Types and Procedures of General Anesthesia
Table of Contents
Image: “Syringes prepared with medications that are expected to be used during an operation under general anesthesia maintained by sevoflurane gas: Propofol, an hypnotic Ephedrine, in case of hypotension Fentanyl, for analgesia Atracurium, for neuromuscular block Glycopyrronium bromide (here under trade name Robinul), reducing secretions.” by Mikael Häggström – Own work. License: CC0
Definition of General Anesthesia
Anesthesia refers to the abolition of sensation. General anesthesia is a reversible state characterized by loss of reception and perception of stimuli. Important effects seen in general anesthesia are sedation, reduced anxiety, lack of awareness and amnesia, skeletal muscle relaxation, suppression of protective reflexes and analgesia. The most important factors among these are analgesia, amnesia, and skeletal muscle relaxation. They referred to as the triad of anesthesia and must be achieved during administration of any anesthetic agent.
General anesthesia is used for performing complex surgeries.
Types of General Anesthetics
Image: “Ketamine Injection” by Psychonaught – Own work. License: Public Domain
Inhalational anesthetics:
- Gas: nitrous oxide
- Liquids: ether, halothane, enflurane, isoflurane, desflurane, sevoflurane
Intravenous Anesthetics:
Inducing agents: thiopentone sodium, methohexital sodium, propofol, etomidate
Slower acting drugs:
- Benzodiazepines: diazepam, lorazepam, midazolam
- Dissociative anesthesia: ketamine
- Opioid Analgesia: fentanyl
Characteristics of Ideal General Anesthetics
Rapid onset of action due to a low blood/gas solubility. Should have a pleasant odor and non-irritant to the respiratory tract. Should provide adequate immobility, analgesia, and muscle relaxation. Minimal adverse effects on liver, heart, and other organs. Cheap and stable thus doesn’t react with parts of the anesthetic circuit.
Should achieve the triad of anesthesia i.e. induce unconsciousness, analgesia and preferably some degree of muscle relaxation. Should have high potency (low MAC).
It should be noted that an ideal anesthetic agent that can achieve all the desired effects in all populations does not exist and thus the best agent is chosen from the available choices by weighing the pros and cons of each agent.
Phases of General Anesthesia
Anesthesia is characterized by three phases:
Induction phase: This is from the time of administration of anesthetic to the development of effective anesthesia. Induction of anesthesia with intravenous agent (e.g. propofol) will produce unconsciousness in 30 seconds. For achieving depth of anesthesia, some drugs are added to the anesthetics either by inhalation or intravenous routes. For example, neuromuscular blockers like succinylcholine and rocuronium are administered to achieve sufficient muscle relaxation and facilitate tracheal intubation.
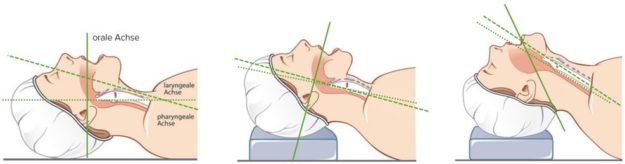
“Intubating the patient. A. The neck is too flexed B. The axis from brow to chest wall should be a straight line for ideal intubating conditions. C. The neck is too extended” Image created by Lecturio
Maintenance phase: It includes providing sustained anesthesia. After the administration of the anaesthetic agent, the vital signs and response to stimuli are continuously monitored to balance the amount of drug inhaled, or infused, with the depth of anesthesia. Sevoflurane (also used for induction), desflurane and nitrous oxide are commonly used agents used for the maintenance of anesthesia.
Recovery phase: This is the time from the discontinuation of anesthetic until consciousness and reflexes return. It is the reverse of the induction phase. The patient is monitored until there is a return of normal physiologic functions.
