Anatomy and Functions of the Kidneys and Kidney Stones
Table of Contents
- Location of the Kidney
- Shape of the Kidney
- Positional Relations to other Organs
- The Kidney’s Relation to the Peritoneum
- Function of the Kidney
- Histology of the Kidneys
- The Nephron: Functional Unit of the Kidney
- The Interstitium
- Diseases of the Kidney
- Examination of the Kidney
- Review Questions
- References
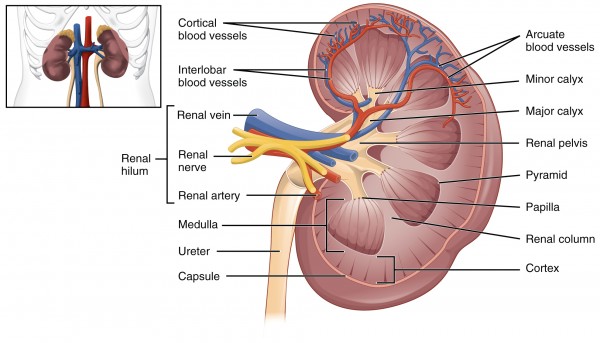
Image: “Internal Anatomy” by Phil Schatz. License: CC BY-SA 4.0
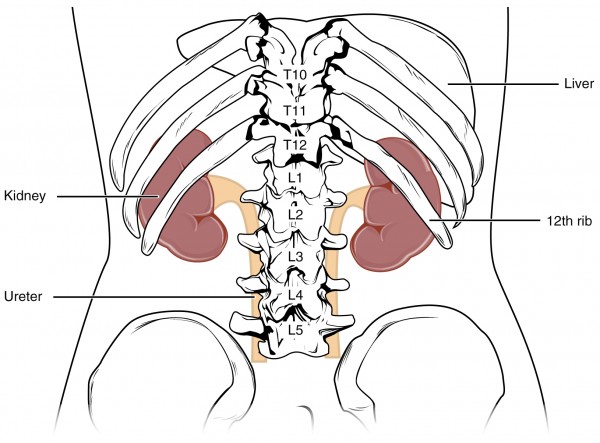
Location of the Kidney
The kidneys are located in the retroperitoneum beneath the diaphragm on each side of the spinal column. They are embedded in a groove, the renal fossa, which consists of the M. psoas major and the M. quadratus lumborum. The left kidney lies between the level of the 11th rib and the third lumbar vertebra.
Due to the size of the liver, the right kidney lies in a slightly lower position, beginning at the level of the 12th rib extending to the lower edge of the third lumbar vertebra. Physiologically, the kidneys have a moving flexibility of about 3-4 cm, depending on the posture of the body and the movement of the diaphragm during breathing, since the kidneys are not firmly adhered to the back abdominal wall.
Shape of the Kidney
As is well known, the kidney is bean-shaped and of a red-brown color. It has a thickness of 4 cm, a width of 5-7 cm and a length of about 11 cm (mnemonic: ‚four7-11‘). It weighs about 120-200 g.
The cranial and caudal edges are called poles, upper and lower (extremitas superior and extremitas inferior). The front surface of the kidney is called facies anterior, the back surface facies posterior. The kidney’s lateral edge (margo lateralis) has a convex shape. The margo medialis is concave. The renal hilum (hilum renale) with the kidney vessels is located on this medial edge. The renal vein lies ventrally to the renal artery, which is, in turn, anterior to the ureter (mnemonic: ‘VAU‘). The renal hilum is the access to the renal sinus and the renal pelvis.
Positional Relations to other Organs
- The adrenal glands are located cranially to the upper kidney poles.
- The subcostalis, N. iliohypogasticus and N. ilioinguinalis run dorsally.
The right hepatic lobe, pars descendes duodeni and the right colonic flexure run ventrally to the right kidney. In front of the left kidney are situated in the stomach, spleen, cauda pancreatis, the root of the transverse mesocolon and the left colonic flexure.
The Kidney’s Relation to the Peritoneum

Image: “
Normal kidney size and its influencing factors” by ncing factors” von G.B., U. V., T. B., H. KJ., R. P., S.A., P. J.. License: CC BY 2.0
The kidneys, adrenal glands and ureters are retroperitoneal organs. This means that they have developed behind the peritoneum and remained there.
