Perinatal Infections — Symptoms and Treatment
Table of Contents
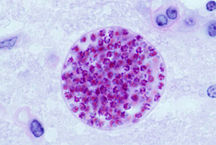
Microscopic cysts containing Toxoplasma gondii develop in the tissues of many vertebrates. Here, in mouse brain tissue, thousands of resting parasites (stained red) are enveloped by a thin parasite cyst wall.
Definition of Perinatal Infections
A bacterial or viral infection which is passed by the mother to her baby either during the pregnancy or during the delivery, or immediately after the delivery, is known as a perinatal infection (PN).
Etiology of Perinatal Infections
Perinatal infections, which can be transmitted vertically by the mother to her unborn fetus or baby include TORCH infections, listeriosis, human immunodeficiency virus infection (HIV), hepatitis B, hepatitis C, lymphocytic choriomeningitis virus (LCV), and enterovirus infections.
The transmission of the infection can occur transplacentally, hematogenously or during passage through the cervicovaginal birth canal. First trimester infections usually lead to miscarriages or fetal malformations, while infections later in pregnancy rarely cause fetal anomalies.
Clinical Presentation of Perinatal Infections
The common features of all perinatal infections are icterus, hepatosplenomegaly, fetal growth restriction and microcephaly. Features specific to individual infections are as follows:
Cytomegalovirus infection (CMV): In cases wherein the mother has a CMV infection prior to or during the first trimester, the fetus can develop blindness, hearing loss, mental retardation and epilepsy due to anomalous embryogenesis.
- Transmission: Body fluids such as urine, saliva, blood, tears, semen and breast milk.
- Diagnosis: PCR of amniotic fluid.
- Effect on fetus: Congenital hearing loss, vision loss, seizures.
- Treatment: None available during pregnancy.
Enterovirus infection can present in the neonatal period and is characterized by myocarditis, meningoencepahilitis, hepatitis and disseminated intravascular coagulation (DIC).
Genital herpes is caused by the herpes simplex virus type 2 (HSV-2) which causes painful genital sores. The infection can be transmitted to the baby during delivery if the mother has active genital sores. It can cause neonatal encephalitis, fever, seizures, keratoconjuctivitis, a vesicular rash and neonatal sepsis syndrome which has a high incidence of mortality and morbidity.
- Transmission: Sexual transmission via body fluids.
- Diagnosis: Serologic.
- Effect on fetus: Life-threatening CNS or death.
- Treatment: Antivirals.
Gonorrhoea leads to neonatal conjunctivitis and colonization of the upper respiratory tract and can be transmitted by the infected mother to her baby during labor.
Hepatitis B: Vertical transmission of the infection can occur due to exposure of the baby to infected maternal blood during delivery.
Picture: “HIV” by BruceBlaus. Lizenz: CC BY-SA 4.0
Human immunodeficiency virus (HIV): Vertical transmission of HIV from mother to the infant can result in babies developing HIV infection, AIDS and is associated with a high incidence of mortality.
- Transmission: Via contact through body fluids.
- Diagnosis: ELISA, Western blot.
- Effect on fetus: None.
- Treatment: HAART.
Listeriosis is a rare food-borne disease which can lead to fetal death or chronic intrauterine and perinatal infection.
Lymphocytic choriomeningitis virus (LCMV) infection is associated with hydrocephalus and chorioretinitis.
Parvovirus B19 infections cause hydrops fetalis and anemia.
Rubella: Antenatal maternal infection with rubella can lead to anomalies during embryogenesis with cardiac, ophthalmic, aural malformations and mental retardation. Specific features of congenital rubella are cataracts, glaucoma, chorioretinitis, “blueberry muffin” rash, pulmonary artery stenosis and patent ductal arteriosus.
- Transmission: Cough or sneeze.
- Diagnosis: Serologic.
- Effect on fetus: Congenital hearing loss, cataracts, “blueberry muffin” rash.
- Treatment: None available during pregnancy.
Group B streptococcus (GBS): Maternal GBS infection can cause premature labor and transmission to the baby can lead to neonatal meningitis, pneumonia and sepsis.
Syphilis infection can be transmitted transplacentally by the infected mother leading to premature labor, stillbirths or neonatal death. Infected babies may be born with severe malformations and those who survive infancy may develop symptoms of syphilis later.
