abdominal organs are pushed inwards, which contributes to the abdominal press during expiration.
External oblique muscle
From the outer surface of the 5th – 12th rib, this outermost abdominal muscle runs in caudal and medial direction and perpendicular to the internal oblique muscle. The muscle shares its points of origin with the insertion spikes of the anterior serratus muscle. In athletic persons, a serrated line is clearly visible.
The insertion points can be divided into a medial crus and a lateral crus. The medial crus forms the rectus sheath and radiates into the white line. The lateral crus inserts at the iliac crest and the pubic tubercle. Between the two crura, there is a fissure which forms the outer ring of the inguinal canal.
The anterior rami of the spinal nerves Th5—Th12 innervate this muscle. It supports the abdominal press for expiration.
Internal oblique muscle
This skeletal muscle belonging to the abdominal muscles originates from the deep lamina of the thoracolumbar fascia, the lateral half of the inguinal ligament, and the superior anterior iliac spine. After its cranial-medial course, it inserts at the inferior edge of the rib cartilages 9—2.
Furthermore, the muscle participates in the formation of the rectus sheath. As mentioned above in the section on the external oblique muscle, their fiber bundles form together with the cremaster muscle.
The innervation of this muscle is supplied by the anterior rami of the spinal nerves Th8 – Th12, as well as the ilioinguinal nerve, the iliohypogastric nerve, and the genitofemoral nerve. Among other things, this muscle plays a role for the abdominal press and expiration.
Erector spinae muscle
This large back muscle group, lying on the vertebral column, belongs to the intrinsic back muscles. These intrinsic (or autochthonous) back muscles are divided into a medial and a lateral part, which shall not be described in more detail at this point.
It receives innervation from dorsal rami of the spinal nerves: The medial part is innervated by the medial rami, the lateral part by the lateral rami.
Quadratus lumborum muscle
This deep abdominal muscle originates from the iliac crest and the iliolumbar ligament, and inserts at the inferior edge of the 12th rib and the costal processes of the lumbar vertebrae 1 – 4.
The innervation is provided by anterior rami from Th12 – L3. In forced expiration, this muscle fixes the free ribs.
Review Questions
Answers can be found below the references.
1. Which abdominal muscle is not a muscle of the anterior abdominal wall?
- Quadratus lumborum muscle
- Rectus abdominis muscle
- Internal oblique muscle
- A, B, and C are correct.
- None of the above.
2. For which of the following processes does atmospheric pressure play a role?
- Lung ventilation
- Production of surface active surfactant
- Lung resistance
- A, B, and C are correct.
- None of the above.
3. What is the correct term for the pressure difference between intra-alveolar and intra-pulmonary pressure?
- Atmospheric pressure
- Negative pressure
- Transpulmonary pressure
- Positive pressure
- Lung pressure
4. What does the contraction of the external intercostal muscles do?
- Caudal movement of the diaphragm
- Cranial movement of the ribs and the sternum
- Compression of the thorax
- A, B, and C are correct.
- None of the above.
Patients frequently ask
What is a normal respiration rate?
The normal respiratory rate for a healthy adult at rest is 12-18 breaths per minute. Average resting respiratory rate by age are:

Comentários
Enviar um comentário