Summary
- Pre-operative assessment of the patient
- Evaluation of the airway
- Induction of general anesthesia
- Securing the airway
- Maintenance of general anesthesia
- Reversal of muscle relaxation (if necessary)
- Recovery from general anesthesia
- Management of pain
- Recovery room care
Depth of Anesthesia
The process of achievement of effective anesthesia is dependent on the depth of anesthesia. It includes four stages:
Stage 1: Analgesia
In this stage, awareness of pain is decreased because of interference of sensory transmission with spinothalamic tract. The condition progresses from conscious to conversational to drowsy.Consciousness is impaired, but not lost.
Stage 2: Disinhibition
The patient is in a state of delirium and excitation. The patient may shout or struggle in this stage. Vomiting, involuntary defecation or micturition may also occur. The operation should not be conducted during this stage.
Stage 3: Surgical anesthesia
Bild: “Diagram of an Inserted Endotracheal Tube” by PhilippN. License: Public Domain
It is characterized by the following activities:
- Roving eyeballs movements
- Loss of corneal and laryngeal reflexes
- Pupil dilation
- Intercostal paralysis
- Patient is unconscious in this stage.
Stage 4: Medullary depression
Severe respiratory and cardiovascular depression results in this stage. It requires mechanical and pharmacological support to prevent the death of a patient.
Mechanism of Action of General Anesthetics
General anesthetics act either by inhibiting the excitatory receptors (NMDA) or facilitating the actions of inhibitory receptors (GABA). Mechanism of action of general anesthetics is best explained by Meyer-Overton lipid solubility theory. This theory put forth the following hypothesis:
The greater the lipid solubility of an anesthetic agent, the higher will be its potency. This theory is quite old, but it still has significance and relevance in modern medicine to explain the correlation of lipophilicity of anesthetics and their potency.
Also, anesthetic agents don’t specifically act at one single ion channel, but they may act on two or more types of ion channels.
Barbiturates, benzodiazepines, etomidate and propofol and all inhaled anesthetics act by facilitating the actions of inhibitory receptors, GABA. Potentiation of GABA receptors leads to opening of the chloride ion channels which later hyperpolarize or short circuit the synaptic membrane.
Ketamine and nitrous oxide act by inhibiting the N-methyl-Daspartate (NMDA) receptor. Ketamine is a non-competitive antagonist of the NMDA receptor Ca2+ channel pore and inhibits NMDA receptor activity by interaction with phencyclidine.
Inhalational Anesthetics
Inhalational anesthetics are commonly used as an induction and maintenance agent. The speed of induction of anesthetic effects depends on factors like:
- Solubility: the greater the solubility, the greater will be the induction of an anesthetic.
- Inspired gas partial pressure: a higher partial pressure of the gas in the lungs results in the greater speed of induction of an anesthetic.
- Ventilation rate: the greater the ventilation rate, the faster is the effect of an anesthetic agent.
- Pulmonary blood flow: a high pulmonary blood flow results in the slow onset of the effect of an anesthetic.
- Arteriovenous concentration gradient: the greater the arteriovenous concentration gradient, the slower will be the induction.
Elimination of Inhalational Anesthetics
All the inhalational anesthetics are excreted from the lungs. Due to the high lipid solubility of general anesthetics, they persist in the adipose tissue for longer periods. Halothane and methoxyflurane are metabolized by liver enzymes. Due to the high amount of hepatic metabolism of halothane, it shows the highest cases of hepatic injuries among all the inhalational anesthetics.
Minimum Alveolar Concentration (MAC)
The potency of inhaled anesthetics is measured by the minimum alveolar anesthetic concentration (MAC), (in volume percent) is defined as the least amount of alveolar concentration of an anesthetic agent at 1 atmosphere required to prevent the response to a standardized painful stimulus in 50% of subjects.
Always remember: MAC is a measure of potency only applicable for inhalational anesthetics.
The MAC value of inhaled anesthetics is somewhat related to its lipid solubility. The higher the lipid solubility, the higher will be its potency and the lower will be the MAC value. The MAC value for halothane is 0.75% (high potency), isoflurane 1.15%, sevoflurane 1.71-2.05%and the MAC value of nitrous oxide is 104% (low potency).
