The Acute Scrotum in Adolescents: Testicular Torsion, Epididymitis, Hydroceles and More
In Lecturio . The acute scrotum is an emergency condition that is characterized by scrotal pain, swelling, and redness which are of acute onset. The most important diagnosis to exclude is testicular torsion, as the testicular tissues cannot withstand ischemia for more than few hours.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your adolescent medicine course now for free!
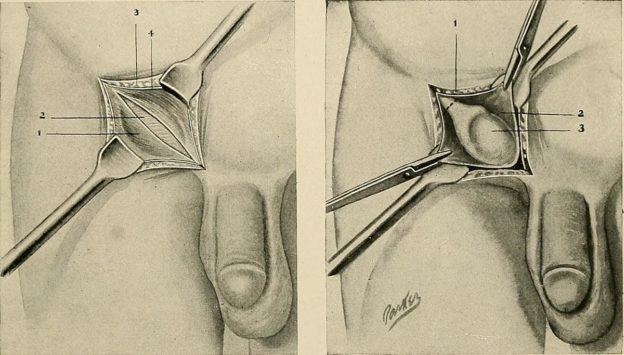
Image: “Surgery of undescended testicle.” by Internet Archive Book Images – https://www.flickr.com/photos/internetarchivebookimages/14592707188/ Source book page: https://archive.org/stream/practiceofsurger00mumf/practiceofsurger00mumf#page/n468/mode/1up. License: Flickr Commons
Epidemiology of the Acute Scrotum in Adolescents
The acute scrotum per our previous definition can be quite common in adolescents. According to our definition, the term acute scrotum includes testicular torsion, orchitis, and epididymitis, or non-testicular diseases that can also present with acute painful swelling of the scrotum. The peak incidence of the acute scrotum is seen in boys aged between 12 and 18 years.
“Scrotal Masses. General Characteristics” Image created by Lecturio
Testicular Torsion
Definition of Testicular Torsion
Testicular torsion is the sudden rotation of one of the testes around its axis. Strictly speaking, it refers to the twisting of the spermatic cord structures either in the inguinal canal or below.This acute rotation results in compromised blood flow to and from the testis. Because of the blocked venous return and the reduced arterial perfusion of the testis, hemorrhagic infarction of the testicular parenchyma occurs. For these pathologic changes to happen, the involved testis needs to rotate at least 360 degrees around its axis.
Delayed treatment of testicular torsion has been linked to impaired spermatogenesis. The main cause of testicular torsion is the abnormal degree of mobility of the testis. When the testis is hypermobile, physical exercise, trauma or the activation of the cremasteric reflex can result in testicular torsion.
Classification
Extravaginal torsion: This type manifests in the neonatal period and most commonly develops prenatally in the spermatic cord, proximal to the attachments of the tunica vaginalis.Intravaginal torsion: This type occurs within the tunica vaginalis, usually in older children.
Etiology and risk factors
- Certain anatomical variations such as the failure to anchor the gubernaculum, testis, and epididymis “the bell-clapper anomaly” may predispose to testicular torsion. Intravaginal torsion is the most common form of testicular torsion in adolescents.
- A large mesentery between the epididymis and the testis
- History of trauma is seen in 20% of patients with testicular torsion.
- 1/3 have had prior episodic testicular pain which may denote previous torsion that rotated and resolved hence acts as a risk factor for recurrence.
- Contraction of cremasteric muscle or dartos muscles shortens the spermatic cord and may initiate testicular torsion may play a role and is stimulated by trauma, exercise, cold, sexual stimulate.
- Cryptochirdism
- Testicular atrophy-post infectious or traumatic.
Clinical Presentation of Testicular Torsion
In the newborn it presents as a hard-scrotal mass that doesn’t transilluminate.In older patients, they usually complain of acute and severe pain that can be associated with nausea and vomiting. Younger adolescents can present with shock-like symptoms. The involved testis is fixed in position, near the body and can be vertical or oblique. The cremasteric reflex is lost in patients with testicular torsion.
Similar symptoms of epididymitis maybe experienced by the patient, however the testis discoloration and swelling that is dominant in epididymitis may not be present. Additionally, testicular infraction can cause a low-grade fever.
Prehn’s sign may be helpful in differentiating between torsion and epididymitis: If pain is reduced when the scrotum is lifted over the symphysis pubica, the pain is due to epididymitis; if pain increases, the cause is probably torsion.
Diagnostic Workup for Testicular Torsion
The main diagnostic tool for the evaluation of a suspected case of testicular torsion is history and physical examination. If the diagnosis is not straightforward, then ultrasonography and Doppler ultrasonography are indicated.The ultrasonographic findings of testicular torsion of ultrasonography depend on the degree of testicular ischemia. In the initial stage, ultrasonography reveals a progressive increase in testicular volume and diffuse hypoechogenicity. Inhomogeneities are found in delayed cases where irreversible testicular damage has happened.
