Types of Diabetes: Type 1, Type 2 and Type 3 and Gestational Diabetes
In many diseases, early diagnosis is important for slowing the progression. This also applies to diabetes mellitus. Especially with type 2 diabetes, a timely detection of symptoms may limit the severe consequential damage and help patients to further have an asymptomatic life. Therefore, medical students should have keen senses about the patients with obesity, weight loss, polydipsia and polyuria.
Table of Contents
Are you more of a visual learner? Check out our online video lectures and start your endocrine pathology course now for free!
Diabetes Mellitus
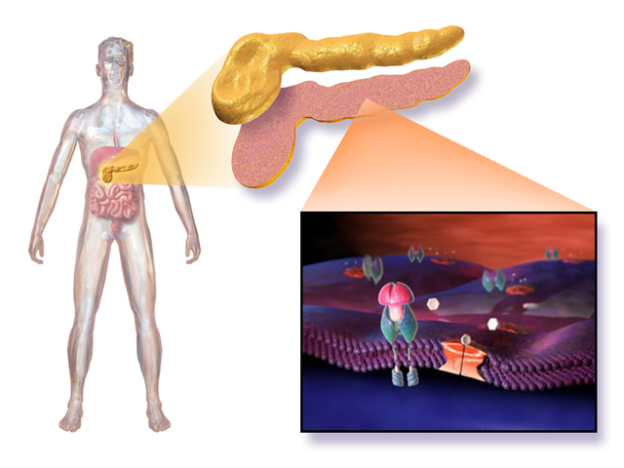
Diabetes Mellitus is a chronic systemic disease of carbohydrate, fat, and protein metabolism resulting from deficient secretion of insulin or peripheral tissue resistance to insulin.Diabetes Subtypes
| Type | Pathogenesis | Acute complications | Chronic complications |
| 1 (IDDM) | b-cell destruction; immune-mediated or idiopathic; affects non-obese younger patients (< 30 years old); genetic component (20—50 % twin concordance) with HLA link | Microvascular Macrovascular | |
| 2 (NIDDM) | Insulin resistance with relative insulin deficiency initially, can progress to type I-like picture; genetic component (60—90 % twin concordance); correlation with obesity genetic component (60—90 % twin concordance); Correlation with obesity |
| Microvascular Macrovascular |
Symptoms of Diabetes Mellitus Type 1
Type-1 diabetes, formerly known as juvenile diabetes, is common in children and young adults. In rare cases, type-1 diabetes occurs in adulthood, and then it carries the name LADA diabetes (latent autoimmune diabetes in the adult).The pathophysiology of type-1 DM is an autoimmune reaction. It leads to the destruction of insulin-producing beta cells of the islets of Langerhans in the pancreas. Only after 80—90 % of the beta cells are destroyed, the first symptoms of type 1 diabetes can be identified. Stressful situations can accelerate the onset of the disease, leading to an acute condition.
As diabetes is only symptomatic when 80—90% of beta cells are destroyed, the onset of the disease is often sudden and dramatic. Noticeable symptoms are weight loss, polydipsia and polyuria. Due to the absence of insulin hormone, the serum glucose level is greatly increased as glucose needs insulin to enter into the cells. Normally, the kidneys completely reabsorb the filtered glucose, and it is not excreted in the urine. But as serum glucose concentration rises over 180 mg/dL (10 mmoL/L), the renal threshold is exceeded, and glucose passes into the urine via the kidney.
Glucose, being a solvent, when excreted by the kidneys, takes free water with itself. Therefore, these patients suffer from frequent urination (polyuria) and excessive thirst. In young children, this may lead to enuresis, which must be understood as a warning sign for diabetes. Since glucose cannot enter into the cells and be processed as an energy supplier, the body relies on the energy reserves of the fatty tissues, which leads to significant weight loss.
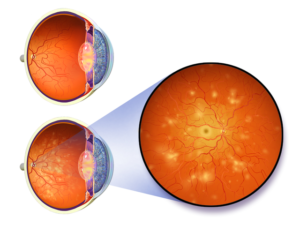
In addition, there may appear unspecific symptoms of the disease, such as malaise, fatigue, anorexia, amenorrhea, impotence problems and dehydration (exsiccosis). The consequential harm caused by diabetes becomes apparent in the subsequent course of the disease. Dry skin, pruritus, muscle cramps, delayed wound healing and visual disturbances are the first indications of the progress of diabetes.