Effects of Inhaled Anesthetics on Organ Systems
CNS Effects
Anesthetics decrease the global cerebral metabolic rate. This is thought to be the mechanism behind the unconsciousness produced by general anesthetics. They act by reducing the vascular resistance in the brain, in turn, causing an increase in cerebral blood flow leading to an increase in intracranial pressure in a dose dependent manner.
Enflurane, given in high doses, may cause spike-and-wave activity and muscle twitching. Because of low blood gas partition coefficient, nitrous oxide has a low anesthetic potency. (High MAC) nitrous oxide exerts analgesic and amnestic actions.
Cardiovascular Effects
A moderate decrease in arterial blood pressure is seen when the drug is given by inhalation route. Halothane and enflurane decrease cardiac output; isoflurane, desflurane and sevoflurane cause peripheral vasodilatation.
Inhaled anesthetics depress myocardial function – nitrous oxide exerts the least effects on the myocardium. Halothane also causes depression of myocardial contractibility and can cause arrhythmia.
Isoflurane causes coronary vasodilation which in the presence of fixed coronary stenotic lesions can cause redistribution of coronary blood supply from the endocardium to the epicardium a state known as coronary steel effect.
Respiratory Effects
Most of the inhaled anesthetics produce bronchodilation except desflurane, which produces bronchospasm. They also increase respiratory rate, decrease tidal volume, and minute ventilation i.e. they are respiratory depressants.
Isoflurane and desflurane induce respiratory tract irritation thus may cause coughing, breath holding and increased bronchial secretions.
Halothane
Due to hepatotoxicity, its use is nearly eliminated in North America. It also causes myocardial depression. Halothane is metabolized to 20-30% in the liver, as compared to newer inhalational anesthetics, enflurane (2%), sevoflurane (1%), isoflurane and desflurane (less than 0.2%).
Isoflurane
It is the most potent anesthetic among the inhalational anesthetics. It has rapid (7-10 min) and short duration of action.
Desflurane
It is not used as an induction anesthetic as it causes air way irritation (cough, laryngospasm and salivation). It also causes bronchospasm.
Sevoflurane
It is one of the most frequently and commonly used inhalational anesthetics for the induction of anesthesia. It produces a rapid onset of action (within a minute). Also, it is a preferred anesthetic as it has very less reported cases of hepatotoxicity.
Other advantages of sevoflurane are a lack of pungency, odor, and bronchospasm.
Overview
Nitrous Oxide
Common adverse effects of nitrous oxide include:
- It produces postoperative vomiting and nausea.
- Also, it is important to note that nitrous oxide causes inactivation of vitamin B12– it can cause neurodegeneration in vitamin B12 deficient patients that may lead to peripheral neuropathy in protracted use.
- It produces poor muscle relaxation, but a rapid induction of anesthesia. It is less potent (high MAC: 104%).
- Fink effect/diffusion hypoxia.
It produces poor muscle relaxation, but a rapid induction of anesthesia. It is less potent (high MAC: 104%).
Toxicity of Inhaled Anesthetics
1. Hepatotoxicity
In patients with hypovolemic shock, halothane causes postoperative hepatitis. Megaloblasticanemia may occur because of the decrease in methionine synthesis with increased exposure to nitrous oxide.
2. Malignant hyperthermia
Mutation in gene loci corresponding to ryanodine receptor (RyR1) results in an uncontrolled release of calcium by sarcoplasmic reticulum of skeletal muscle, leading to muscle spasm, hyperthermia and autonomic lability because of the simultaneous use of neuromuscular blockers (especially succinylcholine) and anesthetics. This condition is called malignant hyperthermia, which is life threatening. Dantrolene, along with supportive management, is used in the treatment of this condition.
3. Teratogenicity
Warning in pregnancy: Transient use of nitrous oxide may cause aplastic anemia in the fetus. Oral clefts have occurred in fetuses when mothers received benzodiazepines in early pregnancy. Benzodiazepines should not be used during labor because of resultant temporary hypotonia and altered thermoregulation in the newborn.