Doppler ultrasonography is used to assess blood flow to and from the testis. The unambiguous demonstration of central arterial and venous flow from the testis is enough to exclude testicular torsion. In case of complete testicular torsion, central perfusion is absent.
Treatment of Testicular Torsion
Emergency surgical exploration of the tests is indicated in all cases of suspected or confirmed testicular torsion. The first step in the surgery is the detorsion of the testicular vessels to restore testicular perfusion. After that, the testicular parenchyma should be inspected to assess the degree of testicular damage. If the testis is clearly necrotic, primary orchiectomy is indicated. When the testis is not necrotic, it should be anchored to the scrotum with two sutures to prevent future recurrences of torsion. Contralateral orchiopexy is indicated in all cases of testicular torsion.When the testis is not removed, follow-up ultrasonography is indicated to assess for subsequent testicular damage and adequate perfusion.
Complications of testicular torsion
- Delayed surgery reduces the salvage rate by more than 50%
- Retention of an injured testis can induce pathologic changes to the contralateral testis.
- Recurrence if orchidopexy not done
- Infertility
Epididymitis and Orchitis
Definition of Epididymitis and Orchitis
Epididymitis and orchitis are two conditions that are characterized by the acute inflammation of the epididymis or the testis due to viral or bacterial infections. Viral orchitis is more common in prepubertal boys and young adolescents, whereas bacterial infections are more commonly seen in older adolescents.Clinical Presentation of Epididymitis and Orchitis
The main goal of the history taking and physical examination of the patient with any of these two conditions is to exclude the true surgical emergency “testicular torsion”. The main differences between these two conditions and testicular torsion are the slower onset, the absence of testicular fixation, and the normal position of the testis. Additionally, the cremasteric reflex is usually preserved. Patients might also complain of dysuria, urinary frequency, and urgency.
“Epididymitis” Image created by Lecturio
Causes of Epididymitis and Orchitis
Among sexual active teenagers gonorrhea as well as chlamydia are the major cause of the Epididymitis and Orchitis conditions. In older males the enteric bacteria are the common cause. The chlamydia trachomatis is responsible for almost two third of cases of urinary tract infections among sexually active men.The various forms of epididymitis can be because ofGenito urinary surgery, which includes prostatectomy as well as the urinary catheterization. Chemical epididymitis is as a result of using drugs such as amiodarone
Diagnostic Workup for Epididymitis and Orchitis

Picture: “An illustration of an adult human testicle with the epididymis highlighted” by KDS444. Lizenz: CC BY-SA 3.0
A urinalysis is indicated in all cases of suspected epididymitis or orchitis. Urinalysis can help with establishing the diagnosis of urinary tract infection and can point towards the most likely causative organism.
Treatment of Epididymitis and Orchitis
Because most cases of orchitis are viral in etiology, symptomatic treatment is all that is needed. Bed rest, local cooling, and nonsteroidal anti-inflammatory drugs are the main treatments prescribed for orchitis. Antibiotic treatment of orchitis and epididymitis is indicated when the cause is suspected to be bacterial in origin. Cefuroxime 100 mg/kg/day is a reasonable antibiotic choice for epididymitis in adolescents.Classification of epididymitis
Epididymitis can be grouped depending of the duration of the symptoms. It can be classified as acute, subacute as well as chronic. The chronic epididymitis is usual present for a duration of more than three months, and it is commonly associated with lower back pains.Testicular Trauma
Testicular trauma can also cause an acute scrotum. Hematocele or deme of the testis and scrotum are the main two findings seen after a blunt traumatic injury to the scrotum. Because testicular trauma can lead to testicular torsion, an ultrasonography should be performed to exclude this surgical emergency. If the testicular damage on ultrasonography is deemed as too extensive, surgical intervention is indicated. Otherwise, symptomatic treatment and ultrasonographic follow-up are all that is needed.Hydroceles
Definition of Hydroceles
Hydroceles in adolescents are usually idiopathic and are not related to a patent processus vaginalis. The main pathology behind idiopathic hydroceles is the imbalance between the secretion and absorption of fluid in the tunica vaginalis. Because of either excessive fluid secretion or decreased absorption, scrotal swelling ensues.Hydroceles are associated with some ipsilateral testicular changes which might be associated with decreased fertility in the future. Increased scrotal temperature and the absence of testicular diastolic flow are the main two abnormalities observed in the ipsilateral testis in an adolescent with a hydrocele.
Thanks for sharing such wonderful knowledge! Natural Treatment for Epididymitis as it has powerful antimicrobial Natural Essential oils that can successfully kill the offending bacteria.bacteria on the skin.
ResponderEliminarhttps://www.herbs-solutions-by-nature.com/Epididymitis.php