The capsula fibrosa is a capsule of firm connective tissue surrounding the kidney. Another capsule of fat (capsula adiposa) encloses the kidney and the associated adrenal gland. Finally, there is the fascia renalis, another capsule of connective tissue.
Function of the Kidney
The entire blood volume of the body is flushed through the kidneys several times each day. This is how the kidneys can control and regulate, among other things, the blood pressure, the water- and electrolyte balance, the elimination of metabolic end-products and toxic substances, and the acid-base -balance.
The kidneys are important in maintaining the internal environment:
- Remove excess water, salt, and waste products
- Maintain the correct levels of nutrients and chemicals
- Maintain acid-base balance
- Maintain blood pressure
The water- and electrolyte-balance
The hormone renin is secreted by the kidney as soon as there is a drop in blood pressure or volume. Renin acts as a protease to split angiotensinogen from the liver into angiotensin I. Angiotensin I is then converted into angiotensin II through angiotensin-converting-enzyme (ACE) in the lungs. The result is, among others, vasoconstriction involving an increase in blood pressure. Moreover, aldosterone is secreted by the adrenal gland. This leads to an increased retention of water and sodium. This chain of reactions is called the renin-angiotensin-aldosterone -system (RAAS).
Atrial natriuretic peptide (ANP) is released if the heart’s right atrium has an increased blood volume. As a result, the kidneys excrete more water and sodium.
ADH (also known as vasopressin): If the blood is too concentrated, osmoreceptors in the hypothalamus will react. Here, ADH is produced and afterward stored in the posterior lobe of the pituitary gland. As a result of this secretion, the kidneys transfer more water from the primary urine back to the blood, thus thinning the blood and increasing its volume.
The kidneys also regulate the blood content of potassium, bicarbonate, phosphate, magnesium, and calcium through influences of hormones and specialized transporters.
Regulation of blood pressure
The kidneys regulate the blood pressure by changing the blood volume and the diameters of the blood vessels. Here, the renin-angiotensin-aldosterone-system plays an important part.
Regulation of the acid-base-balance
Changes in the pH level of the blood can have life-threatening consequences. The kidney has mechanisms for the excretion of protons and the reabsorption of bicarbonate.
The kidney’s hormones
Synthesis of glucose
Glucose is produced in the kidneys by gluconeogenesis and glycogenolysis. This mainly happens through the formation of glucose-6-phoshpate from substrates like lactate, glycerol and amino acids. Glucose is then released into the blood circulation. Therefore, the kidneys contribute to the regulation of the blood sugar in the body.
Histology of the Kidneys
The kidney produces about 1.5 liter final urine each day. The entire blood volume actually flows through the kidneys every 4—5 minutes. The kidney is a paired organ which is situated in the retroperitoneum and embedded in a firm capsule of connective tissue. Another protective capsule of fatty tissue is wrapped around this capsule. The kidney’s parenchyma is divided into the renal cortex (thickness approx. 1cm) and the renal medulla on the inside.
“Cortex” Image by Lecturio
The renal cortex forms the renal columns, the columnae renales. They extend into the medulla and divide it into 8-15 pyramids. The inner medulla leads to the calyces of the renal pelvis. Renal pelvis, calyces, the surrounding fatty tissue, vessels and nerves form the renal sinus (sinus renalis). The pelvis narrows and ultimately forms the ureter that drains the urine from the hilum.
Histologically, the kidney can be divided into the interstitium and the nephron.