In emergency cases, type-1 diabetics may present with life-threatening metabolic acidosis, known as diabetic ketoacidosis. Due to insulin deficiency, the serum glucose cannot be utilized, and the fatty acids are transformed into ketone bodies. These can enter the cells independently of insulin and are utilized for energy purposes. However, ketone bodies are acidic in nature, and their excessive accumulation causes the blood pH to decrease, leading to metabolic acidosis.
Patients with diabetic ketoacidosis initially present with nausea, vomiting, dehydration and abdominal pain. Metabolic acidosis may lead to disturbed breathing pattern (Kussmaul breathing), where the patient takes rapid, shallow breaths in order to hyperventilate, decreasing the carbon-dioxide levels as a compensatory mechanism. Further, the ketone bodies are composed of acetoacetate, beta-hydroxybutyrate and their spontaneous breakdown product, acetone. For this reason, patients presenting with diabetic ketoacidosis may have an acetone-like smell in their breath and urine.
Symptoms of Diabetes Mellitus Type 2
Type-2 diabetes mellitus is most common in adults over 40 years of age. However, due to increased prevalence of obesity in children and adolescents, the younger population is also increasingly diagnosed with type-2 diabetes mellitus. The etiology of type-2 diabetes is multifactorial and has a strong hereditary component. These patients often have the metabolic syndrome that includes central obesity, elevated triglyceride levels, insulin resistance and hypertension.The pathophysiology of type-2 diabetes mellitus is the combination of peripheral insulin resistance, and inadequate insulin secretion by beta cells of the pancreas.
While the presentation of type-1 diabetes mellitus is sudden in onset, the progression of the disease is insidious in type-2 diabetes mellitus. It is often discovered incidentally when investigations are performed for other purposes. Therefore, these patients have undetected type-2 diabetes mellitus for years and may have developed various microvascular and macrovascular complications. These include visual disturbances, polyneuropathy, chronic renal disease and impaired wound healing. For this reason, sometimes patients are first diagnosed with type-2 diabetes when they present with these late complications.
If symptoms are present, they are nonspecific, similar to those of type-1 diabetes. These include polyuria, polydipsia and polyphagia. Glucosuria may occur when the renal threshold is exceeded due to high serum glucose levels. However, these symptoms are more frequent in type-1 diabetes. Other nonspecific symptoms include:
- Fatigue, exhaustion
- Concentration problems
- Headache, dizziness
- Increased susceptibility to infection (cold, flu)
- Impaired wound healing
- Blurred vision
- Muscle cramps
- Pruritus
- Amenorrhea, impotence problems
- Frequent infections due to increased sugar content, in particular, in urine (fungi, cystitis, etc.)
- Acanthosis nigricans

Image: “Acanthosis nigricans,” by Madhero88. License: CC BY-SA 3.0
Note: Acanthosis nigricans of the inguinal and axillary region is typical for conditions with insulin resistance, especially in young patients.
Metabolic Syndrome
| Elevated waist circumference | Men: ≥ 40 inches (102 cm) |
| Women: ≥ 35 inches (88 cm) | |
| Elevated triglycerides | ≥ 150 mg/dL |
| Reduced HDL (“good”) cholesterol | Men: < 40 mg/dL |
| Women: < 50 mg/dL | |
| Elevated blood pressure | ≥ 130/85 mm Hg or use of medication for hypertension |
| Elevated fasting glucose | ≥ 100 mg/dL or use of medication for hyperglycemia |
Note: Patients with these findings are generally considered “high-risk” for adverse cardiac events.