Features specific to congenital syphilis include Hutchinson molars (blunt upper incisors with enamel hypoplasia), metaphyseal osteochondritis, periostitis, osteomyelitic lesions of the humerus and tibia, saber shins, hemolytic anemia, maculopapular rash on the palms, face and soles and bullous lesions on the palms and soles, snuffles (rhinitis), mucocutaneous lesions, interstitial keratitis, deafness, saddle nose deformity and palatal defects.
Image: “Micrograph showing Treponema pallidum, the spirochete that causes syphilis. Dieterle stain.” by Nephron – Own work. License: CC BY-SA 3.0
- Transmission: Sexual contact
- Diagnosis:
- Screening: RPR/VDRL.
- Confirmation: FT-Abs or dark-field microscopy.
- Effect on fetus: Hepatomegaly, CNS abnormalities, saddle nose, Hutchinson’s and FTA-ABS.
- Treatment: Penicillin.
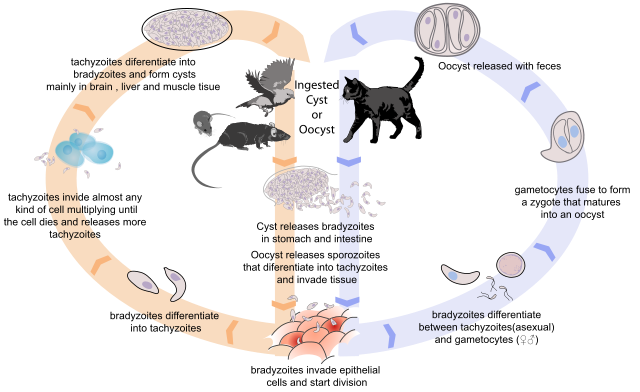
Toxoplasma infection leads to neonatal hydrocephalus with diffuse intracranial calcifications and isolated to late onset chorioretinitis.
- Transmission: Cat feces.
- Diagnosis: Serologic.
- Effect on fetus: Chorioretinitis, hydrocephalus.
- Treatment: Pyrimethamine (daraprim) and sulfadiazine.
Varicella causes scarring of the skin with atrophy of the limbs.
- Transmission: Respiratory.
- Diagnosis: Serologic.
- Effect on fetus: Chorioretinitis, encephalitis, muscle atrophy.
- Treatment: None.
Diagnosis of Perinatal Infections
Maternal workup
- Inquire about maternal history of exposure to sick children in day care (rubella and herpes can be transmitted by infected children), history of fever with rash (rubella), exposure to sexually transmitted diseases, multiple sexual contacts, intravenous drug usage and exposure to raw meat, soil and animals (toxoplasma).
- Antenatal screening with serology for TORCH titers, Venereal Disease Laboratory test (VDRL), HIV, rectovaginal swab for GBS.
- Amniotic fluid testing may be required to confirm fetal infection.
Neonatal workup
This should include the following tests, while additional tests can be performed based on the clinical presentation:
- Complete blood count, peripheral smear, reticulocyte count, platelet count.
- Liver function tests with bilirubin and transaminase levels.
- Toxoplasma IgM and IgG.
- Rubella IgM, rubella culture.
- Cytomegalovirus testing with urine culture if neonate is <2 weeks old.
- Parvovirus: Polymerase Chain Reaction (PCR) from blood sample.
- LCMV: Test IgM in the infant and IgG in the mother and the infant.
- HIV: HIV testing with PCR.
Treatment of Perinatal Infections
Depending on the stage of the gestation, extent of fetal anomalies, and fetal compromise, a decision may have to be taken regarding termination of pregnancy, inducing labor or cesarean section. Treatment specific to certain infections is mentioned below:
Image: “Micrograph showing the changes of herpes simplex virus (HSV). Pap test. Pap stain.” by Nephron – Own work. License: CC BY-SA 3.0
- Chlamydia: Maternal infection can be treated in the third trimester with oral erythromycin, while neonatal infection can be treated at birth with erythromycin suspension.
- Cytomegalovirus: Currently, there are no medicines or vaccines to either treat or prevent CMV infection.