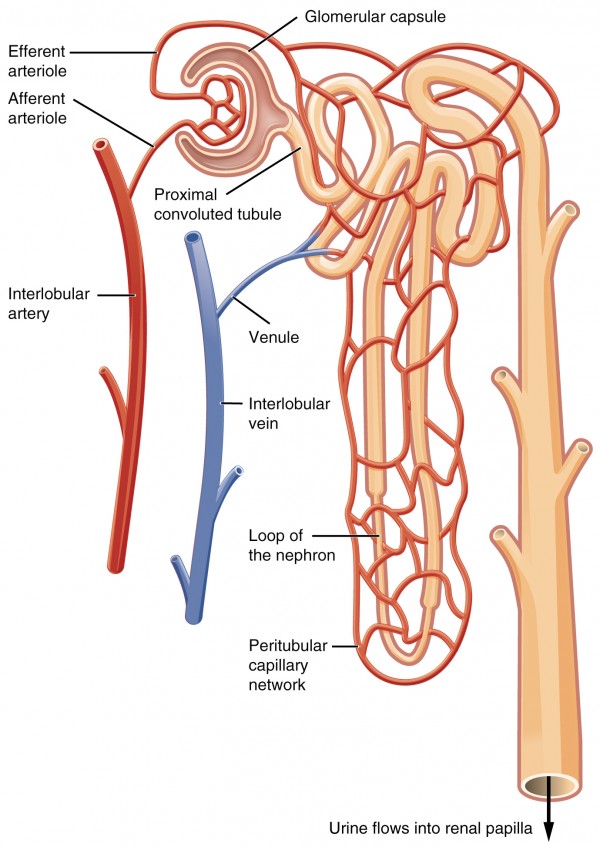
The Nephron: Functional Unit of the Kidney
The nephron is the functional unit of the kidney. It consists of the renal corpuscles as well as the tubules (tubuli renales) and forms an ingenious filter system. In each kidney, there are approximately 1—1.5 million renal corpuscles. A corpuscle is composed of the following components:
The glomerulus is a tuft of capillaries, woven together by anastomoses. They are supplied with fresh blood by the incoming vas afferens. The blood leaves the glomerulus by the vas efferens.
The Bowman’s capsule surrounds the glomerulus and consists of two layers. The parietal layer, formed by a single-layer epithelium lying on a basal lamina, is located on the outside. The visceral layer, formed by so-called podocytes, is located on the inside. These are specialized cells with many processes lining the capillaries of the glomerulus. Both layers are connected at the vessel pole.
The mesangium consists of mesangium cells connected with gap junctions. They occupy the space in between the capillaries in the nephron. They are responsible for the formation of Extracellular Matrix (ECM) and of components of the glomerular basement membrane. They also have a phagocytic function and can contract when necessary to stabilize capillary walls.
The blood-urine-barrier: filter in the nephron
This important filter consists of 3 layers. Each layer refines the structure of the filter.
- The capillary endothelium has small windows (100nm wide) and a strong anionicglycocalyx.
- The glomerular basement membrane (GBM) is located in the center and is formed by the capillaries’ and podocytes’ basal lamina.
- The podocytes form processes which interdigitate, thereby forming gaps (40nm). These pores are covered by a membrane consisting mostly of a protein essential for the functioning of the filtration barrier called nephrin. Podocytes also have a strong anionic glycocalyx facing the urinary side.
Molecules up to a size of 4 nm are filtered through these structures and sorted out based on their electrical charge. This way especially, proteins are prevented from entering into the urine. The ratio of the pressure of capillaries to the capsule chamber (55 mm Hg : 15 mm Hg) also plays a role in filtration.
In general, the renal corpuscles are only located in the renal cortex. Nephrons may, however, be called cortical, mediocortical, juxtamedullary, depending on the position of the renal corpuscle. The blood that has to be filtered passes through the renal corpuscle and then the blood-urine barrier selects the filtrate that enters the Bowman space. From here the ultrafiltrate begins its process of water reabsorption and solute modification.
Schematic structure of the renal corpuscle:
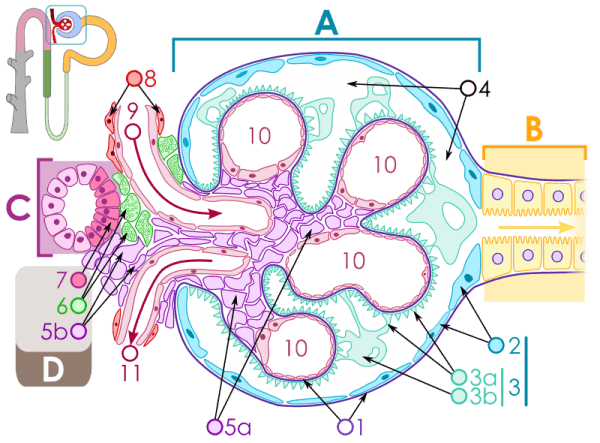
Image: “Schematischer Aufbau des Nierenkörperchens ” by Michał Komorniczak. License: CC BY-SA 3.0
A: Renal corpuscle; B: Proximal tubule; C: Distal convoluted tube; D: Juxtaglomerular apparatus 1: Basement membrane; 2: Bowman’s capsule, parietal layer; 3: Bowman’s capsule, visceral layer; 3a: Podocyte pedicles; 3b: Podocyte; 4: Bowman’s space (urinary space); 5a: Mesangium – intraglomerular cells; 5b: Mesangium – extraglomerular cells; 6: Juxtaglomerular cells; 7: Macula densa; 8: Myocytes (cells of smooth muscle); 9: Afferent arteriole; 10: Glomerulus capillaries; 11: Efferent arteriole
The renal tubules (tubuli) of the nephron
The proximal tubule begins with the convoluted pars contorta and changes into the distal straight pars recta. In this part, 80 % of the primary urine’s water, glucose, amino acids (Na+symport), electrolytes and urea are reabsorbed. This task is carried out by the cubic epithelium studded with a dense brush border.
