Acute Liver Failure (ALF) — Causes and Treatment
Table of Contents
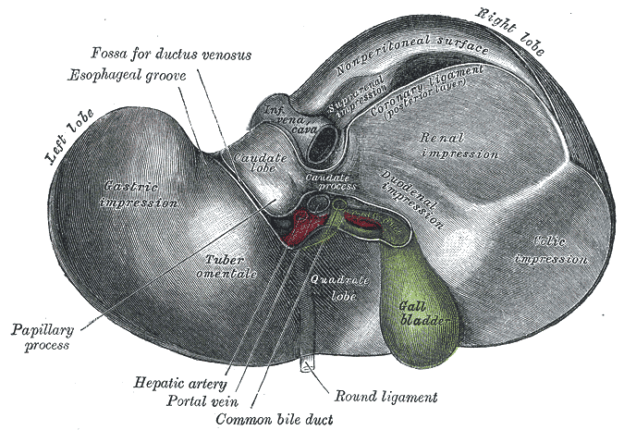
Image: “Inferior surface of the liver” by Henry Vandyke Carter – Henry Gray (1918) Anatomy of the Human Body, Bartleby.com: Gray’s Anatomy, Plate 1086, License: Public Domain
Etiology of Acute Liver Failure
As mentioned, the causes for the development of acute liver failure vary from one place to another. Another example of this fact is the prevalence of Hepatitis B virus infection-caused liver failure in France, Japan, and India. Aside from these, many other causes have been found out to cause the development of the disease.
Acetaminophen toxicity
Being an over-the-counter medication for mild pain and fever, many people tend to overuse acetaminophen. It is available in many different preparations such as tablets, syrups, suspensions, suppositories, and intravenous solutions.
The mechanism of damage by acetaminophen starts when excessive amounts of the drug overwhelm the physiological conjugation processes in the liver and ‘spill over’ to another means of drug metabolism by the liver. Instead of being harmlessly metabolized and bound to glucuronates and sulfates, excessive acetaminophen compounds enter CYP protein-mediated metabolic reactions in the liver. This results in the formation of N-acetyl-p-benzoquinoneimineor NAPQI.
In normal circumstances, a few acetaminophen metabolites enter the latter reaction and are converted to NAPQI. However, a reducing agent such as glutathione neutralizes these metabolites, rendering them inactive.
Excessive amounts of NAPQI such as in the indiscriminate use of acetaminophen or in attempted suicides, the internal stores for glutathione are exhausted, leading to the destruction of hepatocytes by NAPQI. This results in centrilobular necrosis and hepatocellular injury.
Idiosyncratic drug toxicity
Although it only makes up a small percentage of the total when it comes to causing fulminant liver disease, unusual drug reactions are implicated in the development of the pathogenesis. Various medications such as antibiotics, pain relievers, and anti-seizures have had unpredictable reactions resulting in a metabolic idiosyncrasy. Specific medications under this category include isoniazid propylthiouracil, phenytoin, and valproic acid. Most commonly affected individuals are females.
Aside from commercial pharmaceutical products, herbal preparations are also known to cause fulminant liver failure. These alternative medications include kava kava, green tea, black cohosh, weight loss supplements and ephedra. Their ability to contribute to the number of cases of liver failure is prominent, as the commercialization of these products is not strictly regulated in most areas.
The diagnosis of fulminant liver failure caused by idiosyncratic reactions caused by medications is somewhat challenging because one cannot pinpoint a certain laboratory marker to use as a basis for diagnosis. The primary management for unusual hepatic reactions with medications is the discontinuation of these medications.
Viral infections
The prevalence of hepatitis infections all over the world influences the proportion of cases of acute liver failure caused by viral infections. The most common viruses associated with fulminant liver failure are Hepatitis A and B viruses (HAV, HBV). It is more prevalent in populations residing in developing countries.
HAV infection, being highly preventable and curable, rarely results in acute liver failure. Even if it does result in failure, most of the time the outcome is good. The availability of vaccines worldwide against HAV also has contributed to the declining prevalence of acute liver failure from the infection.