Type 1 Versus Type 2 Diabetes
| Type 1 | Type 2 | |
| Weight | Normal or thin. Often lose weight prior to diagnosis | Overweight or obese |
| Age | Typically 1st—2nd decade of life but many presents at any age (latent autoimmune diabetes of adulthood, LADA) | Typically > age 40 but can present much earlier |
| Glycemic patterns | Highly variable | Less variable |
| Insulin sensitivity | Normal | Reduced |
| Response to oral agents | Not responsive | Responsive |
| Antibody status | Usually positive | Negative |
| C-peptide level | Low or undetectable | Detectable or high |
| Family history | 1st-degree relatives uncommonly affected | Strong family history of 1st-degree relatives |
| Other autoimmune disorders | May have autoimmune thyroid disease, adrenal insufficiency, vitiligo, pernicious anemia | Absent |
Symptoms of Gestational Diabetes
Gestational diabetes is often asymptomatic. Therefore, an oral glucose tolerance test (OGTT) is recommended during the 24th to 28th week of pregnancy. Untreated gestational diabetes can lead to developmental problems in the fetus. These result in an increased birth weight (over 4 kg requiring a cesarean section), respiratory distress syndrome, hypoglycemia and hyperbilirubinemia. In emergency cases, the fetus may suffer from injury syndrome – diabetic embryopathy.During pregnancy, due to hydramnios, a larger than an average fetus, urinary tract infections and preeclampsia can be noticed. Usually, in gestational diabetes, we deal with type-2 diabetes mellitus because the hormonal changes lead to insulin resistance in 3—5 % of females. In rare cases, the pregnancy may trigger a type-1 diabetes mellitus.
Symptoms of Diabetes Mellitus Type 3
All the forms of diabetes grouped under type 3 are not easy to observe in clinical practice. They are often diagnosed with type 1 or 2 diabetes, as the symptoms are similar. Which type of diabetes we exactly deal with can just be revealed with the help of specific diagnosis.Under WHO, all the forms which are not applicable to type 1, 2 and gestational diabetes refer to type-3 diabetes. According to different causes that occur with a rare frequency in diabetics, a total of eight groups can be distinguished. Therapeutic measures are similar to type 1, 2 and gestational diabetes.
Diabetes due to genetic defects in beta cells of the islets of Langerhans
This group is part of the so-called MODY diabetes (Maturity Onset Diabetes of the Young), which is caused by genetic defects in the glucose metabolism and occurs mainly in adolescence. These specific gene defects are monogenic autosomal dominant disorders. Eleven different forms of MODY diabetes have been specified so far:- MODY 1: mutation in chromosome 20, defect of the hepatic transcription factor HNF4A
- MODY 2: mutation in chromosome 7, defect in the enzyme glucokinase
- MODY 3: mutation in chromosome 12, defect of the hepatic transcription factor HNF1A
- MODY 4: mutation in chromosome 13, defect of PDX1
- MODY 5: mutation in chromosome 17, defect of the hepatic transcription factor TCF2
- MODY 6: mutation in chromosome 2, defect of NEUROD1
- MODY 7: mutation in chromosome 2, defect of KLF11
- MODY 8: mutation in chromosome 9, defect of CEL
- MODY 9: mutation in chromosome 7, defect of PAX4
- MODY 10: mutation in chromosome 11, defect of INS
- MODY 11: mutation in chromosome 8, defect of BLK
Diabetes due to genetic defects in insulin action
Two types have been distinguished in this group so far. They are both insulin-resistant by genetic defects. For type-A insulin resistance syndrome, there are typical disorders: hyperinsulinemia, skin disorder – acanthosis nigricans (hyperpigmentation and hyperkeratosis (cornification), mostly in groin and armpits) and hyperandrogenism in women. The Lawrence syndrome, or Lipodystrophy, is characterized by a massive reduction of subcutaneous fat, which is accompanied by insulin resistance out of the previously undiscovered reason.Diabetes as a result of a pancreatic disease
All the disorders of the exocrine pancreatic secretion, as a defect of the pancreas itself, or as a consequence of another disease, may lead to diabetes. Following disorders are included in this group:- Pancreatitis
- Trauma or pancreatectomy
- Pancreatic cancer
- Cystic fibrosis
- Hemochromatosis