Intravenous Anesthetics
Barbiturates
Thiopental is an ultrashort-acting barbiturate with high lipid solubility. It acts by blocking GABAa receptors. The high lipid solubility of thiopental and methohexital helps in fast entry into the brain and results in surgical anesthesia in circulation time (<1 min).
These drugs are used for the induction of anesthesia and for short surgical procedures. Termination of anesthetic effects of thiopental is by redistribution from brain to highly perfused tissues and elimination is by hepatic metabolism.
Barbiturates depress cerebral blood flow and cause a decrease in intracranial pressure, and also act as respiratory and circulatory depressants.
Common adverse effects include :
- Anaphylactic reactions with use of the drug.
- Tissue necrosis with extravasation.
- Induction of arterial constriction and thrombi formation.
Benzodiazepines
These anesthetics are never used alone, but always used in adjunct with other anesthetics. Midazolam is used adjunctively with inhaled anesthetics and intravenous opioids.Thus, it is commonly used for procedures such as endoscopy of in the intensive care units. It is preferred over diazepam since it has a rapid and short duration of action with a safer side effect profile. it causes severe postoperative respiratory depression.
The clinical effects of benzodiazepines can be reversed with flumazenil.
Ketamine
Ketamine produces dissociative anesthesia characterized by analgesia, amnesia, and feeling of dissociation from the body.The patient has deliriums, unpleasant dreams, and hallucinations. It acts by blocking NMDA receptors. It is a cardiac stimulant (increase BP, heart rate, cardiac output) and increases intracranial pressure.
Ketamine is contraindicated in glaucoma or acute globe injury.It is metabolized primarily through the liver and excreted mostly in urine. It is a suitable anesthetic for small operations (consciousness is not lost). However, it is associated with pain on injection thus may necessitate co-administration with a local aesthetic agent.
Opioids
Morphine and fentanyl are used with other CNS depressants (nitrous oxide, benzodiazepines) and can be used in patients who cannot tolerate full general anesthesia.
Opioids, when given intravenously, will cause chest wall rigidity, impairing ventilation and causing respiratory depression, which is reversed postoperatively with naloxone. The route of administration can be intravenously, epidurally, or intrathecally (into the cerebrospinal fluid).
It has a short duration of action (30-50 min).
Neuroleptanesthesia is a state of analgesia and amnesia, produced when fentanyl is used with droperidol and nitrous oxide.
Newer opioids like alfentanil and remifentanil have been used for the induction of anesthesia.
Propofol
Propofol produces anesthesia (in 15-45 seconds) as rapidly as the intravenous barbiturates, and recover more rapidly. It has agonistic actions on GABAa receptors. It has antiemetic actions, and recovery is not delayed after prolonged infusion.
This is the anesthetic of choice in outpatient surgery and for producing prolonged sedation for patients admitted in critical care settings. Propofol decreases peripheral resistance and thus causes hypotension (in 15.7% patients) during induction.
Etomidate
This drug causes fast induction with very little change in cardiac function or respiratory rate and has a short duration of action of anesthesia and lacks analgesic properties. The primary advantage is in anesthesia for patients with limited cardiac or respiratory reserve.
Etomidate on injection causes pain and myoclonus. It also causes nausea postoperatively. Adrenal suppression (inhibits cortisol) is seen on administration for a long period.
Review Questions
The correct answers can be found below the references.
1. Which of the following inhalational anesthetics shows the highest rate of hepatitis?
- Halothane
- Isoflurane
- Desflurane
- Sevoflurane
- Nitrous oxide
2. Which of the following inhalational anesthetics causes bronchospasm?
- Halothane
- Isoflurane
- Desflurane
- Sevoflurane
- Nitrous oxide
What is the mechanism of action of ketamine?
- Blockage of NMDA receptors
- Blockage of GABAa receptors
- Blockage of GABAb receptors
- Blockage of opioids receptors
- Blockage of calcium channels




Comentários
Enviar um comentário