The cells are connected and tightly sealed by tight junctions and zonulae adherens. The cells appear dark under the microscope. They are rich in mitochondria, vesicles for endocytosis, lysosomes, and peroxisomes. In this part of the renal tubules, calcidiol is converted to calcitriol under the influence of the hormone PTH.
The intermediary tubule, however, shows a flat epithelium which hardly features any vesicles or other of the aforementioned structures.
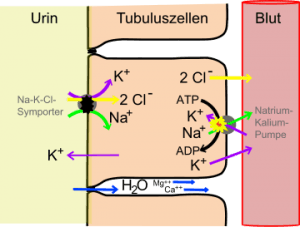
In the following distal tubule, especially NaCl is absorbed, but only a little water. It is a flatter cubic epithelium with many Na/K-ATPases and many tight junctions. The distal tubule is also divided into the pars recta with the intermediary macula densa (which is next to the extraglomerular mesangium) and the pars contorta.
The loop of Henle sits between the proximal and distal tubules and refers to the part of the renal tubule that comprises the intermediate tubule and the straight parts of the proximal and of the distal tubule.
The distal tubule merges into the junctional tubule and finally into the collecting tubule
The collecting tubule consists of:
- Principal cells: They are cubic, the cytoplasm appears pale. Water can be reabsorbed from the urine under the influence of the hormone ADH. It is transported from cell to cell by aquaporins. The hormone aldosterone also works here in order to absorb sodium.
- Intercalated cells – type A and B: These cells are used for the regulation of protons and potassium. Therefore, they have many H+-ATPases and H+/K+-ATPases. They are darker than the principal cells. Subsequently, several collecting tubules unite and form the ductus papillaris which then runs to the kidney pelvis.
The juxtaglomerular apparatus is a distinctive structure in the kidney and acts as a local controller for the NaCl-concentration and as a regulator for the blood pressure in the body. It consists of many different cells.
The iuxtaglomerular cells lie between the endothelium and the media of the vas afferens. They react upon activation of the sympathetic system (e.g. hypovolemia) and upon drops in pressure which leads to the secretion of renin (renin → angiotensinogen → angiotensin I → angiotensin II (by ACE) → leads to an increase in aldosterone secretion in the adrenal glands and vasoconstriction → higher blood pressure).
The palisade shaped cells of the macula densa belong to the cells of the distal tubule. They are located next to the vas afferens and continuously measure the concentration of intraluminal sodium. If detecting a rash of sodium, the vas afferens contracts.
The extraglomerular mesangium cells (Goormaghtigh cells) are located between the juxtaglomerula cells and the macula densa cells.
The Interstitium
It consists of connective tissue and free cells as well as nerves, vessels and the peritubular fibroblasts. These cells produce erythropoietin, the growth hormone for erythrocytes when the oxygen in the blood is low.
In the clinic:
- If the renal corpuscles and therefore the blood-urine-barrier are damaged, the result is a higher permeability for proteins. This leads to hypoproteinemia, generalized edemas and a higher vulnerability for infections.
- The kidneys may reabsorb glucose up to a certain threshold value (a blood glucose level of 200mg/dl). Especially in patients with diabetes mellitus, this limit is being exceeded which results in glucosuria.
- There is a threshold value for hemoglobin as well. An excess, e.g. during increased hemolysis, leads to hemoglobinuria.
Diseases of the Kidney
Get an overview of the most important pathologies of the kidney. Here, you find the most relevant study examples for the categories malformations, inflammations, cysts and kidney stones.
Malformations of the kidney: renal agenesis and horseshoes kidney
Renal agenesis refers to the congenital absence of one (unilateral) or both (bilateral) kidneys. The absence of one kidney may be compensated by the remaining kidney. Bilateral agenesis, however, is always fatal.