Diabetes due to disturbed hormone production or regulation (Endocrinopathy)
Diabetes can occur as an accompanying disease in the case of the following hormonal imbalances:- Acromegaly (disturbance of the growth hormone somatotropin)
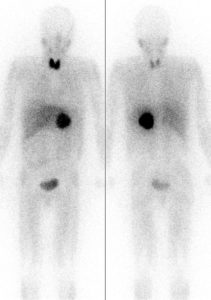 Image: “Body scintigraphy 24 hours after intravenous administration of 123Iod-MIBG. Physiological occupancy of the thyroid, liver and bladder. Pathological accumulation in a tumor of the left adrenal glands (pheochromocytoma). Left: from the front. Right: from behind,” by Drahreg01. License: CC BY-SA 3.0
Image: “Body scintigraphy 24 hours after intravenous administration of 123Iod-MIBG. Physiological occupancy of the thyroid, liver and bladder. Pathological accumulation in a tumor of the left adrenal glands (pheochromocytoma). Left: from the front. Right: from behind,” by Drahreg01. License: CC BY-SA 3.0 - Aldosteronoma (elevated aldosterone production);
- Glucagonoma (tumor which relates to A-cells of the islets of Langerhans)
- Hyperthyroidism (overactive thyroid)
- Cushing’s disease (increased ACTH production)
- Pheochromocytoma (tumors of the adrenal medulla)
- Somatostatinoma (tumor of the pancreas or duodenum, with increased somatostatin production)
Diabetes due to drugs or chemicals
Diabetes may occur as an adverse effect of certain drugs and chemicals, including:- Alpha interferon (for protection against viral diseases)
- Beta-adrenergic agonists (for stimulation of beta receptors of the sympathetic nervous system)
- Diazoxide (hyperglycemia)
- Glucocorticoids (against inflammations, overactive immune system, inflammatory rheumatic diseases)
- Nicotinic acid (for decreasing increased blood cholesterol)
- Pentamidine (antiprotozoal, commonly used in tropical medicine)
- Phenytoin (for epilepsy, cardiac arrhythmia)
- Thyroid hormones
- Thiazide diuretics
- Vacor (rat poison)
Diabetes due to viral infection
In congenital rubella, caused by the rubella virus, the islet cells of the pancreas may be destroyed. It results in the deficiency of insulin hormone leading to type-1 diabetes. The human cytomegalovirus (CMV) can also contribute to the development of diabetes, as pancreatitis may occur as the disease progresses.Diabetes due to immunological defects
In certain autoimmune diseases, such as stiff person syndrome (SPS), the endocrine glands may get harmed. This negatively influences the beta cells of the pancreas, resulting in type-1 diabetes. Other immunological defects that cause diabetes are the presence of anti-insulin receptor antibodies that block the insulin receptors of the cells, resulting in type-1 diabetes mellitus.Diabetes due to genetic disorders
Previously, diabetes was observed as a side effect with numerous genetic syndromes:- Huntington’s disease (HD)
- Down syndrome
- Myotonic dystrophy
- Friedreich’s ataxia
- Klinefelter’s syndrome (KS)
- Porphyria
- Prader-Willi-Labhart syndrome
- Turner syndrome
- Wolfram syndrome
Review Questions
The correct answers can be found below the references.1. Which of the following is a feature of diabetic ketoacidosis?
- Kussmaul breathing
- Hypoglycemia
- pH value > 7.65
- Sweating
- Anuria
- Hypoglycemia
- Increased risk of developing diabetes mellitus in children and adults
- Shoulder dystocia
- Respiratory distress syndrome
- Reduced birth weight
- Determination of HbA1c.
- Oral glucose tolerance test.
- Determining the amount of C-peptide in the blood.
- Determining the amount of glucose in urine.
- One-time measurement of fasting plasma glucose

ResponderEliminarGroundbreaking New Research Shows How to Reverse Type 2 Diabetes in 3 Weeks
Doctors at the International Council for Truth in Medicine are revealing the truth about diabetes that has been suppressed for over 21 years.
Last year they helped over 17,542 type 2 diabetics end the need for prescription drugs, insulin injections and blood sugar monitoring.
This year they're on track to help over 30,000.
In just a few weeks, 96% of their patients are able to stop ALL diabetes medication and insulin injections.
No more neuropathy pain, pricking your finger, or the need for expensive medication.
Learn about this groundbreaking new research here: [LINK]
Thank you for sharing that. For all we can do new researches and improve the quality of life of persons 😏
Eliminar