HBV, on the other hand, is a more common cause of viral acute liver failure. However, like HAV, it rarely results in liver failure. It has been said in studies that certain components of the virus, such as the precore or core promoters are responsible for the predisposition to liver failure.
Other hepatitis-associated viruses that can cause acute liver failure include:
- HDV – requires an existing infection with HBV
- HEV – one of the most common viral causes of acute liver failure in India; pregnant women are especially predisposed
- HCV – rarely causes acute liver failure
Hepatitis B associated liver failure. Table adapted from Textbook of Clinical Gastroenterology and Hepatology, 2nd ed. by Hawkey CJ, Bosch J, Richter JE, Tsao GG and Chan FKL
Other non-hepatotropic viruses that can result in acute liver failure are the following:
- Epstein-Barr virus (EBV)
- Cytomegalovirus (CMV)
- Varicella-zoster virus
- Herpes simplex virus (HSV)
Miscellaneous causes
In some cases, the fulminant liver disease can result from pregnancy, particularly during the 3rdtrimester. This is thought to happen because of an inborn deficiency in an enzyme involved in fatty acid oxidation in the liver. Sometimes, liver failure during pregnancy can also be attributed to the accompanying preeclampsia.
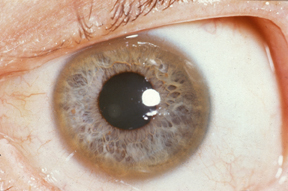
Image: “Kayser-Fleischer ring: copper deposition in Descemet’s membrane of the cornea. These rings can be either dark brown, golden, or reddish-green, are 1 to 3 mm wide, and appear at the corneal limbus. With rare exceptions, they are diagnostic of inherited hepatolenticular degeneration—Wilson’s disease.” by Herbert L. Fred, MD, Hendrik A. van Dijk – http://cnx.org/content/m15007/latest/, License: CC BY 3.0
Another disorder that could contribute to the development of fulminant liver failure is Wilson’s disease. This is an autosomal recessive disorder that manifests with excessive copper stores in the liver as a result of impaired biliary excretion of the element.
Patients who come to the clinics with this disorder are usually in their 20’s or 30’s, have prominent hemolysis, a low serum alkaline phosphatase level, an elevated serum aspartate aminotransferase to alanine aminotransferase ratio (AST-to-ALT ratio), the presence of excessive copper in the urine and Kayser-Fleischer rings.
Indeterminate acute liver failure
In some cases, acute liver failure is preceded by signs and symptoms of viral infections. However, during testing, patients may appear seronegative to HAV, HBV, and other hepatitis viruses. They may also be free from metabolites of idiosyncratically reacting medications. These cases are usually described as an indeterminate acute liver failure.
Clinical Features of Acute Liver Failure
Generally speaking, the manifestation of acute liver failure results from the cessation of function of the hepatocytes, such as in the production of amino acids, the metabolism of nutrients and medications, and the neutralization of radicals in the body.
Initially, patients with fulminant liver failure present with nonspecific signs and symptoms such as nausea, vomiting, fatigue, and jaundice. More liver-specific manifestations such as bilirubin excretion, clotting factor deficiency, and impaired glucose synthesis follow soon after.
Hepatic encephalopathy
It has been commonly thought of that hepatic encephalopathy is a result of the shunting of toxins and radicals to the blood stream and into the central nervous system. However, recent studies have suggested that hepatic encephalopathy is caused by cerebral edema and increased intracranial pressure. Other contributory factors that could lead to nervous systemdisturbances in fulminant liver failure include:
- Hypoglycemia
- Sepsis
- Fever
- Hypoxemia
- Hypotension
All of these factors could result from the impairment of the liver’s functions.
Staging for hepatic encephalopathy is the same as staging for liver cirrhosis.
Coagulopathy and bleeding
In fulminant liver failure, clotting and bleeding problems coexist as a result of the impairment of the clotting factor synthesis and degradation functions of the liver. Laboratory findings for patients with acute liver failure may show results that are indicative of the following:
- Fibrinolysis
- Hypofibrinogenemia
- Dysfibrinogenemia
- Disseminated intravascular coagulopathy
Infection
There are 3 mechanisms by which patients with fulminant liver failure are predisposed to infections:
- The damage in the hepatic macrophages or the Kupffer cells in the liver results in the entry of microorganisms from the portal venous system to the systemic circulation.