A horseshoe kidney is a frequently occurring abnormality of the kidney. The kidneys are fused together at their lower poles to form the shape of a horseshoe. This malformation usually is asymptomatic.
Renal inflammation
The acute pyelonephritis is a bacterial infection which is mostly caused by an ascending urinary tract infection. In 70 % of the cases, the trigger is Escherichia coli – an often asked fact in exams. Common symptoms include fever, dysuria (problems with urination) and pain on percussion in the flank.
Kidney cysts
The simple kidney cyst is the most common renal alteration. The Bosniak-classification distinguishes between simple and complex cysts, depending on whether they have septa or calcifications.
The cystic kidney, in turn, refers to a pathology that is either congenital or acquired. The classification of this pathology follows the system of Potter. The hereditary form is called polycystic, whereas cystic changes caused by dysplastic development are called multicystic.
Kidney stones or urolithiasis
Kidney stones develop when there is an over-saturation of one substance in the urine. Depending on the urinary pH, the substance settles and forms stones.
There are many reasons for high concentrations in urine. Too little fluid intake, a high fluid loss, a nutrition rich in sodium chloride and calcium, immobilization during a long period of time, hormonal changes, gout and many other things may be responsible for the formation of kidney stones.
Inorganic and organic stones are to be looked at separately:
Inorganic stones:
- Stones of calcium oxalate (65 %), calcium phosphate (10 %), or magnesium-ammonium-phosphate (10 % – also called struvite stones)
These stones are visible on radiographs without the application of a contrast medium.
Organic stones:
- Uric acid residues (10 % – increased in gout), cystine stones (1 %)
These stones cannot be seen without the application of a contrast medium.
Symptoms occur when the urine flow is obstructed or the stone gets stuck in a narrow part. Common symptoms include pain in the flanks spreading to the lower abdomen and back. They can even lead to colic, nausea and vomiting, sometimes to blood in the urine. As a result of kidney stones, complications may occur, leading to urinary obstruction and infection.
Small kidney stones often travel through the ureters and bladder by themselves. However, if the passage is not possible, the following measures can be taken:
- Extra-corporal shock wave lithotripsy: The kidney stone is placed at the intersection of two shock waves and decomposes into many fragments.
- Pyelotomy: A surgery in which the renal pelvis is opened.
- Flexible or semi-rigid ureteroscopy: The ureter is flushed, and the stone is crushed.
Renal cell carcinoma
The most common malignant renal cancer is the renal cell carcinoma formerly known as Grawitz tumor. It originates mainly in the epithelia of the proximal tubule. Under the microscope, cancer can be discerned as a clear cell tumor, which means the cytoplasm is full of glycogen and lipids.
Renal cell carcinoma can be detected early in an ultrasonic examination. Symptoms, e.g. pain in the flank or painless hematuria, occur late. The moment of detection is very crucial for the progression of the disease and prognosis. Men are affected twice as often as women.
Kidney transplantation
If there is a definitive kidney failure, a kidney transplant is the best treatment.
Organs to be transplanted may be obtained either from a living donor or from a deceased donor (post-mortem donation). There are some advantages to the living donation: There is little or no waiting time and a longer functioning of the donor organ and a higher life expectancy for the receiver can be expected.
Post-mortem donation means that the organ stems from a person that has been determined brain dead. The criteria for a possible donor include the matching of HLA-antigens. The waiting time for such a donor organ is usually several years and is bridged by dialysis (‘blood cleansing’).
Some complications may occur after a kidney transplant. In addition to the risk of wound infection, thrombosis, and other typical postoperative complications, there may be a rejection. In order to minimize the risk, the receiver will have to take immunosuppressants his entire life.
Examination of the Kidney
Review Questions
The answers are below the references.
1. Which hormone acts on the kidney and regulates the plasma osmolality?
- Renin
- ADH
- Erythropoietin
- Prolactin
- Aldosterone
2. What is the topographic relation of the kidneys to the peritoneum?
- Intraperitoneal
- Secondary retroperitoneal
- Primary retroperitoneal
- Subperitoneal
- Mesoperitoneal
3. What is the maximum size of molecules to cross the blood-urine barrier?
- 4nm
- 5nm
- 10nm
- 40nm
- 100nm


Comentários
Enviar um comentário