- Genital herpes: Antenatally, the mother can be prescribed antiviral drugs like acyclovir or famcicyclovir, while acyclovir can be administered to infants with suspected HSV-2. Cesarean section is the preferred mode of delivery in cases where the mother has active genital herpes.
- Hepatitis B: All infants should receive the hepatitis B vaccine at birth as part of the routine immunization schedule. In addition, babies born to mothers who are HbsAg positive should receive hepatitis B immune globulin at birth.
- Hepatitis C (HCV) infection: Currently, there is no immunoprophylaxis for HCV and breast feeding is not contraindicated as HCV RNA and HCV antibodies have been detected in the breast milk of infected mothers.
- Human immunodeficiency infection: All pregnant women with HIV should be treated with retroviral drugs during pregnancy and should be counseled against breast feeding their infants to avoid vertical transmission of the infection. Babies born with HIV should be treated aggressively with retroviral drugs to prevent the development of AIDS.
- Human papillomavirus: Maternal genital warts can be treated antenatally with cryotherapy, laser, electrocautery or surgical excision and cesarean section is the preferred mode of delivering babies in the presence of maternal genital warts.
- Rubella: Ideally, women with no previous history of exposure to rubella should receive the rubella vaccine immediately after their first pregnancy. There is no treatment for rubella and pregnancy termination should be considered on a case-by-case basis.
- Streptococcus (GBS): Maternal GBS bacteriuria of any significance or a positive rectovaginal swab at 35-37 weeks is an indication for chemoprophylaxis. Intravenous antibioticprophylaxis is administered in all women with a positive GBS status and it is also administered to women with unknown status during premature labor pending results of the rectovaginal swab. Neonates suspected to be infected or with symptoms are also treated with antibiotics.
- Syphilis: Penicillin is the antibiotic of choice in the antenatal period if the mother is suspected to have syphilis. If given in the first trimester, vertical transmission of the infection to the fetus can be prevented.
Prognosis of Perinatal Infections
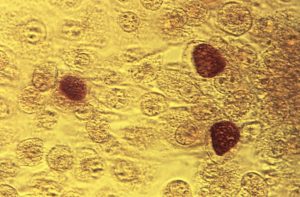
Image: “This photomicrograph reveals McCoy cell monolayers with Chlamydia trachomatis inclusion bodies; Magnified 200X. ” by CDC/Dr. E. Arum; Dr. N. Jacobs – This media comes from the Centers for Disease Control and Prevention’s Public Health Image Library (PHIL), with identification number #3802. License: Public Domain
Adverse outcomes can be prevented by antenatal screening and counseling.
- Chlamydia infection is associated with premature delivery in untreated cases and infected neonates usually recover with antibiotic treatment.
- Cytomegalovirus: Lifelong sequelae can be expected in neonates born with CMV infection and the infection can be life-threatening if there is concomitant HIV/AIDS.
- Genital herpes: Once infected, genital herpes can recur anytime during the lifetime of the baby.
- Hepatitis B: Neonates treated with hepatitis B immunoglobulin and vaccination are protected from the infection, but babies infected with hepatitis B can develop chronic hepatitis and have a higher risk of developing chronic liver disease.
- Human immunodeficiency virus: Antenatal treatment with retroviral drugs decreases the risk of vertical transmission and the infant can be protected. Avoiding breast feeding also prevents the baby from getting infected.
- Human papillomavirus: If infected with HPV, the infant has a lifelong risk of developing warts and some types of malignancies.
- Rubella: Intrauterine rubella infection is associated with a high incidence of cardiac anomalies, cataracts and deafness.
- GBS infection is associated with a high risk of premature labor and life-threatening GBS meningitis and sepsis in the neonate. If the baby recovers, it may still develop sequelae and neurological deficits.
- Syphilis: Untreated pregnant women with syphilis are at a high risk for premature labor and their babies may be stillborn or may be born with birth defects discussed above.
Prevention of Perinatal Infections
Multiple sexual partners and intravenous drug use are the most important risk factors for PNs. Pre-pregnancy and antenatal counseling about barrier contraception, antenatal maternal screening and nutritional support can help in the prevention of these infections.


Este comentário foi removido por um gestor do blogue.
ResponderEliminar