- There is a decrease in the production of acute-phase reactants in the liver. This could result in impaired neutrophil action.
- Patients with fulminant liver failure are subjected to breaks in the physical barriers such as in diagnostic testing and invasive therapeutic measures.
The presence of infection among fulminant liver failure patients accounts for a significant percentage of the rejection cases for liver transplantation and deaths after transplantation. Infections also tend to worsen the preexisting liver failure-related manifestations such as hepatic encephalopathy and coagulation problems.
Multiple organ failure syndrome
Multiple organ failure syndrome from fulminant liver failure can occur by means of 2 mechanisms:
- The polymerized actin from damaged hepatocytes and platelet activation irritate and damage the endothelia of blood vessels.
- Many vasoactive substances that are normally present in the bloodstream are retained in the circulation because of an impaired excretory mechanism in the liver.
This syndrome can manifest as peripheral dilation of blood vessels with hypotension, pulmonary edema, renal failure, and disseminated intravascular coagulopathy.
Diagnosis of Acute Liver Failure
Since the there are varying etiologies for different cases of fulminant liver failure, it is important to get clues from the patient’s history and physical examination. Histologic examination of the damages liver tissue can only contribute a small amount to the diagnosis. However, some histologic findings could help in ruling out certain causes for fulminant liver failure.
Diagnosis for the different causative agents for liver failure. Table adapted from Textbook of Clinical Gastroenterology and Hepatology, 2nd ed. by Hawkey CJ, Bosch J, Richter JE, Tsao GG and Chan FKL
Treatment of Acute Liver Failure
Initially, the management of a patient with fulminant liver failure involves the identification of the causative agent. This is because the management of the causes vary significantly. In most hospital protocols, fulminant liver failure is treated in an intensive care unit due to its unpredictable development.
Encephalopathy
This condition, when associated with liver failure tends to be very progressive. Medications such as sedatives are avoided unless intubation is required. Reversible conditions such as infections, hypoglycemia, and hypoxemia should be addressed immediately.
Airway management should be provided as needed. Intracranial pressure should be monitored and controlled accordingly in order to prevent further complications.
Coagulopathy and bleeding
Patients with fulminant liver failure should have a nasogastric tube inserted in order to monitor for gastrointestinal bleeding and gastric pH fluctuations. Medications such as H2 receptor antagonists and proton pump inhibitors are provided in order to decrease the risk of gastrointestinal bleeding. Vitamin K is also administered subcutaneously in order to address the deficiency in the vitamin K-dependent clotting factors. A blood coagulation panel should also be measured regularly to monitor the progress of the treatment.
Infection
Monitoring of the cultures from the blood, urine, and ascitic fluid should be done daily because the assessment for infections among liver failure patients is difficult due to the presence of relatively nonspecific manifestations (hypotension, leukocytosis, and acidosis). Antibiotics can help in the delay in the development of infections in patients. However, not all practitioners agree that this is helpful due to the fact that it could aggravate idiosyncratic reactions. The most commonly prescribed empirical regimen is a combination of intravenous vancomycin and a 3rd generation cephalosporin or fluoroquinolone.
Multiple organ failure syndrome
The primary goal for patients manifesting with this syndrome is to normalize the arterial pressure and to ensure proper tissue oxygenation. This can be done by regularly monitoring the blood pressure, adequate volume replacement and careful use of vasopressors.
Prognosis of Acute Liver Failure
Review Question
The correct answer can be found below the references.
A patient came into the ER and complained of fever, abdominal pain, and nausea and vomiting. You suspect him to have acute liver failure after getting his history. Upon doing the physical examination, you notice a band encircling the iris of both eyes. What diagnostic test should be done in order to narrow down the etiology?
- Serum acetaminophen levels
- Serum copper levels
- IgM anti-HAV
- Differential white blood cell count
Comentários
Enviar um comentário